Introduction
Traumatic brain injury (TBI) caused by accidental events affects approximately 3 million children annually and is the main cause of sequelae in the pediatric population worldwide1,2. In Mexico, around 6% of cases are caused by childhood accidents, of which 30% require care in pediatric emergency services3.
In the United States of America, 80% of head traumas are considered mild, of which 70-80% go to emergency services to receive assistance, in contrast to severe head traumas that contribute to between 3-7% of cases1,4. In a study carried out during the year 2001 at the "Roberto Rodríguez" general hospital in Morón, Ciego de Àvila, Cuba, of the 339 pediatric cases that requested medical attention in the emergency service, 97.05% presented a mild TBI, 2.36% were moderate and 0.59% severe5.
In head injuries at any age, different types of damage to the brain tissue can occur, which are generated by different pathophysiological mechanisms. Primary brain damage is caused by the transfer of kinetic energy to the parenchyma owing to direct trauma to the head. Secondary damage is produced by the effect of several factors that act in minutes or hours on the brain6. These factors include hypoxia, arterial hypotension, hyperthermia, hypo or hypernatremia, hypo or hyperglycemia and intracranial hypertension (ICH)6. Tertiary damage is generated as a consequence of injuries caused by care and health care, and quaternary damage appears in the subacute and chronic phases when the cell damage process appears to have ceased and generates tissue loss, adding injuries to the primary damage7.
One of the main objectives of TBI management is the prevention of hypoxia and arterial hypotension. It is known that an episode of arterial hypotension is related to a doubling of mortality and an increase in morbidity in patients with severe traumatic brain injury (sTBI)8.
Prevention of factors that trigger secondary damage, such as hypotension and hypoxia, is of great significance to avoid the development of cerebral edema and ICH, a phenomenon that can have a negative impact on the results if it is not controlled in the first hours of treatment. Once the trauma has occurred, therefore, efficient care, continuous and in stages, must begin at the site of the event and continue until the secondary level, in the reference centers for the treatment of traumatic brain injury TBI9.
Appropriate treatment of patients with polytrauma is associated with decreased mortality and sequelae in all age groups. The speed and efficiency with which each of the damage control measures are adopted during the patient's "golden hour" will favor the final results9. This study aimed to evaluate the influence of prehospital variables on intracranial pressure (ICP) and outcomes in pediatric patients with sTBI.
Methods
A descriptive study was carried out with 41 patients between 1 month and 17 years, 11 months and 29 days, who were received in the emergency department (ED) and who were admitted to the pediatric intensive care unit (PICU) of the "Roberto Rodríguez Fernandez" General Teaching Hospital for a sTBI, between January 2003 and December 2018.
The inclusion criteria were as follows: pediatric patients with sTBI admitted to the PICU. Exclusion criteria: Other types of TBI, need for transfer to another hospital due to the presence of associated injuries, death in the ED, death in the operating room (OR), or death during transfer.
Patients with sTBI were treated at polyclinics, municipal, or provincial hospitals, and were transferred through the integrated medical emergency system (IMES) to the neurotrauma center. In some cases, the transfer was performed by the child's relatives. Transport used: Sanitary through the IMES or private means.
After evaluation and stabilization in the ED, a general physical examination and imaging studies were performed. All patients underwent surgery to place an external ventricular drain (EVD), with double objective, continuous monitoring of ICP and cerebral perfusion pressure (CPP), and drainage of cerebrospinal fluid (CSF) in patients with ICH. Upon arrival at the PICU, ICP was monitored using a liquid column system connected to a transducer that converted the pressure of the liquid column into an electrical signal displayed through a LifeScope or Doctus VII monitor.
Variables: Time elapsed between head trauma and reception in the neurotrauma center: It is subdivided into 0-3 hours, 4-6 hours and-7-12 hours. The age groups were divided into under one year old, 1 to 4 years, and 5 to 17 years. The clinical conditions on arrival at the neurotrauma center include endotracheal intubation, hemodynamic stability, and hypoxia.
Prehospital therapeutic measures: These were divided according to the needs of the patients in relation to the use of 0.9% saline solution, vasoactive drugs, aspiration of secretions, endotracheal intubation, hyperosmolar therapy, anticonvulsants, sedatives, and other therapeutic measures. All patients underwent surgery to evacuate intracranial space-occupying lesions (SOL), decompressive craniectomy (DC) or EVD placement.
ICP values were distributed according to the age groups in the following treatment thresholds10: Under one year: 6 mmHg, from 1 to-4 years: 10 mmHg, from 5 to17 years:15 mmHg. To establish treatment, elevated ICP above the values indicated for 15 min for each age group was considered.
Mean arterial pressure (MAP): A sphygmomanometer was used according to age and was calculated using formula 2 (diastolic BP + systolic BP)/3. Considering hypotension, the MAP was below the 5th percentile for each pediatric age group. The results were evaluated by the tables established for each age group11.
Hypoxemia was considered when oxygen saturation (SaO2) values determined by pulse oximetry were below 90%. The Glasgow Outcome Scale (GOS) was evaluated at discharge and included grades I (death), II (persistent vegetative state), III (severe sequelae), IV (moderate sequelae), and V (slight sequelae or no sequelae).
The data were collected in a data notebook that included different variables; later, they were poured into a database made up of the statistical system SPSS version 20.0, using the chi-square goodness of fit test, Pearson correlation coefficient, and Mann-Whitney U test. The results are presented in tables and graphs for a better understanding.
Results
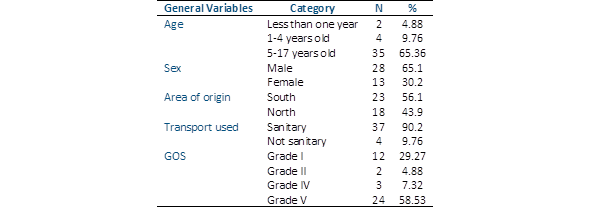
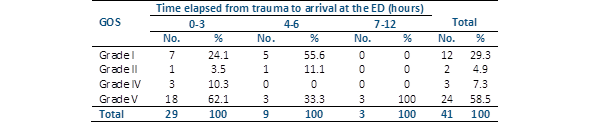
Children between 5 and 17 years of age predominated with 35 cases (85.36%), the largest number belonging to the provincial southern zone with 23 patients (56.1%) and 37 (90.2%), were transferred through the IMES (Table 1). The time elapsed from trauma to arrival at the ED of the neurotrauma center was 0-3 hours in 29 children (70.7%) (p<0.001), 4-6 hours in 9 (22%) and 7-12 hours in 3 (7.3%). By relating the time elapsed from the trauma to arrival at the ED with the results, we found that of the 24 children in grade V of the GOS, 18 (75%) arrived at the hospital between 0 and 3 hours, while of the 12 deceased, 7 (58.33%) were transferred in the same time, showing no statistical differences (Table 2).
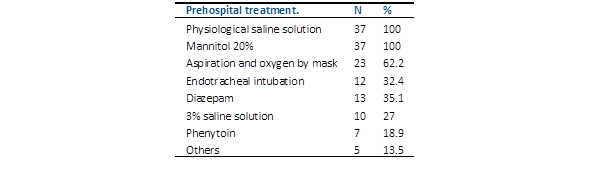
Among the prehospital medical treatments applied in the cases transferred by the IMES (n=37), 0.9% saline solution and mannitol 20% were used in all cases (100%) (Table 3). The clinical conditions of the 41 patients who arrived at the neurotrauma center had the following characteristics: hemodynamically stable, 26 patients (63.4%) (p<0.001); expedited airway, 14 (34.1%) (p<0.05); without an expedited airway, 27 (65.9%) (p<0.05); and hypovolemic shock, 15 (36.6%) (p=0.086).
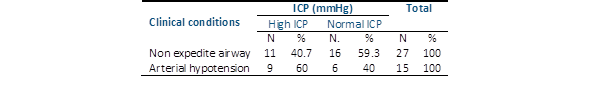
On physical examination in the ED, arterial hypotension was diagnosed in 15 cases (36.6%) and hypoxemia in 27 cases (65.85%), all without an expedited airway. The 27 patients who did not have an expedited airway underwent endotracheal intubation; four had the tube repositioned, and another two the tube changed. The relationship between hypoxemia, arterial hypotension at admission, and ICP behavior is shown in Table 4. Hypoxia on admission present in 27 children, was related to increased ICP in 11 (40.7%) and normal ICP in 16 (59.3%) children.
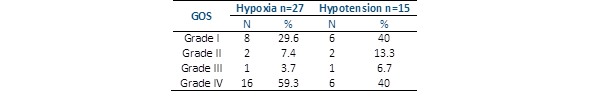
Hypotension in 15 children was associated with elevated ICP in 9 (60%) and normal ICP in 6 (40%).Of the 12 children who died (29.27%), 8 (29.6%) were exposed to hypoxia because of the non-expedited airway, and 6 (40%) were exposed to hypotension. Of the 24 patients with grade V (mild sequelae or no sequelae), 16 (59.3%) presented hypoxia related to a non-expedited airway, and 8 suffered from hypotension (40%) (Table 5).
Discussion
In the present study, a high frequency of sTBI occurred in pediatric patients aged between 5 and 17 years (85.36%), with a mean of 10.08 ± 4.95 was significant. We know that the little children their parents take care of them and spend most of their time at home; the same is not true for older children as those over 5 years old and much less with adolescents. In these last two age groups, the care of those responsible is reduced, which explains why they are more exposed to traumatic events.
Some authors report children older than 5 years as the most affected with sTBI, such as Sarnaik et al. (mean age 9.2 years)12 Vavilala et al. (mean age 7.5)13 and Kayhanian et al. (mean age 9.4 years)14) which agrees with our results. However, Chaitanya et al15 obtained a mean age of 5.5 years, which is different from that found in our study. The highest percentage of patients came from the most populated southern area of the province, in which the main municipality was located. In this area, there is a central highway and a central railway line with abundant traffic where most accidents occur.
As there is an ISME, which directs the transfer of patients in health facilities, the transfer of the largest number of cases was carried out by this route, data that correspond to other studies, where health systems are used to transportation of sTBI patients16. Regarding the time elapsed between the trauma and arrival at the neurotrauma center, it was significant that more than half of the patients (70.7%) (p≤ 0.001) arrived in the first 3 hours of evolution, which shows the efficiency of ISME for the transfer of patients in the shortest possible time. Álvarez et al. reported a transfer time of 4-6h in 82.6% in their series, which differs from our results17.
In reference to this topic, Labrada et al.16 suggest that the reduction in the time of transfer and the beginning of the treatment until final admission to the PICU is an important factor to consider in order to improve survival. These authors observed a trend towards higher mortality in patients with longer transfer times. Newgard et al.18 based on a multivariate analysis found that there is no relationship between transfer time and mortality, while other authors suggest that it is not the response time that influences the results, but rather the severity of the injuries19.
The authors of the present study agree that the transfer time in the best possible clinical conditions of the patients, as well as the magnitude of the injuries, influence the final result of pediatric patients with sTBI. It is important to note that the therapeutic measures adopted during the first hour of evolution in patients with sTBI can have a great influence on the final result, therefore this period of time has been called "golden hour" by many researchers. In the opinion of the authors, among the necessary measures mentioned previously, such as the prevention of hypoxia and arterial hypotension, one of the most important may be the control of the possible elevation of ICP.
Álvarez et al.17 found that a considerable number of their cases were treated with associated secondary injury, which was fundamentally represented by certain degrees of hypoxia and hypovolemic arterial hypotension, in agreement with the findings of our study. There is a lot of evidence to support the relationship between good results and early surgical evacuation of intracranial SOL that produce a mass effect or pressure cones associated with brain herniations20.
Today, it is accepted that the intracranial cavity is a compartmentalized space due to the existence of dural divisions, such as the falx cerebri and tentorium cerebelli, which divide it into compartments that do not express the same ICP values, so that any diffuse or focal SOL can produce an "intracranial compartment syndrome", in which pressure cones are transmitted from one compartment to another and can even produce ischemic damage to the brain stem21.
From the foregoing, it can be suspected that early management can be of great significance in the treatment of these patients if it is considered that some therapeutic measures used to control ICH have a greater impact on the results when applied at the appropriate time of evolution, which may also have a preventive effect on the development of the feared secondary damage, associated with exposure of the brain to prolonged periods of ICH, a criterion that other authors have considered22.
The primary evaluation of pediatric patients begins at the scene of the accident or where the trauma occurs23, with a comprehensive examination and state of consciousness. The main priority is to guarantee optimal airway and shock control, that justifies the justification that all patients with sTBI should be considered for endotracheal intubation (ETI). In the group of patients studied, only 34.1% (14 of 41 children) underwent ETI, despite the fact that 90.2% were transferred by the MIES, with personnel trained in polytraumatized patient care. This behavior led to the fact that 65.9% of the patients arrived without an open airway, which suggests that they could have been exposed to oxygen desaturation events at some point.
These results do not differ from those found in the scarce literature available on the subject of ventilation of children with sTBI in the prehospital phase, since there is sufficient evidence that hypoxemia occurs in the greatest number of occasions in this phase24. At present, there are no studies with an adequate design to evaluate the role of some maneuvers on the airway in these cases in the prehospital stage. On the other hand, it is very important to know that these maneuvers, and specifically ETI, can represent a significant risk of increased ICP, bronchial aspiration, and hypoxia, if the procedure is not performed with the required professional level25.
The CENTER-TBI26 Pan-European multicenter study reported the risk of developing hypoxia and arterial hypotension in patients with sTBI. In addition, it states that the performance of ETI maneuvers and venous cannulation delays the time of arrival at the secondary care center because of the delay in the stabilization of cases. This aspect is clearly influenced by the distance between the accident site and the neurotrauma care center as well as the accessibility and technological availability of the country to the optimal medical transfer where the event occurs. This study also refers to the fact that prehospital care has improved in recent years due to the widespread use of supplemental oxygen, ETI and volume resuscitation.
The prehospital evaluation of the patient with sTBI by an anesthesiologist who participates in resuscitation and ETI using pulse oximetry together with a short time transfer, is associated with lower mortality and sequelae27.
According to Spaite et al.28 the presence of hypoxia and arterial hypotension in patients with sTBI increases mortality. In their study, both factors contributed 43.9% of deaths, as reported by Carreón González29. Alberto et al.30) proposes a relationship between unfavorable results and events of respiratory depression, hypoxia, and arterial hypotension, increasing mortality with these last two events together up to three times in relation to each phenomenon separately.
As mentioned previously, the injured brain is extremely sensitive to secondary damage, mainly due to events of hypoxia and arterial hypotension. According to Manley et al.31) 48% of the patients in their study were exposed to more than one episode of hypoxia or arterial hypotension, and in 14% both episodes coexisted, increasing the mortality of an episode of arterial hypotension (mortality 53%) to 3 events (100% mortality) (p<0.05)31.
The drop in MAP in children with sTBI, could be related with associated injuries, spinal cord shock, hypovolemic shock and/or the use of hyperosmolar drugs, causes a decrease in CPP, with failures in the autoregulation of cerebral blood flow, ischemia and increase of ICP3, it is also known that in these children, despite intensive medical-surgical treatment, intermittent events of ICH of variable duration occur, which increase mortality32.
In the present study we were able to observe that a considerable number of patients were exposed to events of hypotension, shock, non-expedited airway and hypoxemia, some of them with unfavorable results (grade I and II of the GOS), which shows the close relationship between hypotensive events and worse results; however, those who presented good results were also exposed to these phenomena, which demonstrates the lack of evidence regarding the real benefit of the different ventilatory maneuvers in the prehospital phase over mask ventilation especially when they are performed by untrained personnel33,34.