Introduction
Mental, neurological and substance use disorders contribute to a significant proportion of disease burden worldwide. These disorders are considered the third leading cause of disability-adjusted life years (DALYs) after cardiovascular and circulatory diseases as well as diarrhea, lower respiratory infections, meningitis, and other common infectious diseases1. For example, depression is a leading contributor to the global burden of disease and is nowadays a common chronic disease affecting the personal functioning and quality of life2. Even if most patients may benefit from pharmacological and/or psychotherapeutic treatment, many other patients may need adjuvant approaches, such as physiotherapy3.
People with severe and persistent mental disorders (e.g. schizophrenia, bipolar disorder and major depression disorder)4-7 report poor physical health and high rates of comorbid medical illnesses (respiratory and cardiovascular diseases, diabetes mellitus and obesity, among others) 8. For example, people with mental disorders are 2-3 times more likely to develop cardiovascular disease, they have an increased prevalence of metabolic syndrome, and their life expectancy is 15 to 25 years lower than in the general population9,10. These poor physical health conditions may be due to the mental disorder itself and the adverse effects of psychotropic drugs (e.g. antipsychotics), which are associated with metabolic and endocrine changes11. In addition, these patients are more likely to be involved in negative habits such as smoking, substance abuse, lack of physical activity, and the practice of unhealthy lifestyles12.
Physiotherapy can improve the quality of life of people with mental disorders13,14. This may be achieved through the optimization of their physical health as well as the relief of their psychosocial disability15, and through its role as an adjuvant treatment of the mental disorder itself16,17. There is evidence that improvements in muscle balance and flexibility are associated with a feeling of increased safety and increased self-esteem. In addition, an improved posture can benefit the body self-image and improve the mood, as well as decrease bodily pain. There is also strong evidence that an adequate regimen of physical exercise improves the well-being of people with mental disorders, such as depression and anxiety17,18.
Despite these benefits, researchers19 have stated that people with mental disorders do not regularly access Physiotherapy services for the management of their physical health problems and that there is still a lack of awareness on the role of Physiotherapy in mental health20.
A recent study surveyed 88 physiotherapists4 confirming that they do report the need of training opportunities in mental health, education in this area during the graduate school and professional development opportunities in Physiotherapy in mental health.
Some studies have focused on the barriers for people with mental disorders in accessing Physiotherapy services from the point of view of Mental Health professionals20, in determining the factors that influence the provision of Physiotherapy in the physical health management of people with mental disorders from the point of view of physiotherapists4, or in recognizing the positive impact of Physiotherapy in the management of the physical health of people with mental disorders21-24. Poor evidence is available on the knowledge about the role of Physiotherapy as an adjuvant treatment of mental disorders, not only for physical diseases affecting mentally ill persons.
This study aimed to determine the knowledge of physiotherapists about the provision of Physiotherapy services to people with mental disorders, about the role of Physiotherapy in the treatment of physical illnesses of mentally ill persons and in the treatment of the mental disorder itself.
Methodology
This was a pilot, descriptive, cross-sectional, and prospective observational study. A non-probabilistic sampling of consecutive cases was used. During the months of November 2019 to March 2020, a survey was carried out that included 187 physiotherapists in Paraguay, of both sexes, who agreed to participate in the research.
Instrument
The data collection instrument was a Spanish version of the survey used by Andrew et al.4 in Australia, which was adapted. The translation and adaptation of the instrument was carried out with the authorization of the original authors. The survey has been spread through Google Forms and distributed to mailing lists of physiotherapists practicing in Paraguay, inviting them to participate in the research. The survey contained closed (single-choice or multiple-choice) and open-ended questions, designed to collect information on participants' knowledge about the physiotherapy treatment of people with mental disorders (frequency of care for people with mental disorders; attitudes and knowledge about people with mental disorders, among others) and on the contribution of Physiotherapy in the treatment of mental disorders (its perceived role and the need for professional development in the area of Mental Health, among others). In addition, the survey contained a section to collect sociodemographic and professional information (age, sex, years of experience as a physical therapist, primary area of professional practice, area of work, main place of employment, location of employment and previous experience working in an environment of Mental Health services).
The data were processed using Microsoft Excel. Descriptive statistics were performed for all variables with central trend and dispersion measurements.
Ethical issues
This study is part of the research line "Physiotherapy in Mental Health", approved by Resolution No. 1163-00-2019 of the Dean of the School of Medicine of the National University of Asuncion, Paraguay. Data were treated with confidentiality, equality, and justice, respecting the Helsinki principles.
Results
187 physiotherapists completed the survey. 75.94% were women (142 participants). The mean age was 32.84 years, with a standard deviation of 7.95 years. The average number of years of experience as physical therapist was 8.47 ± 7.30 years. 49.2% graduated from a private University or Higher Institute, 34.22% worked in Trauma Physiotherapy and 87.7% worked with outpatients. The rest of the sociodemographic and professional data are shown in Table 1.
Table 1: Sociodemographic and professional characteristics of the participants (n=187).
| Characteristics | Frequency | ||
| n | % | ||
| University of origin | |||
| Private universities and institutes | 85 | 45.45 | |
| National University of Asunción | 83 | 44.39 | |
| Foreign universities | 19 | 10.16 | |
| Main professional practice area | |||
| Trauma physiotherapy | 64 | 34.22 | |
| Neurological physiotherapy | 31 | 16.58 | |
| Pediatric physiotherapy | 19 | 10.16 | |
| Sports physiotherapy | 17 | 9.09 | |
| Geriatric physiotherapy | 16 | 8.56 | |
| Cardiorespiratory physiotherapy | 16 | 8.56 | |
| Physiotherapy in ICU | 7 | 3.74 | |
| Physiotherapy in palliative care | 3 | 1.60 | |
| Dermato-functional physiotherapy | 3 | 1.60 | |
| Aesthetic physiotherapy | 2 | 1.07 | |
| Other | 9 | 4.81 | |
| Type of patients | |||
| Outpatient | 164 | 87.70 | |
| Inpatient | 23 | 12.30 | |
| Main scope of work | |||
| Hospital/Private Center | 145 | 77.54 | |
| Hospital/Public Center | 42 | 22.46 | |
| Location of the workplace | |||
| Rural | 5 | 24.06 | |
| Urban | 182 | 75.94 | |
Knowledge on the physiotherapeutic treatment of physical illnesses affecting people with mental disorders
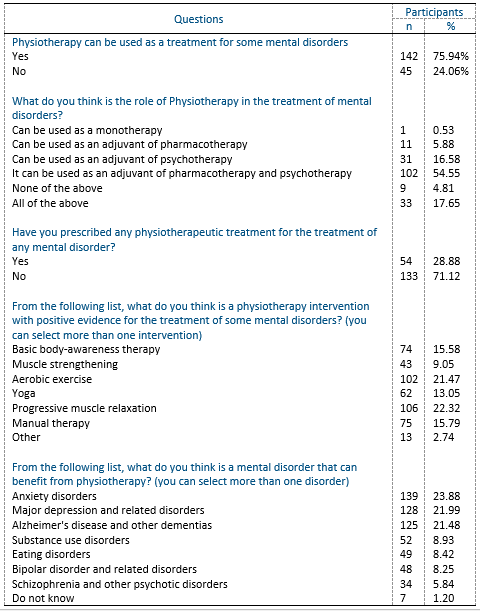
82.89% reported no previous experience in a Mental Health service and 61.50% reported a lack of information about the management of physical conditions affecting people with mental disorders. 46.52% stated that Physiotherapy is useful to manage physical symptoms in these patients and 35.83% reported that physiotherapy should be largely provided to mentally ill subjects. 55.61% asked for more information and/or training on the management of physical conditions affecting people with mental disorders. Table 2 shows these results in more detail.
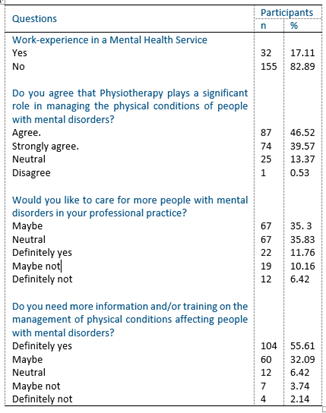
Table 2: Knowledge of the physiotherapeutic treatment of physical diseases affecting people with mental disorders. Part 1 (n=187).
41.18% reported that less than a quarter of their patients are people with mental disorders. 23.53% reported that this proportion may be due to an inadequate knowledge about the physiotherapeutic treatment of mentally ill people. More information can be found in Table 3.
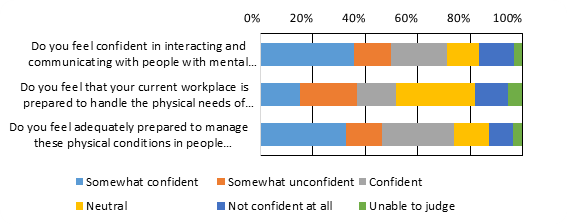
35.83% of participants reported feeling somewhat confident to interact and communicate with people with mental disorders. 14.97% felt that their workplace was somewhat prepared to treat the physical illnesses affecting people with mental disorders and 32.62% reported that they felt somewhat prepared to manage these physical conditions (cardiovascular diseases, respiratory diseases, metabolic syndrome and diabetes, among others). Figure 1 summarizes these findings.

Table 3: Knowledge of the physiotherapeutic treatment of physical diseases affecting people with mental disorders. Part 2 (n=187).
The need of more information for the management of the physical difficulties of people with mental disorders included: a. How physiotherapists can manage physical conditions that afflict people with mental disorders (39.04%); b. How to interact and communicate with people with mental disorders, their relatives and / or caregivers (21.93%); c. How to assess the behavioral risk of people with mental disorders, for example: risk of aggressiveness towards health personnel (16.04%); d. Physical conditions commonly associated with mental disorders (11.23%); e. Information on mental disorders in general, for example: symptoms, clinical presentation, available treatments (8.02%); and, f. All of the above (3.74%).
Knowledge of Physiotherapy as a treatment for mental disorders
75.94% of the participants stated that they were aware that Physiotherapy can be used as treatment for some mental disorders, mainly as an adjunct to both pharmacotherapy and psychotherapy (54.55%).
Jacobson's progressive muscle relaxation and aerobic exercise were considered to be effective in the treatment of some mental disorders (22.32% and 21.47%, respectively).
Participants mentioned that anxiety disorders (23.88%), major depression and related disorders (21.99%), and Alzheimer's disease and other dementias (21.48%) could mostly benefit from physiotherapy treatment. Table 4 presents these results in detail.
20.3% of sample reported to be aware on the existence of services providing Physiotherapy in the treatment of mental disorders in Paraguay. The “Hospital de Clínicas” of the School of Medicine, at National University of Asunción, was one of the most recognized health services (50%).
Discussion
To the best of our knowledge, this is the first research carried out in a Spanish-speaking country in order to determine the knowledge that physiotherapists have about the provision of Physiotherapy to people with mental disorders and about the role of Physiotherapy in the treatment of the physical illnesses of people with mental conditions, as well as those related to the use of Physiotherapy in the treatment of mental disorders. Although there is a similar work done in Australia4, it focused on studying physiotherapists' perceptions of their role in the management of people with mental disorders, as well as the barriers they identified in the provision of Physiotherapy services for this population, but did not measure knowledge regarding the use of Physiotherapy as a treatment for mental disorders.
In this study, more than 80% of surveyed Physiotherapists recognized that Physiotherapy plays a significant role in the management of physical conditions affecting people with mental disorders, and almost 50% of the participants would like to treat more people with these comorbidities. This is in line with what was reported by Andrew et al.4, who in their study found that the majority considered that the treatment of people with mental disorders was part of their work and that Physiotherapy had an important role in the management of physical diseases that affect this population.
Likewise, our results may support the evidence of a positive attitude of physical therapists in managing physical illnesses of people with mental disorders21-24. However, this research also showed the existence of some barriers to this. Although 35.83% of participants reported feeling somewhat confident and/or capable of interacting and communicating with people with mental disorders, and 32.62% stated they felt somewhat able of managing physical frequent comorbidities (cardiovascular diseases, respiratory diseases, metabolic syndrome and diabetes), more than 60% reported that they could not access information about the management of these physical conditions. Furthermore, more than half of surveyed physiotherapists reported the need of more information and/or training regarding the management of physical conditions affecting people with mental disorders. This is a clear sign of the lack of an adequate training at undergraduate and graduate levels, as confirmed by previous findings25.
Connaughton and Gibson25 identified gaps in knowledge about mental illness among Physiotherapy students (due to insufficient content in the undergraduate curriculum programs). Since mental disorders are increasing in prevalence, for example major depression affects approximately 340 million people worldwide26, with a prevalence at lifetime of around 20.6%27, and up to 33.7% of people are affected by an anxiety disorder during their lifetime28, the need training in mental Health for physical therapists is encouraged.
Our finding about the need for more information and/or training on managing physical conditions that affect people with mental disorders, is consistent with previous studies15,29. Education among physiotherapists should include psychopathology, available treatments of mental disorders in general, and frequent comorbid physical comorbidities30. In addition, communication techniques should be improved.
In Paraguay, the first initiative carried out jointly between resident physicians of Psychiatry and resident physiotherapists of the National University of Asunción (involving the Department of Psychiatry and the Department of Kinesiology and Physiotherapy of the School of Medical Sciences of the National University of Asunción), led to training opportunities. As a result, a first Paraguayan book has been published on the topic3, as well as scientific articles13,18,31.
In our study, it is noteworthy that a non-negligible number of physical therapists considered that they needed more information about how to interact and communicate with people with mental disorders (21.93%) and how to assess the behavioral risk and risk of aggressiveness towards health professionals (16.04%). Some researchers have already reported the existence of such beliefs among health professionals, including physical therapists32-35.
Stigma may also limit access to health services for people with mental disability36. Education on Mental Health (and mental disorders) is also essential to reduce prejudices and discrimination37. Educational processes should include elements on risk assessment, substance abuse and how to manage aggressive patients38-41.
Importantly, in this study, the majority of people seen by physical therapists were isolated cases and not referred by general practitioners. The lack of medical referral to Physiotherapy has been pointed out by some other authors4. Musculoskeletal complains among psychiatric patients were mostly managed by the surveyed physiotherapists in this study: this may reflect that Physiotherapists do not generally treat physical symptoms of mental disease and general practitioners are not referring them. Nonetheless, a large majority (75.94%) of physical therapists stated that they were aware that Physiotherapy can be used as treatment of some mental disorders, as an adjunct to both pharmacotherapy and psychotherapy. Physiotherapy in Mental Health may improve physical symptoms and well-being by promoting functional movement, awareness of movement, activity and physical exercise42. Approaches may include: basic body-awareness therapy43-45, muscle strengthening46,47, aerobic exercise48-51, yoga52,53, progressive muscle relaxation54-56, manual therapy57 and therapeutic Pilates 31, among others. In our study, Jacobson’s progressive muscle relaxation and aerobic exercise were recognized as the most effective physiotherapeutic interventions for the treatment of some mental disorders (22.32% and 21.47%, respectively).
Participants scored that anxiety disorders (23.88%), major depression and related disorders (21.99%), and Alzheimer’s disease and other dementias (21.48%) were those mental disorders benefiting from a physiotherapy intervention. This has been confirmed by previous evidences3,15,16,58. Also, it is important to emphasize that, currently, aerobic exercise can be used even in monotherapy for mild depression26. Physiotherapy may improve the symptoms of mental disorders through various approaches: a. improving the overall physical health; b. psychophysiological approach enhancing physical competences related to the body; and c. approach related to psychotherapy, using the body as a gateway to improve the affective and social functioning of the individual12,59.
Limitations of this study may include the type of sampling used, since, being a non-probabilistic type sampling, its results cannot be generalized. However, given its internal validity, it can be considered that the results are applicable for the study-sample. Also, it was not possible to establish a certain degree of causality between the variables but rather they were studied cross-sectionally. Finally, a study-design including a qualitative component is needed to further explore physiotherapists' perceptions of this particular area.
We conclude that Physiotherapy has a potential role in managing the physical needs of people with mental disorders, and there may be a need to strengthen the skills and knowledge of physical therapists in order to address some specific needs of people with mental disorders. An adequate training of professional physiotherapists, starting from undergraduate education, is encouraged60.