Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Cirugía paraguaya
On-line version ISSN 2307-0420
Cir. parag. vol.47 no.2 Asunción Aug. 2023
https://doi.org/10.18004/sopaci.2023.agosto.39
Case report
Bilateral synchronous parathyroid carcinoma: a case report
1REVITA - Centro Oncológico Integral. Asunción, Paraguay.
Parathyroid carcinoma (PC) is a rare endocrine neoplasm that most commonly occurs in patients with primary hyperparathyroidism, with an incidence of 0.5-4% among patients treated surgically for primary hyperparathyroidism. The diagnosis of PC is challenging as it clinically, radiologically, and histologically overlaps with parathyroid adenoma/hyperplasia. Diagnosis is based on clear evidence of local tissue invasion and/or metastasis. Bilateral PC is rare, and the primary treatment is surgical resection.
Keywords: Bilateral synchronous parathyroid carcinoma; diagnosis; treatment
El carcinoma de paratiroides (CP) es una neoplasia endocrina poco frecuente, ocurre con mayor frecuencia en pacientes con hiperparatiroidismo primario, con una incidencia del 0,5-4% de los pacientes tratados quirúrgicamente por hiperparatiroidismo primario. El diagnóstico de CP es difícil porque se superpone clínica, radiológica e histológicamente con adenoma/hiperplasia de paratiroides, se basa en la evidencia de invasión tisular local inequívoca y/o metástasis. El CP bilateral es anecdótico y el principal tratamiento es la resección quirúrgica.
Palabras clave: carcinoma de paratiroides bilateral; diagnóstico; tratamiento
INTRODUCTION
Parathyroid carcinoma (PC) is a rare neoplasm, with fewer than 1000 cases reported in the literature since its description by De Quervain in 1904. With an estimated prevalence of 0.005% of all cancers, PC is the rarest endocrine cancer, representing 0.5 to 5% of all cases of primary hyperparathyroidism1.
Parathyroid carcinoma occurs equally in both sexes, with an average age of onset between 54 and 56 years2. PC typically presents as an indolent and slowly progressive course. Most patients present with signs and symptoms of primary hyperparathyroidism and hypercalcemia, including nephrolithiasis, nephrocalcinosis, osteopenia, pathological fractures, gastrointestinal disturbances, fatigue, and depression3. Most cases of parathyroid carcinoma are unilateral. Bilateral cases are exceptionally rare, especially in patients without a history of long-term hemodialysis1-2. We present a case of bilateral parathyroid carcinoma without a history of hemodialysis.
CLINICAL CASE
A 63-year-old male patient presented with recurrent nephrolithiasis and renal colic for 3 years prior to consultation. Laboratory data showed PTH 522 pg/ml, total calcium: 13 mg/dl, and calciumuria of 650 mg/24h. Cervical ultrasound revealed two mixed nodular images with cystic areas located behind and below the lower pole of each thyroid lobe, suggestive of parathyroid adenomas. The right side measured 4.5 x 2.5 x 1.6 cm, and the left side measured 4.4 x 2.3 x 2.3 cm. Thyroid nodules classified as Thyroid Imaging Reporting and Data System (TI-RADS) 3 were detected in the right thyroid lobe. The patient expressed a preference for a less invasive method than surgery and received percutaneous ethanol injection for both parathyroid glands. Two months later, laboratory data showed PTH 504 pg/ml, total calcium 12.4 mg/dl, and calciuria 858 mg/24h.
A single-photon emission computed tomography (SPECT) scan with sestamibi revealed a positive gammagraphic pattern for two lower left parathyroid adenomas. (Figure 1)
An ultrasound study indicated an enlarged right thyroid lobe. Additionally, a mixed cystic nodule with regular borders measuring 28 x 21 mm was observed, along with a hypoechoic solid nodule with irregular borders (29 x 17 mm) in the postero-inferior zone and delimited by the thyroid, compatible with a parathyroid nodule. The left thyroid lobe exhibited a mixed nodule measuring 13 mm with regular borders. In the left postero-inferior zone, delimited by the thyroid, another mixed hypoechoic nodule with regular borders measuring 47 x 21 mm was observed, also compatible with a parathyroid nodule. The diagnosis was multinodular goiter and bilateral lower parathyroid nodules. Total thyroidectomy with bilateral parathyroidectomy and resection of bilateral macroscopically lymph nodes at level VI was performed.
Pathological findings showed: 1) Solid right parathyroid tumor measuring 2.5 cm. Microscopically, it was a low-grade infiltrative parathyroid carcinoma, adhered to the thyroid, with extensive stromal fibrosis and capsular invasion (Figures 2 and 3). 2) Solid left parathyroid tumor measuring 1.1 cm. Microscopically, it was a low-grade parathyroid carcinoma with fibrosis and capsular invasion (Figures 4 and 5).
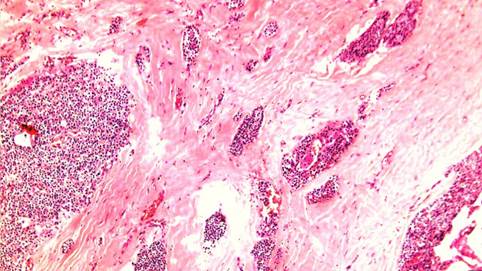
Figure 2. Low-grade parathyroid carcinoma. On the left, solid tumor composed of small cells. In the center and on the left, a thick fibrous capsule with nests of infiltrating carcinoma.
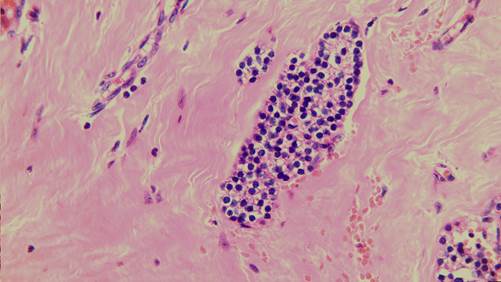
Figure 3. Nest of well-differentiated low-grade carcinoma, round non-atypical cells, without mitosis, indistinguishable from an adenoma except for its infiltrative nature.

Figure 4. Low-grade parathyroid carcinoma. On the left, solid tumor composed of small cells with irregular borders. In the center and on the left, a thick fibrous capsule with infiltrative nests.
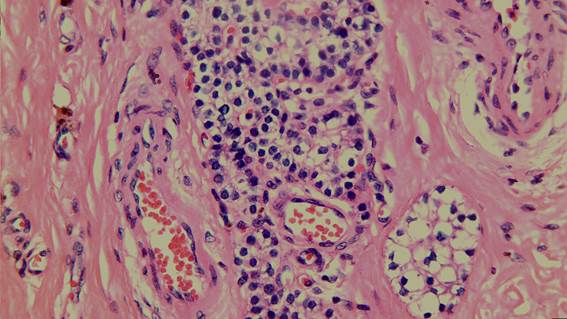
Figure 5. Infiltrative nests of carcinoma, with minimal nuclear atypia, absence of mitosis, peritumoral fibrosis.
The thyroid gland showed changes consistent with benign multinodular goiter. Regional left (4) and right (2) lymph nodes showed no evidence of metastatic carcinoma.
It was classified as a bilateral low-grade parathyroid carcinoma. TNM staging (8th AJCC edition): Right side T2N0M0 and left side T1N0M0.
One month postoperatively, PTH was 4 pg/ml, total calcium was 8.8 mg/dl, no calcium was detected in urine; at the 10-month follow-up, PTH was 3 pg/ml, total calcium was 9.2 mg/dl (January 2023). The patient remains under active surveillance with no evidence of recurrence.
DISCUSSION
Diagnosis of CP is challenging due to its clinical, radiological, and histological overlap with parathyroid adenoma/hyperplasia, and only unequivocal evidence of local tissue invasion and/or metastasis confirms the diagnosis. However, a higher frequency of hypercalcemia symptoms; palpable neck mass; PTH levels exceeding 500 pg/ml; and total calcium levels above 14 mg/dl are suggestive of carcinoma4. The preferred imaging studies for localization are neck ultrasound and sestamibi scintigraphy.4
The etiology of CP remains unknown, and there is no evidence of transformation from pre-existing lesions. Nonetheless, there is an increased risk of parathyroid carcinoma in patients with other endocrine neoplasms such as isolated familial hyperparathyroidism and multiple endocrine neoplasia type 1. Several genetic mutations have been proposed in CP, including retinoblastoma (RB), P53, cyclin D1/gene 1 of parathyroid adenomatosis (PRAD1), and BRCA25.
Surgery remains the only intervention offering the potential for curing parathyroid carcinoma. The primary goal of treatment should be complete removal of parathyroid cancer with negative margins. This includes en bloc resection of the primary lesion, ipsilateral thyroid lobectomy, isthmectomy, tracheal skeletonization, and excision of any adherent muscles. Central lymph node dissection is not indicated prophylactically6.
Ultrasound-guided percutaneous ethanol injection therapy can reduce calcium and PTH levels by up to 45% in parathyroid adenomas, although studies in carcinomas are not well-established7.
While parathyroid adenomas tend to be soft, oval, and reddish-brown in appearance, carcinomas tend to be larger (> 3 cm), white-gray, lobulated, and have a dense fibrous capsule. Adherence or invasion of adjacent structures suggests malignancy. Histological characteristics of parathyroid carcinoma described by Shanz and Castelman include sheets or lobules of tumor cells separated by dense fibrous bands, mitotic figures, necrosis, capsular invasion, and vascular invasion8.
Unfortunately, these classical pathological features are not always present in parathyroid carcinoma. Additionally, some of these characteristics, particularly mitotic figures and trabecular architecture, can also be observed in parathyroid adenomas9. They are categorized as low or high grade based on pleomorphism, nuclear size variation, prominent nuclear membranes, features closer to or distant from adenomas10.
Recent reports have recommended postoperative radiation therapy as a strategy to optimize local control, as it appears to effectively reduce local recurrence rates and improve disease-free intervals. However, due to the rarity of the disease, there are no prospective randomized trials, and most of the knowledge so far comes from case reports and small retrospective series, making the role of adjuvant radiotherapy after surgery still unclear1,11.
Chemotherapy has not been shown to improve survival, disease-free period, or correct hypercalcemia in patients with disseminated or unresectable disease12.
The AJCC 8th edition tumor classification uses the TNM system for staging; however, there is no specific clinical staging. Complete en bloc tumor resection can achieve survival rates of up to 90% at 5 years and 67% at 10 years11. Negative prognostic factors include lymph node metastasis at the time of diagnosis, distant metastasis, non-functioning carcinomas, tumor size, high mitotic rate10.
Despite the best efforts, a significant proportion of patients experience recurrence. Recurrence rates of 33% to 78% have been reported in published studies. Most recurrences will manifest within the first 3 years, but recurrences up to 20 years have been reported. Once the disease has recurred, chances of cure are remote13.
To our knowledge, this is the first reported case of synchronous bilateral parathyroid cancer in Paraguay.
REFERENCES
1. Kassahun WT, Jonas S. Focus on parathyroid carcinoma. International Journal of Surgery. 1 de enero de 2011;9(1):13-9. [ Links ]
2. Lee PK, Jarosek SL, Virnig BA, Evasovich M, Tuttle TM. Trends in the incidence and treatment of parathyroid cancer in the United States. Cancer. 1 de mayo de 2007;109(9):1736-41. [ Links ]
3. Fang SH, Lal G. Parathyroid cancer. Endocr Pract. 2011;17 Suppl 1:36-43. [ Links ]
4. Machado W. Parathyroid Cancer: A Review. Cancers. 28 de octubre de 2019;11(11):1676. [ Links ]
5. Ullah A, Khan J, Waheed A, Sharma N, Pryor EK, Stumpe TR, et al. Parathyroid Carcinoma: Incidence, Survival Analysis, and Management: A Study from the SEER Database and Insights into Future Therapeutic Perspectives. Cancers . enero de 2022;14(6):1426. [ Links ]
6. Givi B, Shah JP. Parathyroid Carcinoma. Clin Oncol (R Coll Radiol). agosto de 2010;22(6):498-507. [ Links ]
7. Yazdani AA, Khalili N, Siavash M, Shemian A, Goharian AR, Karimifar M, et al. Ultrasound-guided ethanol injection for the treatment of parathyroid adenoma: A prospective self-controlled study. J Res Med Sci. 28 de octubre de 2020;25:93. [ Links ]
8. Schantz A, Castleman B. Parathyroid carcinoma. A study of 70 cases. Cancer. marzo de 1973;31(3):600-5. [ Links ]
9. Bondeson L, Sandelin K, Grimelius L. Histopathological variables and DNA cytometry in parathyroid carcinoma. Am J Surg Pathol. agosto de 1993;17(8):820-9. [ Links ]
10. Staging-parathyroid [Internet]. [citado 21 de mayo de 2023]. Disponible en: Disponible en: https://www.pathologyoutlines.com/topic/parathyroidstaging.html [ Links ]
11. Kleinpeter KP, Lovato JF, Clark PB, Wooldridge T, Norman ES, Bergman S, et al. Is parathyroid carcinoma indeed a lethal disease? Ann Surg Oncol. marzo de 2005;12(3):260-6. [ Links ]
12. Schoretsanitis G, Daskalakis M, Melissas J, Tsiftsis DD. Parathyroid carcinoma: clinical presentation and management. Am J Otolaryngol. 2009;30(4):277-80. [ Links ]
13. Sandelin K, Tullgren O, Farnebo LO. Clinical course of metastatic parathyroid cancer. World J Surg. 1994;18(4):594-8; discussion 599. [ Links ]
8Conflict of Interest: The authors declare no conflicts of interest. Funding: Self-funded by the authors.
Received: June 15, 2023; Accepted: August 15, 2023











 text in
text in 




