Introduction
Astigmatism is a refractive defect of the eye in which there is a different refractive power in different meridians, which prevents a specific image from being formed on the retina from a specific object1,2. It occurs on a surface whose curvature progresses from a minimum value to a maximum value in perpendicular meridians so that the rays do not suffer the same deviation in all meridians1. Instead of a single focal point, two focal lines are separated from each other by an interval whose length is directly proportional to the difference in power between the two principal meridians. Irregular astigmatism is caused by corneal pathologies such as keratoconus; post-transplant, post-refractive surgery, or corneal degeneration produce poor visual acuity that cannot be corrected with aerial lenses3, which could only be corrected with a surgical procedure or simply with the use of special contact lenses4,5.
Scleral contact lenses (SCL) are gas permeable and are placed entirely on the sclera without contacting structures, such as the cornea or limbus6. They are large in size, with diameters that vary between 15 and 20 mm, centering independent of irregularity, a wide optical zone to achieve greater stability of visual acuity in addition to the optical field. One can find formulas that exceed ± 40.00 diopters. They are designed to locate a thin layer of aqueous liquid above the ocular extension, without allowing air bubbles or foreign bodies to enter the thickness. They are currently manufactured with high oxygen permeability, and there are, for example: Itafluorfocon B Dk 127X10¹¹, Equalens II, DK = 110 × 10¹¹7,8. These ECLs are designed to rehabilitate reduced vision in eyes with irregular corneas that are intolerant to rigid contact lenses7-9. Its reserve fluid functions as a dressing fluid that offers unique therapeutic benefits to the ocular surface. This deposit protects the surface from desiccation and the effects of exposure to air, and acts as a barrier between the cornea and eyelid, significantly reducing the intensity of pain and ocular photophobia, facilitating the healing of persistent epithelial defects, promoting corneal health, and maintaining hydration of the area. Currently, with the appearance of scleral contact lenses, they could be a therapeutic option for the treatment and optical correction of corneal pathologies10-12 to improve visual acuity (VA) in these patients.
Methods
This was a retrospective, cross-sectional, descriptive observational study. This study was conducted in accordance with the standards of the Declaration of Helsinki and its subsequent revisions. No distinction between sex, religion, or politics was made in the inclusion and analysis of the data. Population: Patients diagnosed with irregular astigmatism who could not be fitted with rigid gas-permeable contact lenses within a time frame from March 2019 to March 2021. Non-probabilistic sampling of consecutive cases. Patients of both sexes, of all ages, with a diagnosis of irregular astigmatism who could not be fitted with rigid gas-permeable contact lenses, and who had attended the Fundación Oca del Valle Eye Bank during the research period were included. To calculate the necessary sample size, a prevalence of 2% of patients who could require adaptation of scleral lenses was considered; for a 90% CI and a margin of error of 5%, 20 patients would be required, which would correspond to 40 eyes, for the calculation the Epilnfo 7.2.2.2 statistical package was used. The data were recorded in an Excel 2022 electronic spreadsheet with the variables included in the study and subsequently analyzed using the SPSS program. The results were expressed as frequencies, percentages, means, and standard deviations.
Results
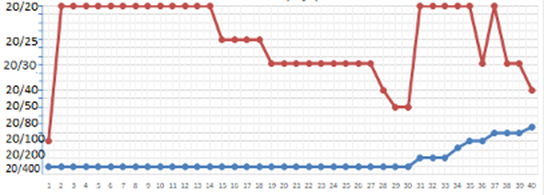
Forty cases of irregular astigmatism with different initial effects on visual acuity before lens placement. The mean visual acuity (VA) prior to correction with scleral lenses observed in the 40 cases was 20/200 with correction (CC) on the Snellen scale with a minimum (worst VA) equal to “finger-counting vision” (represented as cases with 20/400 vision for quantification purposes), and a maximum (best VA) of 20/70. After scleral lens placement, a mean VA of 20/25 was observed in the study population, with a minimum of 20/100 and a maximum of 20/20. An improvement in the mean VA from the state prior to lens placement of about 13.21 times on average (minimum improvement of 1.78 times and maximum of 20 times) to the post-lens placement state is estimated, considering the total study population.
The individual variations in each case are shown in Figure 1. Nineteen cases (47.5%) restored their VA to normal values (20/20), and 30 cases (75%) improved their VA by at least 10 times compared with the initial value.
The mean age of the studied sample was 44.15 years ± 17 SD, with a median age of 40 years and range from 20 to 84 years. 29 cases corresponding to the male sex and 11 to the female sex were studied. In the female population, the mean age found was 44.9 years ± 17.1 SD while in the male population it was 43.86 years ± 17.3 SD. The minimum age for females was 20 years and 22 years for males, with a maximum age of 66 years for females and 84 years for males.
Regarding etiologies, 26 cases of keratoconus (65%), 8 postoperative cases of penetrating keratoplasty (20%), 5 postoperative cases of refractive surgery (13%), and 1 case of Terrien's degeneration (2%) were observed.
The 40 cases were divided into three groups according to the percentage of VA decrease with respect to the normal value of 20/20. In the three groups, according to the percentage of VA loss with respect to the normal value of 20/20. The means of the three groups are presented in Table 1, along with the new mean post-placement VA values.
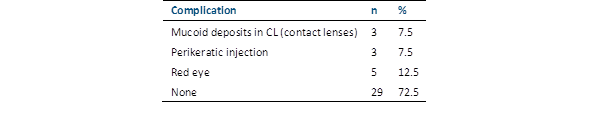
It was found that the group with VA loss greater than 90% benefited about 15.76 times on mean compared to the original value, while the group with VA loss between 80% and 90% benefited about 7.425 times compared to the original value, and the group with VA loss between 50 and 79% improved their visual acuity value by a mean of approximately 2.76 times. Complications and their frequencies of occurrence are shown in Table 2.
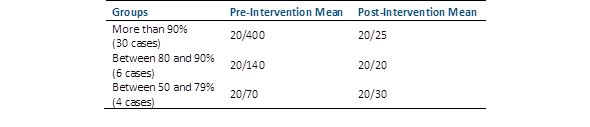
TABLE 1 MEAN VALUES OF VISUAL ACUITY (VA) ACCORDING TO THE SNELLEN SCALE BEFORE AND AFTER THE USE OF SCLERAL LENSES (N=40).
Discussion
The use of LCE for the treatment of corneal irregularities, uncomplicated refractive errors, and ocular surface diseases has increased11,12. The placement of LCE improved the VA in the 40 cases studied by a mean of 13.21 times compared to the state prior to adaptation to them and was expressed in values of the Snellen scale, with an mean VA of 20/ 200 to the best mean value of 20/25. Approximately half of the cases had their VA restored to normal values (20/20). Regarding correction values, similar findings can be observed in the work of Escamilla from 20107 where the majority of patients reached visual acuity values close to 20/50, 20/30 or even 20/20, although This study is focused on those after refractive surgery; In the present study, the cases associated with it were a total of 5. Most cases were derived from keratoconus13,14, which is consistent with the findings of other studies.
The mean age of the patients who required study intervention was 44.15 years with a standard deviation of 17 years. A normal age distribution was observed. Most patients were male (72%). A similar distribution of ages was found considering each sex separately (mean, median age, and SD in both groups were similar and approximate to that of the population).
Most cases (26 cases, 65%) required the placement of lenses due to keratoconus, followed by other causes, such as postoperative penetrating keratoplasty (PKP) (8 cases, 20%), postoperative refractive surgery (5 cases, 13%), and tertile degeneration (1 case, 2%).
Most patients (72.5%) did not present with complications after lens application. The most frequently observed complication was red eye (12.5% of the 40 cases), followed by perikeratic injection and mucoid deposits (7.5% each), similar to the reported frequencies15,16. Depending on the reason for needing the intervention under study, keratoconus cases had a greater probability of developing complications (30.77% of cases). Most episodes of ocular redness were recorded in patients who underwent penetrating keratoplasty. In both sexes, the most frequent complication was absence of complications. However, among the complications reported, in terms of proportion, the most common complication was eye redness, whereas in female patients, the most prevalent complication was the presence of deposited mucoids in the contact lenses.
From a physiological perspective, it has been established that the irregularity of corneal astigmatism in the context of typical human eyes increases as the aging process progresses, but it can also be induced by corneal surface pathologies and ophthalmological surgeries17-19.
The improvement in VA observed in the present study showed a high and constant value for all patients studied. The finding of an increase of up to 20 times its initial value prior to the application of the lens, and in many cases, the resolution at Snell scale values of 20/20, shows a promising treatment with relatively few adverse effects according to the present findings. In fact, out of every 4 eyes, in 3 of them no type of obvious complications were found at the time of the post-placement re-evaluation. It will be pertinent to carry out a corresponding follow-up of these patients to evaluate the progression of the pathology that led them to this intervention and the potential presence of complications that may be found. The high number of elevated patients who underwent evaluation, their demographic homogeneity, and the consistent results of improved visual acuity observed are cited as important points. Some points to consider for future work would be to consider a longer follow-up time and the inclusion of additional keratometric tests associated with the state of visual acuity.