Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Cirugía paraguaya
On-line version ISSN 2307-0420
Cir. parag. vol.47 no.1 Asunción Apr. 2023
https://doi.org/10.18004/sopaci.2023.abril.30
Case report
Late presentation of isolated gallbladder perforation due to penetrating abdominal trauma. Case Report
1Hospital Central del Instituto de Previsión Social. Asunción, Paraguay.
Isolated gallbladder perforation due to penetrating abdominal trauma is a rare event due to its anatomical location. The signs and symptoms suggestive of choleperitoneum may not be obvious within the first few hours following the event. This is the case of a 26-year-old man with penetrating abdominal trauma due to bladed weapon used by some individual with isolated gallbladder perforation.
La perforación vesicular aislada posterior a un traumatismo penetrante de abdomen es un evento infrecuente debido a la situación anatómica de la misma. Los signos y síntomas de un coleperitoneo pueden no ser evidentes en las primeras horas a días del evento. Este es el caso de un paciente de 26 años que, tras traumatismo abdominal por arma blanca por agresión de terceros, presenta perforación aislada de la vesícula biliar.
Palabras clave: perforación vesicular; peritonitis biliar; traumatismo penetrante de abdomen
INTRODUCTION
Due to the anatomical situation of extrahepatic bile ducts, damage to these organs has a low incidence rate and are a rare entity. In 95% of the cases the cause is attributed to iatrogenic causes while only 5% is attributed to trauma. In addition, these lesions often occur at the following anatomical locations: gallbladder (3% to 5%) and bile ducts (0.5% of the cases)1.
Bile duct injury is rare even in large reference centers. In their study, Ball et al. found 45 gallbladder lesions (0.11%) in 40 000 patients. This is, mainly, due to the fact that the gallbladder is surrounded by organs and structures like liver, colon and intestines, greater omentum, and thorax that protect it from any aggressions. It is precisely for that same reason that trauma to the gallbladder is associated with other lesions to the abdominal cavity. The most common cause of gallbladder trauma is penetrating wounds due to bladed weapon or firearm (89%) followed by closed abdominal trauma (remaining 11%)2.
The management of trauma injuries to the gallbladder is often cholecystectomy. In patients with bile duct injuries, mortality is associated with other lesions like cardiac, thoracic lesions or intra-abdominal bleeding, multi-organ failure and/or traumatic brain injuries. The prognosis of isolated bile duct injuries is often promising (3) .
CASE REPORT
This is the case of a 26-year-old man without any known underlying conditions who is a sporadic user of psicoactive substances, occasional drinker, and has no past surgical history. He says that 72 hours prior to admission he was hurt by someone with a bladed weapon. As a result, he was stabbed in the right hypochondriac region in the context of a fight resulting in pain to the region surrounding the wound. After seeking medical attention, he is administered analgesic drugs and admitted to the hospital under observation since the lesion looked superficial and had not reached the fascia. A few hours later, he is discharged and asked to remain alert.
Six hours prior to admission, the patient presented with insidious abdominal onset pain wrongfully located at the epigastrium radiating to the right hypochondrium that did not subside with common analgesic drugs, and no nausea or vomiting. He decides to go to the emergency room. He walks to the ER, and is admitted showing a general state of good health, remains hemodynamically stable, and with good respiratory mechanics. The physical examination revealed the presence of an asymmetrical abdomen, and a 1 cm cutting lesion in the right hypochondriac region that was covered with a sterile gauze. The abdomen was soft and depressible at palpation. Also, slightly painful at deep-not superficial-palpation in the perilesional region without muscular defense, but with signs of peritoneal irritation.
Parenteral hydration was indicated. Routine lab tests were performed giving the following results: white blood cell count of 14 400/uL, 82% neutrophils; hemoglobin, 14.8 g/dL; platelets, 284 000/uL; total bilirubin, 0.85 mg/dL; alkaline phosphatase, 69 µ/L; GPT, 26 u/L; GOT, 52 u/L. The abdominal ultrasound performed revealed “the presence of a gallbladder with 20 mm thick walls of irregular appearance in its entirety. Also, the presence -at the bottom and posterior wall level-of a 26 mm x 18 mm predominantly echogenic heterogenous formation of immobile lobulated borders with scarce vascular signal in the color Doppler ultrasound . A targeted study of this region is suggested for better lesion characterization that ends up revealing the presence of free fluid in the right parietocolic space and pouch of Douglas in moderate amount.” Following these findings, a simple abdominal and pelvic CT scan was performed that revealed the presence of multi-compartment free fluid, and a thickened bile duct with heterogeneous appearance in the gallbladder lumen. (See Figure 1).
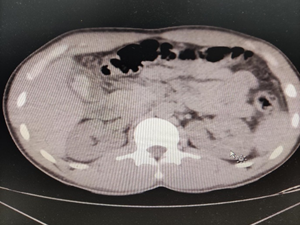
Figure 1. Simple abdominal CT scan. Presence of free fluid and hyperdense image in the gallbladder lumen.
Following this finding, surgery was suggested. The exploratory laparotomy revealed the presence of 500 cc of bile fluid distributed across the entire abdominal cavity, omental loose adhesions to the thin-walled gallbladder that had perforated in the gallbladder fundus with bile content, and blood clots inside. Also, the cystic duct was long and thin, and the ductus choledochus seemed to have a preserved caliber (see Figure 2). The remaining organs inside the cavity looked normal with no specific findings. Neck cholecystectomy and abdominal washout were performed. After surgery, the patient was transferred to the hospital ward where disease progression was favorable. Twenty-four hours after surgery he was put on antibiotic therapy that covered the abdominal focus with a course of ciprofloxacin/metronidazole. Seventy-two hours after surgery the patient was discharged from the hospital.
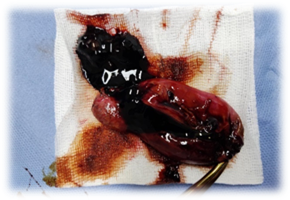
Figure 2. Exploratory laparotomy showing the choleperitoneum, and the perforation of gallbladder fundus.
Results from pathological anatomy reveal the presence of acute cholecystitis with extensive transmural necrosis, and peritoneal reaction.
DISCUSSION
Bile duct injuries in abdominal trauma are a rare entity often associated with damage to other organs. Isolated gallbladder perforation due to penetrating abdominal trauma is rare because of the anatomical protection it has. Its overall incidence rate goes from 0.8% to 2.1% in patients with some type of abdominal trauma4.
The presence of sterile bile in the peritoneal cavity causes discrete irritation, which would explain the slow progression of the disease5,6.. The diagnosis of gallbladder perforation is confirmed with exploratory laparotomy being more severe damage to the organs overlapped to it. When the abdomen is not examined, there can be a period from 1 to 6 weeks during which peritoneal disease can occur as it happened in this case. Cholecystectomy is the treatment of choice for gallbladder rupture after abdominal trauma. Laparoscopic approach is an effective and safe way to treat gallbladder traumas7. However, in this case, due to diagnostic uncertainty, exploratory laparoscopy was considered the safest option between the two.
REFERENCES
1. Trauma de vesícula biliar por traumatismo penetrante de abdomen por herida de arma blanca, reporte de caso. [Internet]. Revista SACD. 2021 [citado 12 de agosto de 2021]. Disponible en: Disponible en: http://revista.sacd.org.ar/trauma-de-vesicula-biliar-por-traumatismo-penetrante-de-abdomen-por-herida-de-arma-blanca-reporte-de-caso/ [ Links ]
2. Beltrán S MA, Rodríguez V FJ, Hevia M JA, Zaffiri M VR, Beltrán C AA, Beltrán S MA, et al. Perforación traumática aislada de la vesícula biliar. Revisión de la literatura actual con reporte de un caso. Rev Cir. febrero de 2020;72(1):76-81. [ Links ]
3. Kwan BYM, Plantinga P, Ross I. Isolated traumatic rupture of the gallbladder. Radiol Case Rep. 1 de enero de 2015;10(1):1029. [ Links ]
4. Epstein MG, Silva DL da, Elias NC, Sica GTA, Fávaro M de L, Ribeiro Junior MAF. Isolated rupture of the gallbladder following blunt abdominal trauma: case report. Einstein São Paulo. junio de 2013;11(2):227-8. [ Links ]
5. Izzo L, Gabriele R, Conte M, Di Cello P, Pugliese F, Merlini G, et al. Severity in biliary peritonitis. Il G Chir. mayo de 2012;33(5):168-71. [ Links ]
6. Andersson R, Tranberg KG, Bengmark S. Roles of bile and bacteria in biliary peritonitis. Br J Surg. enero de 1990;77(1):36-9. [ Links ]
7. Egawa N, Ueda J, Hiraki M, Ide T, Inoue S, Sakamoto Y, et al. Traumatic Gallbladder Rupture Treated by Laparoscopic Cholecystectomy. Case Rep Gastroenterol. 2016; 10(2): 212-7. [ Links ]
Authors’ contributions: All the authors share responsibility for the idea, design, and drafting of this manuscript, as well as for the bibliographic search conducted, and the manuscript final review.
Received: November 25, 2022; Accepted: February 03, 2023











 text in
text in 




