Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Cirugía paraguaya
On-line version ISSN 2307-0420
Cir. parag. vol.47 no.3 Asunción Dec. 2023
https://doi.org/10.18004/sopaci.2023.diciembre.23
ORIGINAL ARTICLE
Experience in the surgical treatment of bile duct stone not removed by ERCP at the Itauguá National Hospital from January to October 2022
1Hospital Nacional. Itauguá. Paraguay.
Introduction: Bile duct stones is the presence of calculi in the common bile duct caused by its migration from the gallbladder or its extrahepatic or intrahepatic formation in the bile duct. Objective: Determine the surgical conduct adopted for BDS treatment not removed by ERCP. Materials and methods: Observational, retrospective, descriptive, cross-section study. Results: From the studied patients, calculi were found in 62% of the performed ERCP, in which the symptoms were resolved 85% of the times (151/245). The average age was of 56.3 ± 20.75 years old with a female predisposition of 78%. In the remaining patients, the most used surgical techniques were open surgery (22/23) and choledochotomy, more frequently with primary closure (14/23). Only a single case was resolved by laparoscopy. Conclusion: open method and choledochotomy with primary closure are the main surgical techniques used.
Keywords: Bile duct stones; Endoscopic retrograde cholangiopan- creatography; Cholecystectomy.
Introducción: La coledocolitiasis es la presencia de cálculos en el colédoco como consecuencia de su migración desde la vesícula o de su formación en la vía biliar extrahepática o intrahepática. Objetivo: Determinar la conducta quirúrgica adoptada para el tratamiento de la coledocolitiasis no resuelta por CPRE. Materiales y métodos: Estudio observacional, retrospectivo, descriptivo, de corte transversal. Resultados: De los pacientes en estudio se hallaron cáculos en el 62% de las CPRE realizadas, en los cuales se pudo resolver el cuadro en 85% (151/245). La edad media fue de 56,3 ± 20,75 años con mayor predominio del sexo femenino en el 78%. En los demás pacientes la técnica quirúrgica evidenció en la mayoría se realizó cirugía abierta (22/23) y coledocotomía, más frecuentemente con rafia primaria (14/23). Un solo caso fue resuelto por laparoscopía. Conclusión: para el tratamiento quirúrgico de las coledocolitiasis se utiliza principalmente la vía abierta, y la coledocotomía con rafia primaria.
Palabras claves: Coledocolitiasis; Colangiografía retrograda endoscópica; Colecistectomia
INTRODUCTION
Bile duct stones (BDS) is the presence of calculi in the common bile duct caused by its migration from the gallbladder (secondary stones) or its extrahepatic or intrahepatic formation in the bile duct (primary stones) (1); representing a gallstone complication that is present in 7-20% of symptomatic lithiasis (2).
Asymptomatic BDS has a 75% chance of becoming symptomatic at some point during its evolution and bring forth serious complications such as: acute cholangitis, acute pancreatitis, among others, possibly deadly pathologies hence it must always be treated(3-4).
BDS diagnosis is based on the combination of symptoms and clinical signs, serum cholestasis markers and imagery findings (transabdominal ultrasound, among others); individually these pointers possess variable levels of diagnostic precision and none of them, by themselves, represent a completely reliable method to identify bile duct calculi (5-6).
The ideal BDS treatment is still a subject of debate; with the invention and development of the endoscopic cholangiopan- creatography and sphincterotomy, the presurgical endoscopic handle of BDS was popularized, followed double-time (ideally not more than 24 hours) by laparoscopic cholecystectomy (7).
Laparoscopic bile duct exploration techniques have still been refined and consolidated, although the studies that have compared the single-time surgical handle against the sequential handle are few; both modalities show similarities in terms of common bile duct cleaning and complications, however single-time handle results in a shorter hospital stay reduced costs. In that regard, BDS handle depends nowadays on the surgical team’s experience and the technological availability of hospital centers (8-10).
The present study’s objective is to evaluate retrospective data of patients with a BDS diagnosis not resolved by an endoscopic retrograde cholangiopancreatography (ERCP) who were sub- mitted to surgical treatment between January through October of 2022 in the Hospital Nacional de Itauguá.
MATERIALS AND METHODS
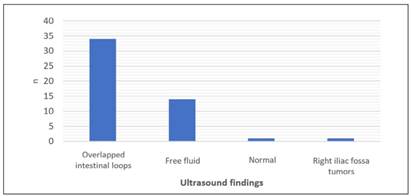
Observational, retrospective, descriptive, cross-section study. The work’s objective was to determine the surgical conduct adopted for BDS treatment not resolved by ERCP in admitted patients in the Hospital Nacional de Itauguá, from January through October 2022. Patients of both genders were included, 18-yeard-old and older, with a BDS diagnosis through ERCP, in the Hospital Nacional de Itauguá during the period between January through October of 2022. Deceased patients and those with incomplete forms were excluded. For data recollection records from the Endoscopy Service, patients’ clinical forms and surgical techniques of surgery-submitted patients were re- viewed. The Excel® and EpilnfoTM programs were employed for data processing and analysis. A descriptive analysis of all analyzed variables was performed.
RESULTS
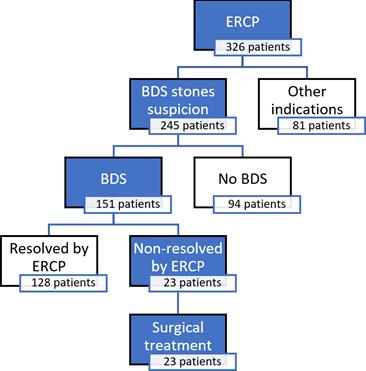
Between January and October of 2022, 326 ERCP procedures were performed, from which 75% (245 patients) were ordered for patients with BDS suspicion, 25% (81 patients) for other rea- sons (neoplasia, biliary stent, biopsy sample, etc.).
From the 245 patients submitted to ERCP by BDS suspicion, calculi were found in 151 patients equal to 62%, and no calculi were found in 94 patients equal to 38%, being ERCP unnecessary. (see Figure 1).
Of the 151 patients of which BDS were reported, 128 patients equal to 84% had a successful ERCP extraction and 23 patients (16%) had an unsuccessful one due to various reasons (calculi disproportion, lack of appropriate instruments, multiple lithiasis). This last group belong to the surgically handled patients, whether by conventional or laparoscopic approach (see Graphic 1).
Of the 23 patients of which BDS extraction by ERCP was unsuccessful, an average age of 56.3 ± 20.75 years old was identified, with aa range between 24 to 92 years old. (see Graphic 2). The age group with the most frequency was the 70-years-old un upwards, with 30% (n=7) of the cases. Most patients were of the female gender with 78% (n=18).
Presurgical diagnosis were obstructive jaundice by BDS and acute cholangitis by BDS, with 61% and 39% respectively, equal to 14 and 9 patients.
Of the 23 patients, 15 (65%) presented an on-site gallbladder, while the 35% (8 patients) had already being submitted to either conventional or laparoscopic cholecystectomy. (see Table 1)
The surgical technique showed that in 96% of the patients, a conventional or open choledochotomy was performed, and only in a single case through laparoscopy. It is observed that in patients without gallbladder surgery history a cholecystectomy +
choledochotomy was performed equal to 39% (n=9), which was the most frequent situation, followed by cholecystectomy + choledochotomy + Kehr’s T tube placement which was performed in 4 patients equal to 17% and cholecystectomy + choledochot- omy + transcystic drainage placement on 2 patients (9%). On the other hand, 5 patients (22%) that had already had a chole- cystectomy performed on a previous occasion were submitted to a choledochotomy + primary closure, 3 patients (13%) to a choledochotomy + Kehr’s T tube placement. (see Table 1).
DISCUSSION
Despite multiple studies and different expert meetings, currently there isn’t an algorithm for the diagnosis and treatment of BDS that could be considered the gold standard.(10)
Nowadays, bile lithiasis disease is a clearly identified condition that forces the general physician, gastroenterologist, and general surgeon to have a proper diagnostic approach; this pathology contemplates a spectrum of clinical and paraclinical manifestations according to the lithiasis’ location and to this day there isn’t an optimal approach for patients in risk of BDS. (11)
Amongst the literature there is a variety of predictive models that seek to focus an optimal handle of these patients; the ASGE grading system stratifies said patients according to clinical criteria, ultrasound imagery, and labs and categorizes them with the goal of achieving a better handle of BDS risk.(11)
Currently, the usual treatment consists of first performing an ERCP and then a cholecystectomy; if the first one fails, bile duct exploration with Kehr’s T tube placement or primary closure is indicated. The laparoscopic approach is the worldwide standard; however, it is not a common practice in our area.(12)
In this work a total of 326 ERCP procedures were considered, from which 75% (n=245) were indicated due to BDS suspicion and 25% (n=81) due to other causes.
Amongst the patients with probable BDS, it was confirmed in 151 (62%) of them, with calculi absence in 94 patients. The low lithiasis finding percentage tells us that ERCP indication is not optimal, needing the utilized criteria to be evaluated; ac- cording to a study published by the Hospital de Clínicas (Asunción) in 2019, of the 40 patients submitted to ERCP due to BDS suspicion, calculi were reported in 21 of them (51%) numbers similar to the ones in the present work.(13)
Since its implementation, ERCP has become an excellent technique for the preoperative study of the bile duct, with di- agnostic sensibility and specificness close to 100%; it allows, through a side view endoscope, to cannulate the papilla and to opacify the bile duct injecting contrast. In this study, ERCP proved to be effective in 84% of BDS patients; according to a study published by Franco López J in 2021, endoscopic treatment’s effectiveness was of 79.2%(14)
Regarding the average age of the patients submitted to sur- gery (50 years old), it is similar to the one found in literature and other performed studies at national level; the greater prevalence in the female gender also matches the greater frequency of bile lithiasis presentation on said gender, being considered a risk factor for said pathology.(1)
Presurgical diagnosis were obstructive jaundice by BDS and acute cholangitis by BDS; with 61% and 39% respectively based on clinical and imagery criteria; according to an international study published in March of the current year performed in 1.001 patients, the most common ERCP indication was confirmed or suspected BDS in 52,6% of cases and cholangitis suspicion in 7.7%(15).
In this group of patients, open or conventional surgery was performed in most of them and a choledochotomy was done in all of them. Choledochotomy’s primary closure was the most frequent procedure, followed by Kehr’s drainage and the trans- cystic one. In the study performed by Machain G in 2021, choledochotomy with Kehr’s drainage by open surgery was the most performed surgery done in patients submitted to surgery due to non-resolved BDS by ERCP (21 cases).(13)
The main bias of the current study is the lack of long-term follow-ups, in order to corroborate subsequent clinical success.
CONCLUSION
326 ERCP procedures were performed during the study, 245 were by suspicion of BDS, which was confirmed in 151 patients, giving a total of 38% of unnecessary ERCP (94 patients).
Of the 151 BDS patients, calculi extraction by ERCP was successful in 128 patients (85%), and the remaining 23 patients were submitted to surgical resolution.
All the BDS cases which were submitted to surgery were resolved: in every case a choledochotomy was performed, most of them by primary closure. Only one case was resolved by laparoscopic approach.
REFERENCES
1. Ferraina P, Oría A. Cirugía de Michans. 5° Edición. Buenos Aires Argentina: Editorial El Ateneo; 2008. [ Links ]
2. Benites Goñi HE, Palacios Salas FV, Asencios Cusihuallpa JL, Aguilar Morocco R, Segovia Valle NS. Rendimiento de los criterios predictivos de la ASGE en el diagnóstico de coledocolitiasis en el Hospital Edgardo Rebagliati Martins. Rev. Gastroenterol. Perú [Internet]. 2017;37(2):111-9. Disponible en: https://www.scielo.org.pe/scielo.php?script=sci_arttext&pid=S1022-51292017000200002 [ Links ]
3. Ortiz de la Peña Rodríguez J, de la Fuente Lira M, Orozco Obregón P. Colangiografía transoperatoria, procedimiento selectivo o rutinario. Rev Mex Cir Endoscop. [Internet]. 2001;2(4):185-187. Disponible en: https://www.medigraphic.com/cgi-bin/new/resumen.cgi?IDARTICULO=6536 [ Links ]
4. Skandalakis JE, Skandalakis PN, Skandalakis LJ. Anatomía y técnica quirúrgicas. 2da ed. Madrid, Mcgraw Hill; 2002. [ Links ]
5. Zhu HY, Xu M, Shen HJ, Yang C, Li F, Li KW, et al. A Meta-analysis of single stage vs two stage management for concomitant gall stones and common bileduct stones. Clin Res Hepatol Gatroenterol. [Internet]. 2015;39: 584-93. Disponible en: https://pubmed.ncbi.nlm.nih.gov/25936687/ [ Links ]
6. Ding GQ, Cai W, Qin MF. Single-State vs. Two-stage management for concomitant gall stones and common bileduct stones. Rev. Gastrintest. Surg. [Internet]. 2014; 18:947-51. Disponible en: https://pubmed.ncbi.nlm.nih.gov/25936687/ [ Links ]
7. Barreto Suárez E, Soler Porro LL, Sugrañes Montalván A. Coledocolitiasis: diagnóstico y terapéutica mediante la colangiopancreatografía retrógrada endoscópica. AMC Camagüey [Internet]. 2010 Dic;14(6):1-10. Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1025-02552010000600007 [ Links ]
8. Barreras González JE, Torres Peña R, Ruiz Torres J, Martínez Alfonso MA, Roque González R, Brizuela Quintanilla R. Algoritmo para el tratamiento mínimamente invasivo de la coledocolitiasis. Rev Cuba Cir. [Internet]. 2014;53: 346-55. Disponible en: http://scielo.sld.cu/pdf/cir/v53n4/cir03414.pdf [ Links ]
9. Phillis E, Berci G, Barker K, Williams J. The role of choledochoscopy: The eternal problem of howtoremove a CBD Stone. SurgInnov. [Internet]. 2015;22: 540-5. Disponible en: https://pubmed.ncbi.nlm.nih.gov/26187857/ [ Links ]
10. Oblitas NM. Pruebas de laboratorio como predictores de coledocolitiasis en pacientes sometidos a CPRE en un hospital nacional de referencia. Lima: Facultad de Medicina, Universidad Nacional Mayor de San Marcos. Rev. Gastroent. Peru. [Internet]. 2015; 27(3) Disponible en: https://www.scielo.org.pe/scielo.php?script=sci_arttext&pid=S1022-51292007000300005 [ Links ]
11. Toro Calle J, Guzmán Arango C, Ramírez Ceballos M, Guzmán Arango N. Son los criterios de la ASGE suficientes para la estratificación del riesgo de la coledocolitiasis. Rev. Colomb. Gastroent. [Internet]. 2020. Disponible en: https://revistagastrocol.com/index.php/rcg/article/view/464/954 [ Links ]
12. Cuadrado D, Salazar A, Orozco J, Buitrago D. Exploración laparoscópica de la vía biliar con cierre primario en casos de colecisto-coledocolitiasis en el Hospital Universitario San Ignacio. Rev. Colomb. Cir. [Internet]. 2017; 32(3): 182-185. Disponible en: https://www.redalyc.org/journal/3555/355553288004/html/ [ Links ]
13. Machain G, Arellano N, Melgarejo S, Páez L, Cáceres M. Predictores de coledocolitiasis en pacientes con litiasis vesicular sintomática tratados en la segunda catedra de clínica quirúrgica, Hospital de clínicas, San Lorenzo. Rev. Paraguaya. Cir.[Internet]. 2021, 54(1). Disponible en: http://scielo.iics.una.py/scielo.php?script=sci_arttext&pid=S1816-89492021000100101 [ Links ]
14. Franco López J, Ferreira Bogado M, Adorno Garayo C. Efectividad del tratamiento endoscópico en el manejo de la coledocolitiasis en el servicio de endoscopia digestiva del Hospital Nacional de Itauguá. Rev. Paraguaya. Cir. [Internet]. 2021, 45(3). Disponible en: http://scielo.iics.una.py/scielo.php?script=sci_arttext&pid=S2307-04202021000300011 [ Links ]
15. Qureshi L, Alzanbagi A, Tashkandi A, et al. Analisis retrospectivo de las características, indicaciones y resultados de la CPRE en un centro de referencia en Arabia Saudita. Rev. Pub. Med. [Internet].2023, 15(3). Disponible en: https://pubmed.ncbi.nlm.nih.gov/37123677/ [ Links ]
Author’s contribution
Ríos S: Conceptualization, data analysis, formal analysis, investigation, methodology, project administration, resources, validation, visualization, writing of the original draft, writing, revision, and editing.
Franco López J, Echague M.: Conceptualization, methodology, supervision, validation, visualization, writing, revision, and editing.
Conflict of interest: The present study respects the bases of medical ethic given that it will not produce any ill-being to the patients; likewise corresponding authorization was solicited to the General Surgery Service’s personnel.
Ethical considerations: Patient’s information will remain anonymous. This study does not present any risk to the patients. Results and conclusions of this investigation will be available to any who requires them.
Received: July 10, 2023; Accepted: December 10, 2023











 text in
text in