Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Cirugía paraguaya
On-line version ISSN 2307-0420
Cir. parag. vol.47 no.3 Asunción Dec. 2023
https://doi.org/10.18004/sopaci.2023.diciembre.11
Original Article
Transient hypocalcemia after total thyroidectomy on general surgery services. Hospital Nacional de Itauguá. Period: 2016 - 2022
1Ministerio de Salud Pública y Bienestar Social, Centro Médico Nacional, Hospital Nacional, Departamento de Cirugía. Itauguá, Paraguay
2Ministerio de Salud Pública y Bienestar Social, Centro Médico Nacional, Hospital Nacional. Servicio de Cirugía de Cabeza y Cuello. Itauguá, Paraguay
Introduction: Transient post thyroidectomy hypocalcemia is the most frequent complication of neck surgery, it can be mild and asymptomatic, or severe. The objective was to identify the incidence of transient hypocalcemia in patients undergoing total thyroidectomy, in the General Surgery Service of the Hospital Nacional de Itauguá. Material and methods: A descriptive, observational, retrospective, cross-sectional study was carried out, with a non-probabilistic sampling of consecutive cases of all patients undergoing total thyroidectomy for benign pathology, from January 2016 to December 2022. Conclusions: Of the total of 141 records of operated patients, in the distribution by sex a prevalence of 92% of the female sex with an average age of 55 years ± 5 SD was found. The incidence of laboratory hypocalcemia was 32.6% (46), con- sidering the total calcium value less than 8 mg/dl; however, only 19.9% (27) of the patients presented clinical hypocalcemia.
Keywords: Hypoparathyroidism; Hypocalcemia; Thyroidectomy
Introducción: La hipocalcemia transitoria postiroidectomia es la complicación más frecuente de la cirugía cervical, la misma puede ser leve y asintomática, o grave. El objetivo fue identificar la prevalencia de hipo- calcemia transitoria en paciente operados de tiroidectomía total, en el servicio de cirugía general del Hospital Nacional de Itauguá, durante el periodo entre enero de 2016 a diciembre de 2022. Métodos: Se realizó un estudio descriptivo, observacional, retrospectivo de corte transversal, con un muestreo no probabilístico de casos consecutivos de todos los pacientes sometidos a tiroidectomía total por patología benigna, desde enero 2016 hasta diciembre 2022. Resultados: Del total de 141 fichas de pacientes post operados, en la distribución por sexo se encontró una prevalencia del 92% del sexo femenino con una edad promedio de 55 años ± 5. La prevalencia de hipocalcemia laboratorial fue de 32,6% (46), considerando el valor de calcio total inferior a 8 mg/dL, sin embargo, solo el 19,1% (27) de los pacientes presentó hipocalcemia clínica. Conclusión: La hipocalcemia sigue representando una complicación frecuente en la tiroidectomía: desde un 19,1% con manifestaciones clínicas hasta casi un tercio de los pacientes en los análisis laboratoriales.
Palabras clave: Hipoparatiroidismo; Hipocalcemia; Tiroidectomía
INTRODUCTION
Postoperative hypocalcemia is the most frequent of the thyroidectomy complications1, some can be mild and totally asymptomatic while others can manifest bronchospasms, laryngospasms, seizures, and conscious-level alterations2. In general, when there is clinical proof of hypocalcemia the blood calcium levels are 8.0 or will be under 8.0 mg/dL3.
The most frequent injury mechanism is direct damage to the parathyroid glands: whether it is by a vascular system injury, by mechanical damage or by partial or complete excision of them- selves, voluntary or not4.
Due to, in most cases, postoperative hypocalcemia being re- solved on the first month after surgery, some authors choose to wait to the 4-6th week to establish a hypoparathyroidism diagnosis5,6 that can be classified according to its transitory treatment time if the recovery happens in less than 12 months and permanent if this period is exceeded6.
Hypocalcemia caused by lack of parathyroid hormone (PTH) can be severe, and present symptoms of carpopedal spams, tetany, seizures, and QT interval lengthening. Likewise, asymptomatic hypocalcemia presents acutely with corrected calcium levels less than or equal to 7.5 mg/dL, which could lead to serious complications if left untreated6.
Chvostek sign can be positive in 10% of normocalcemic patients, and be absent in 30% of hypocalcemic patients, while Trousseau sign is more sensitive and specific, appearing in 95% of hypocalcemic patients and only in 1% of normocalcemic ones7. The diagnosis done with the blood’s analytics is the diagnostic proof that allows the specialist to determine whether there is hypocalcemia or not. Hypocalcemia is considered to exist when the blood calcium quantity is below 8.0 mg/dL. However, it must be corrected in accordance with the albumin, given that low al- bumin levels can produce a false hypocalcemia (1 g/dl drop of albumin decreases 0.8 mg/dL of calcium)8.
The acute hypocalcemia treatment (of fast emergence), symptomatic or with low calcium levels (under 7 mg/dL) consists of intravenously administering calcium, which must be replenished first5,8.
Chronic hypocalcemia treatment consists of orally administering calcium and vitamin D supplements. The objective is to keep calcium levels just below the average. To do this blood calcium levels must be controlled, first weekly and, once stabilized, every 1-3 months9.
The objective of the present work was to identify the incidence of transitory hypocalcemia on total thyroidectomy surgery patients, within the General Surgery Service of the Hospital Nacional de Itauguá between January 2016 to December 2022.
METHODS
A descriptive, observational, and retrospective cross-section study was performed, alongside a non-probabilistic sampling of consecutive cases of all the total thyroidectomy patients from January 2016 to December 2022 on the Hospital Nacional de Itauguá. Patients with a TI-RADS (Thyroid Imaging Reporting and Data System) III preoperative ultrasound diagnosis and fine-needle (PAAF) Bethesda III aspiration10 with proper thyroid profile control were also included, whom which had a total calcium control at postoperative 12 hours. Those who had the same laboratory hypocalcemia symptoms as the patients with a postoperative total calcium level below 8 mg/dL were deemed as clinical hypocalcemia. Those with TI-RADS IV or above, or Bethesda IV or above, those who required some other procedure besides total thyroidectomy alike lymphatic drainage, those with an altered preoperative thyroid profile, and those with only postoperative ionic calcium controls were excluded. 152 patient forms were included, of which only 11 did not have a total calcium control at 12 hours, reason why they were omitted.
Acquired data was arranged in Microsoft Excel® and frequency, percentage, and measures of dispersion (standard deviation, SD) tables were used.
Bioethical principles were respected: obtained information was confidentially analyzed. Inquired consent was not required due to the data being extracted from the records. There was no risk of illintension nor discrimination. There were no commercial interest conflicts.
RESULTS
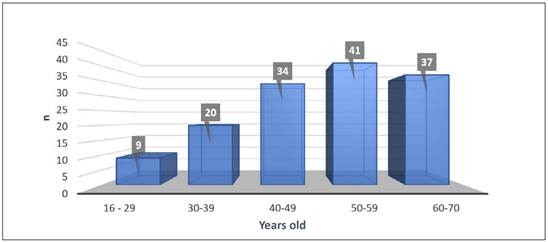
From the total of 141 postoperative patient forms, in the gender distribution it was found a 92% (130) female gender and 8% (11) male gender ratio. The average age of the patients was 55 years-old ± 5, with the following distribution of age groups: 16- 29 years-old 6.4% (9 patients), 30-39 years-old 14.1% (20), 40-49 years-old 24.2% (34), 50-59 years-old 29.1% (41), 60-69 years-old 26.2% (37). See Graphic 1.
Of the 141 total thyroidectomy patients, all of them had a preoperative ultrasound TI-RADS III diagnosis, and through PAAF Bethesda III it was found an incidence of laboratorial hypocalcemia of 32.6% (46), considering the total calcium levels below 8 mg/dL, however, only 19.1% (27) of patients presented a clinical hypocalcemia, the remaining 80.9% (144) were asymptomatic, see Table 1.
All laboratorial hypocalcemia cases received oral calcium treatment.
DISCUSSION
In our research we obtained a 92% (130) prevalence of the female gender. A slightly elevated figure compared to the one mentioned by Velázquez et al, whom in a multicenter study on the Universidad Nacional de Asunción found an 85.7% prevalence of the female gender in 1,913 thyroidectomy patients11.
The average age obtained was 55 years-old ± 5, a figure which differs from the one found by Velázquez et al that stratifies age for cancer types, with papillary cancer being the most frequent one, 42 years-old ± 13.11 This age is also elevated compared to the sample of Medina Ruiz et al who in the Instituto del Cáncer del Paraguay found the average age of 47 years-old.12 These results are more similar to the ones obtained in 2012 on the surgical oncology service of the Hospital San Juan de Dios of Costa Rica, where the demographic variables of age and gender are included as a risk factor for postoperative hypoparathyroidism, finding that 85% appertains to the female gender with an average age of 50 years-old9.
Laboratorial hypocalcemia prevalence was 32.6% (46), dosed between 12 to 24 hours postoperative; Franco Lopez et al found in a parallel study at the Hospital Nacional a postthyroidectomy hypocalcemia incidence of 55.4% in 97 patients. With a 78.4% of global postthyroidectomy complications this study does not mention that TI-RADS or Bethesda were included.13 While Medina Ruiz et al describes only a 15.3% of transitory hypocalcemia in total thyroidectomy patients with a clinical goiter classification of Grade 2 and 3, whereas more than 80% were benign11. Barquero Melchor el at, in Mexico reported a post thyroidectomy hypocalcemia rate of 50%, considering patients that required lymphatic drainage as part of the sample.9 Gac-E et al in Santiago de Chile obtained similar figures in 448 patients, where they also found a postoperative hypocalcemia rate of 50%14. This difference could be explained by the encompassed population, in this study only patients with TI-RADS III and Bethesda III were included, considering them as low malignant potential, and whom only required a total thyroidectomy, and lymphatic drainage techniques were not included.
In a study performed by González-Botas in 2013 in Spain about total thyroidectomy surgery, transitory hypocalcemia was found in 29.1%, where the cause was due to trauma or inadvertent injury of the parathyroid gland.7 The figure is close to the one in our study, which we consider low. The clinical test is not the most sensible one to measure hypocalcemia given that only 19.1% (27) manifested symptoms in postoperative, phenomena also described by Gac-E et al in Chile which found a laboratorial incidence of 42-50% with a clinical manifestation of only 14.8- 15%.14 In our research, the treatment in every single case was immediate and with a good clinical response through oral method. We do not certified cases of severe hypocalcemia.
This report has its limitations: it only analyzes total thyroidectomies through probably benign pathologies hence results cannot be generalized; on the other hand, it’s a retrospective design with a less-than 30 days follow-up.
Medium and long-term patient follow-up is recommended, to describe the transitory hypocalcemia’s incidence or permanence, besides a longitudinal study of cases and controls to relate the variables with which determine the emergence of postoperative hypocalcemia. Another possible bias was the lack of correlation between the anatomical pathology reports.
CONCLUSION
The female gender is more prevalent when submitted to thyroidectomy, with an average age of 55 years old. The laboratorial postthyroidectomy hypocalcemia’s prevalence through benign pathologies is 32.6%, while the clinical hypocalcemia is of 19.1%. Every hypocalcemia case presented a proper response to early oral treatment.
REFERENCES
1. Fretes D, Cardozo AHR, Caballero R AM, Fretes A, Insfran S, Verdecchia-Insfran CP. Incidencia de complicaciones de la tiroidectomía total en el Servicio de Cirugía General Hospital Militar Central de las Fuerzas Armadas de la Nación. Periodo Noviembre de 2018 - Septiembre de 2019. Cir. Parag. 2020:44(2);25-25 https://doi.org/10.18004/sopaci.2020. agosto.25 [ Links ]
2. Martínez Bello A, Rivera Real P, Reyes García MA. Morbilidad posquirúrgica en pacientes sometidos a tiroidectomía en el hospital general de Acapulco. Tres años de experiencia. Cir. Gen. [revista en la Internet]. 2014;36(2):91-95. Disponible en: http://www.scielo.org.mx/scielo.php?script=sci_arttext&pid=S1405-00992014000200091&lng=es [ Links ]
3. Gutierrez Fernandez G, Lopez Useros A, Muñoz Cacho P, Casanova Rituerto D. Prediccion de hipocalcemia postiroidectomia mediante determinacion de PTH rapida Cir. Esp. 2021;99(2):115-123. DOI: 10.1016/j. ciresp.2020.05.009 [ Links ]
4. Huguet I, Muñoz M, Cortés M, Romero M, Varsavsky M, Gómez J. Protocolo de diagnóstico y manejo de hipocalcemia en postopera- torio de tiroides. Rev Osteoporos Metab Miner [Internet]. 2020 Jun; 12(2): 71-76. Disponible en: http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1889-836X2020000200006&lng=es Epub 05-Oct-2020. https://dx.doi.org/10.4321/s1889-836x2020000200006 [ Links ]
5. Ventosa-Viña M, Cuéllar-Olmedo L, Crespo-Soto C, Palacio-Mures JM, García-Duque M, Lázaro-Martín L. Actualización en el tratamiento del hipoparatiroidismo posquirúrgico. Revista ORL 2022; 13(3): e27528. https://doi.org/10.14201/orl.27528 [ Links ]
6. Román-González A, Zea-Lopera J, Londoño-Tabares SA, Builes-Barrera CA, Sanabria A. Pilares para el enfoque y tratamiento adecuado del paciente con hipoparatiroidismo. Iatreia [Internet]. 2018; 31(2): 155-165. https://doi.org/10.17533/udea.iatreia.v31n2a04 [ Links ]
7. Gonzalez-Botas JH, Lourido Piedrahita D. Hipocalcemia postiroidectomía total: incidencia, control y tratamiento. Acta otorrinolaringologia 2013; 64(2):102-107 https://doi.org/10.1016/j.otorri.2012.09.001 [ Links ]
8. Castro Calvo A. La PTH como predictor de la necesidad de tratamiento para la hipocalcemia post-tiroidectomia [Tesis doctoral]. Madrid: Universidad Autónoma de Madrid; 2015. Recuperado a partir de: https://repositorio.uam.es/bitstream/handle/10486/669528/castro_calvo_alejandro.pdf [ Links ]
9. Barquero-Melchor H, Delgado-Rodríguez MJ, Juantá-Castro L. Hipocalcemia e hipoparatiroidismo post tiroidectomía. Acta méd. costarric 2015;57(4):184-189 Disponible en: https://www.scielo.sa.cr/pdf/amc/v57n4/0001-6002-amc-57-04-00184.pdf [ Links ]
10. Horvath E, Silva CF, Majlis S, et al. Prospective validation of the ultrasound based TIRADS (Thyroid Imaging Reporting And Data System) classification: results in surgically resected thyroid nodules. Eur Radiol 2017;27(1):2619-2628. DOI: https://doi.org/10.1007/s00330-016-4605-y [ Links ]
11. Velázquez SA, et al. Prevalencia de Cáncer de Tiroides en Centros de Referencia del Paraguay. An. Fac. Cienc. Méd. (Asunción) 2020;53(2):67-72 https://doi.org/10.18004/anales/2020.053.02.67 [ Links ]
12. Medina Ruíz BA. Complicaciones post operatorias en la tiroidectomía total por bocio multinodular en el Instituto Nacional del Cáncer. An. Fac. Cienc. Méd. (Asunción) [Internet]. 2014;47(1):33-46. Disponible en: http://scielo.iics.una.py/pdf/anales/v47n1/v47n1a03.pdf [ Links ]
13. Franco López J, Ferreira Bogado M, Samudio Machuca LS. Incidencia de complicaciones post-tiroidectomia total en el Centro Médico Nacional- Hospital Nacional, periodo 2018-2022. Rev. Nac. (Itauguá) [Internet]. 2023;15(1):14-23 https://doi.org/10.18004/rdn2023.jun.01.014.023 [ Links ]
14. Gac EP, Cabané TP, Amat VJ, Huidobro G, Rossi F, Rodríguez FF, et al. Incidencia de hipocalcemia pos tiroidectomía total. Rev. méd. Chile [Internet]. 2007;135(1):26-30. http://dx.doi.org/10.4067/S0034-98872007000100004 [ Links ]
Author’s contribution: MAAW
Participated on substantial contributions of the idea or design of the work, data recollection and studying, literary search, writing of the work and critically revising in search of important intellectual content, critical revision, and final approval. RA: participated on substantial contributions of the idea or design of the work, data recollection, literary search, partial writing of the work and final approval. MDVA: participated on the contribution of the idea, data analysis and graphics and table creation, design and writing of the work, and final approval.
Conflict of interest:
Funding:
Ethical considerations:
Received: June 27, 2023; Accepted: November 24, 2023











 text in
text in