Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Cirugía paraguaya
versão On-line ISSN 2307-0420
Cir. parag. vol.47 no.1 Asunción abr. 2023
https://doi.org/10.18004/sopaci.2023.abril.22
Original article
Clinical and surgical characteristics of crural hernias in the I Surgical Clinical Chair of Hospital de Clínicas from 2015 through 2021
1Universidad Nacional de Asunción, Facultad de Ciencias Médicas, Hospital de Clínicas. Primera Cátedra de Clínica Quirúrgica. San Lorenzo, Paraguay
Introduction:
Crural hernia is due to a defect of the fascia transversalis, which makes the hernia sac becomes exteriorized in the femoral region. Patients and methods: 32 cases of patients with a diagnosis of crural hernia from the Surgical Clinical Chair at Hospital de Clínicas, Paraguay from 2015 through 2021. This was a retrospective, descriptive, cross-sectional study whose objective is to determine the clinical and surgical characteristics of Crural Hernias in the I Surgical Clinical Chair at Hospital de Clínicas, Paraguay from 2015 through 2021. Results: 78.1% were women. Mean age was 68.1 +/- 14 years, the most common reason for consultation was pain in the inguinocrural region in 56.3% of the patients. In 78.1% of them, pain was confirmed in the right sid. Infrainguinal approach was attempted in 68.8% of the cases. Conclusion: The current challenge is always for the surgeon to achieve an accurate diagnosis and follow the correct course of action in each patient. Since the group of patients diagnosed with crural hernia is limited we should provide them with proper treatment and know all the options available.
Keywords: crural hernia; inguinocrural pain; infrainguinal approach
Introducción:
La hernia crural se produce por un defecto en la fascia transversalis exteriorizándose el saco herniario en la región femoral. Pacientes y métodos: 32 casos de pacientes con diagnóstico de hernia crural en la I Cátedra Clínica Quirúrgica del Hospital de Clínicas entre los años 2015 al 2021. Estudio retrospectivo, descriptivo y transversal que tiene como objetivo determinar las características clínicas y quirúrgicas de las Hernias Crurales en la I Cátedra de Clínica Quirúrgica del Hospital de Clínicas durante el periodo 2015-2021. Resultados: El 78,1% de los pacientes eran mujeres. Media de edad, 68,1 +/- 14 años. El motivo de consulta más frecuente es dolor en región inguinocrural en el 56,3% de los casos. El 78,1% se confirmó en el lado derecho. El abordaje infrainguinal se realizó en un 68,8%. Conclusión: El desafío actual, siempre para el cirujano, es realizar un diagnóstico preciso y un abordaje correcto de cada paciente. Al tratarse de un grupo limitado de pacientes con el diagnóstico de hernia crural debemos ofrecerles el tratamiento adecuado y conocer todas las opciones para la misma.
Palabras claves: hernia crural; dolor inguinocrural; abordaje infrainguinal
INTRODUCTION
Crural hernia is due to a defect in the fascia transversalis, which makes the hernia sac become exteriorized in the femoral region1.
Its incidence rate is somewhere between 5% and 7% with regarding all hernias of the abdominal wall, and it affects mainly women in a 9 to 1 ratio in the ages between 30 and 60 years. Strangulation is the most common complication and occurs 6 to 8 times more often compared to inguinal hernias2,3.
Age, lack of physical exercise, multiple pregnancies, previous surgeries and bed rest are considered predisposing factors as well as all those circumstances increasing intraabdominal pressure4.
Irreducible hernias can be particularly sensitive, especially when there is vascular compromise. Also, in this context, late-onset skin color changes are observed5,6.
Several techniques have been developed for surgical repair of the crural hernia. Placing a mesh plug is the procedure of choice (81%). Closure using classic techniques is only preferred by 15% of surgeons. In addition, 77% say that the mesh procedure should always be adjusted to the measure of the hernia orifice7,8.
Infrainguinal approach using a mesh plug has gained popularity thanks to its simplicity and short procedural time9.
As a result of its low incidence rate, there are relatively few clinical studies on crural hernias. The largest series ever published to this date comes from the Swedish Hernia Register. It includes 588 patients who were treated in a 6-year period at 29 different centers with a mean of 3.4 per hospital per year. The Shouldice Hospital specializes in the management of abdominal wall hernias. Here over 7500 repairs are performed each year. Although crural hernias account for just 2.1% of all repairs reported, the cumulative volume represents an unprecedented experience10,11.
Crural hernia is not very common. However, it is important to know this condition since its timely diagnosis and treatment improve the results of surgery and the patients’ quality of life.
It is important to have a detailed registry of patients treated with crural hernia to be able to consider actions to improve the patients’ wellbeing. Therefore, this study was proposed to try to determine the clinical and surgical characteristics of crural hernias in the I Surgical Clinical Chair at Hospital de Clínicas in San Lorenzo, Paraguay from 2015 through 2021.
MATERIALS AND METHODS
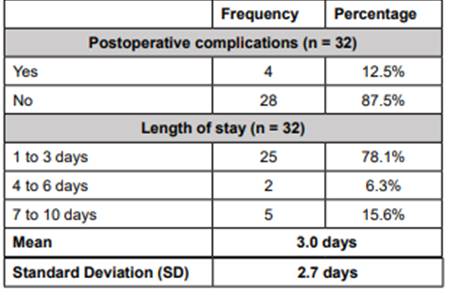
This was an observational, descriptive, cross-sectional, and retrospective study with non-probabilistic sampling of consecutive cases. This was a review of the medical records available in our unit within the I Surgical Clinical Chair at Hospital De Clínicas, San Lorenzo, Paraguay from 2015 through 2021. The series includes 32 patients with a diagnosis of crural hernia. A total of 78.1% were women and mean age was 68.1 +/- 14 years. (Table 1)
Inclusion criterion
We included the complete record of patients of both sexes, over 18 years of age with a diagnosis of crural hernia admitted to the I Surgical Clinical Chair at Hospital de Clínicas in San Lorenzo, Paraguay.
Variables
Sex
Age
Origin
Occupation
Comorbidities
History of abdominal surgery
Main reasons for consultation
Location of crural hernia
Type of surgery
Evolution of disease
Surgical approach
Kelotomy
Groin ligament incision
Sac content
Ischemic distress
Anastomosis resection
Postoperative diagnosis
Type of surgery performed
Procedural time
Postoperative complications
Postoperative length of stay
RESULTS
A total of 32 patients were studied with a diagnosis of crural hernia at the I Surgical Clinical Chair of Hospital de Clínicas in San Lorenzo, Paraguay between the years 2015 and 2021. A total of 78.1% were women, 50% of them were at an age between 61 and 80 years. The mean age was 68.1 +/- 14 years. A total of 75% came from the Central Department while 63% of the patients were housewives (Table 1).
Table 1. Personal information (sex, age, origin, occupation) of the patients diagnosed with crural hernia at the I Surgical Clinical Chair
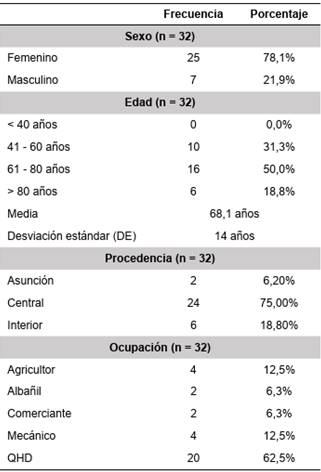
Regarding personal past medical history, we found that 39.6% had high blood pressure (HBP), 18.9% had more than one underlying condition, and 17% did not know they had such underlying disorder. A total of 75% did not have a past surgical history (Table 2).
Table 2. Underlying disorder and previous surgeries of patients diagnosed with crural hernia at the I Surgical Clinical Chair
COPD, chronic obstructive pulmonary disease; HBP, high blood pressure; type 2 DM, diabetes mellitus type 2.
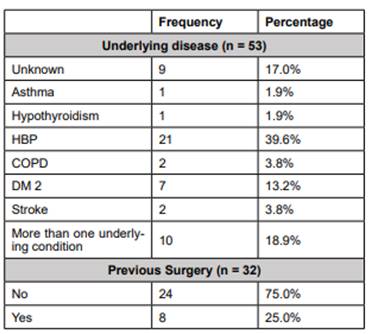
Among the most common reasons for consultation we find, by order of frequency, pain in the inguinocrural region in 56.3%, tumor in the inguinocrural region in 31.3% and distended abdomen in 12.5%. In 78.1% of the cases, the presence of crural hernia on the right side was confirmed. Regarding the surgeries performed, 81.3% were emergency surgeries. The most common time of disease progression was between 12 and 24 hours in 58.3% of the cases with a mean of 27.1 +/- 13.3 hours (Table 3).
Table 3. Reason for consultation, location of crural hernia, type of surgery, and disease progression time in the emergency surgeries of patients diagnosed with crural hernia at the I Surgical Clinical Chair.
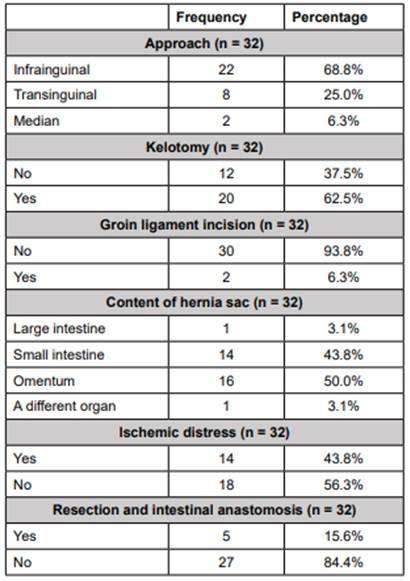
Regarding the access route, all of them were conventional surgeries. Infrainguinal access route was the most common access route being reported in 68.8% of the cases, kelotomy in 62.5% while in 6.3% groin ligament incision was performed. It was found that the most common sac content was the presence of omentum in 50% of the cases followed by the small intestine in 43.8%. One of the cases reported the presence of the bladder and in yet another the presence of the large intestine with the cecal appendix. In 43.8% of the cases the presence of ischemic distress was confirmed, and 15.6% required resection with intestinal anastomosis (Table 4).
Table 4. Surgical approach, kelotomy, groin ligament incision, sac content, ischemic distress and resection, and intestinal anastomosis of patients diagnosed with crural hernia at the I Surgical Clinical Chair
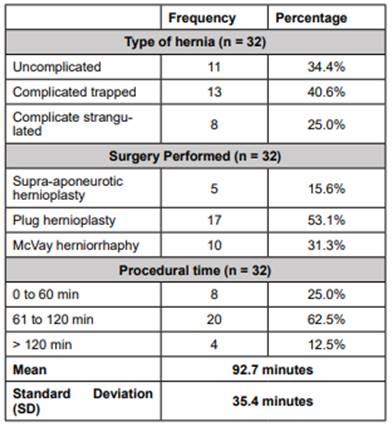
A diagnosis of complicated, trapped crural hernia was achieved in 40.6% of the cases followed by uncomplicated crural hernia in 34.4%, and complicated strangulated crural hernia in 25%. The most common surgery performed was hernioplasty with placement of prosthetic mesh plug in 53.1%. The most common surgical time was 61 to 120 minutes in 62.5% of the cases with a mean of 92.7 +/- 35.4 minutes (Table 5).
Table 5. Type of hernia, surgery performed, and procedural time of patients diagnosed with crural hernia at the I Surgical Clinical Chair
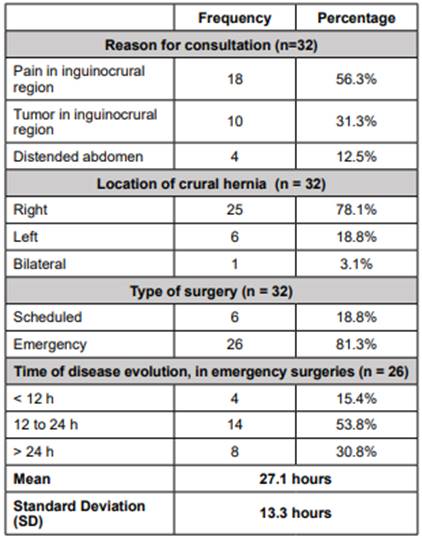
A total of 12.5% had postoperative complications such as paralytic ileus, in-hospital pneumonia (IHP), and wall abscess. The mean length of stay was 3 +/- 2.7 days (78.1% between 1 and 3 days) (Table 6).
DISCUSSION
In this work a total of 32 patients are reported with a diagnosis of crural hernia in the period between 2015 and 2021 at the I Surgical Clinical Chair of Hospital De Clínicas, San Lorenzo, Paraguay. Based on sex distribution, it was observed that 78.1% of the patients were women. Ohkura et al. reported a predominance of women in 78% of the population. The frequency of women is clear and this is especially due to anatomical factors, although there are publications that recorded a growing tendency of crural hernias among men3,7,8.
The most common age is between 61 and 80 years in 50% of the cases, and the study recorded a mean age of 68.1 +/- 14 years. The study published by Ohkura et al. reported a mean age over 66 years and a range between 48 and 95 years while the study published by Sanz et al. reported a mean age of 59 years. Most patients originally came from the Central Department, which is the department with the largest population in Paraguay6,18.
The most common occupation is being full-time housewives which concerns women who do this work and depending on the tasks they do, they make different kind of efforts of that increase intraabdominal pressure and make these patients be prone to have some type of hernia, in this case a crural hernia4.
In this study, as in literature reviews, we find that patients with crural hernias show underlying conditions like high blood pressure in 39.6%, and conditions that elevate intraabdominal pressure like in the case of patients with chronic obstructive pulmonary disease (COPD) and asthma, in addition to patients with previous abdominal surgeries associated with a predisposition to crural hernia5) .
Among their main reasons for consultation, patients mention the following in order of frequency: pain in the inguinocrural region in 56.3%, tumor in the inguinocrural region in 31.3%, and distended abdomen in 12.5%. No differences are observed regarding the patients’ main reasons for consultation compared to international statistics9,19.
This study comes close in statistics to other publications regarding disease progression among patients with crural hernia who presented with urgent symptoms. The most common disease progression time found was between 12 and 24 hours with an mean of 27.1 +/- 13.3 hours.12
Regarding the need for surgery, 81.3% of them underwent emergency surgery. The study published by Sanz et al. reports a frequency of patients undergoing emergency surgery of 28%9,11.
Regarding the surgical approach, infrainguinal approach was performed in 68.8% of the patients. We found that the study conducted by Sanz et al. reported the use of the transinguinal technique in the all their patients with good results7.
As in international publications, we found similar results in which kelotomy was performed in 62.5%. Only 6.3% underwent groin ligament incision, and the most common sac content found was the presence of omentum and small intestine (50% and 43.8%, respectively) (13.
As mentioned in some publications with results similar to ours, the presence of ischemic distress was confirmed in 43.8% of the cases, of which only 15.6% required resection - intestinal anastomosis and the rest was solved through physical means14.
Complicated trapped crural hernia was the most common diagnosis found in 40.6% of the patients from our study. Unlike this study, most publications reviewed report overall complication rates < 30%. Trapped crural hernias can have, or not, distress fluid without vascular compromise. However, in a strangulated hernias, in addition to distress fluid, we find vascular compromise which in most cases will eventually require resection with anastomosis15.
We should mention that one of the complications of crural hernias is intestinal strangulation, hence the importance of timely diagnosis and treatment to prevent necrosis and intestinal resection16.
A total of 15.6% of the patients who underwent hernioplasty required placement of a supra-aponeurotic polypropylene mesh, 53.1% of crural hernias required repaire with a prosthetic plug and herniorrhaphy using the McVay Technique in 31.3%. The study conducted by Pasto et al. reported the greatest frequency of repairs with prosthetic plugs and repairs with the McVay technique in 3% of the cases. Our review is consistent with these publications where we find that the most common procedural time was somewhere between 61 and 120 minutes in 62.5% (mean, 92.7 +/- 35.4 minutes)20.
Regarding postoperative complications, it was reported that 12.5% of patients showed some kind of complications following the surgery such as paralytic ileus, IHP, and wall abscess. In most patients we found lengths of stay between 1 and 3 days (mean, 3 +/- 2.7 days). Martínez et al. reported similar mean rates of postoperative complications of 16.6% lengths of stay of 2.5 days11,17
CONCLUSION
Most of our patients were women, with an mean age of 68 years; most came from the Central Department, their main occupation was being full-time housewives, and their most common comorbidities HDP, COPD, and asthma. Most patients did not report any previous surgeries being the main clinical sign inguinocrural pain, and a mean disease progression time of 27.1 hours among patients with crural hernia that presented with emergency signs and symptoms.
The main diagnosis was complicated trapped crural hernia and the most widely used surgical technique used was hernioplasty with prosthetic plug. Surgeries lasted a mean 92.7 minutes.
Most patients underwent emergency surgery with a diagnosis of right crural hernia being the infrainguinal approach the most common one. In most cases kelotomy was performed and in very few cases groin ligament incision. In most cases the sac contained omentum and thin loops. In addition, the presence of ischemic distress was confirmed, which in most cases did not require resection - intestinal anastomosis.
Regarding postoperative complications, a low percentage of paralytic ileus and IHP was reported. In addition, it can be concluded that the mean length of stay was 3 days.
The current challenge for the surgeon is always to achieve an accurate diagnosis and follow the correct course of action in each patient. Since this is a limited group of patients with a diagnosis of crural hernia we should provide them with the correct treatment and know all the treatment options available.
REFERENCES
1. Townsend JR, Courtney M. et al. Sabiston tratado de cirugía: a base biológica da prática cirúrgica moderna. 20.ed. Rio de Janeiro: Elsevier, 2019. p. 1104. [ Links ]
2. Jeyarajah DR, Dunbar KB. Abdominal hernia and gastric volvulus. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021: chap 27. Disponible en: https://ufhealth.org/femoral-hernia [ Links ]
3. Kichler K, Gomez CO, Lo Menzo E, Rosenthal RJ. Abdominal wall and abdominal cavity hernias. In: Floch MH, ed. Netter's Gastroenterology. 3rd ed. Philadelphia, PA: Elsevier; 2020: chap 48. Disponible en: http://thnm.adam.com/content.aspx?productid=617&pid=1&gid=001136 [ Links ]
4. Malangoni MA, Rosen MJ. Hernias. In: Townsend CM, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 20th ed. Philadelphia, PA: Elsevier; 2017: chap 44. Disponible en: https://ufhealth.org/ventral-hernia-repair [ Links ]
5. Reynolds JC, Ward PJ, Rose S, Solomon M. Small bowel. In: Reynolds JC, Ward PJ, Rose S, Solomon M, eds. Netter Collection of Medical Illustrations: Digestive System: Part II - Lower Digestive Tract, The. 2nd ed. Philadelphia, PA: Elsevier; 2017:31-114. Disponible en: https://www.elsevier.com/books/the-netter-collection-of-medical-illustrations-digestive-system-part-ii-lower-digestive-tract/reynolds/978-1-4557-7391-6 [ Links ]
6. Jm C. Hernies crurales définition et traitement. Soins Chir. 2013;45-7. Disponible en: http://scielo.iics.una.py/scielo.php?script=sci_nlinks&pid=S2307-0420202100010001200001&lng=en [ Links ]
7. Gold BI, Cáceres Arana, Moscoso N, Navarro Vásquez PB. Tratamiento laparoscópico de la hernia inguinal. Rev Cient Arte Cienc Medica. 2014; 5(4). Pp 18-29. Disponible en: https://www.asacirujanos.com/admin/upfiles/revista/2018/Cir_Andal_vol29_n2.pdf [ Links ]
8. Fina R, Rafael J, Fernández M, JE, Rabassa C, Pablo P, et al. Uso de bioprótesis en las hernias inguinocrurales complicadas. Rev Cuba Cir 2013;2(4).Pp 45 - 55. Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0034-74932003000200009 [ Links ]
9. Rubilar OP, Jarufe CN, Guridi GR, Sahid ZS, Reyes MG. Hernioplastias con prótesis de polipropileno: experiencia del Hospital Clínico San Borja-Arriarán. Rev Chil Cir. 2011; 51-5. Disponible en: https://pesquisa.bvsalud.org/portal/resource/pt/lil-211877 [ Links ]
10. Mayagoitia González JC. Hernias de la pared abdominal, tratamiento actual. Hernia femoral. 3ra.ed. México. Editorial Alfil. SA, 2015. p. 517. [ Links ]
11. Rodríguez JI. Propuesta de estándar asistencial en la reparación de la hernia inguinal o crural. Cir Esp Ed Impr. 2013; 73: 331-5. Disponible en: https://hernia.grupoaran.com/magazines/filesPortalWeb/23 [ Links ]
12. Meilán-Martínez A, Argüelles-García B, Anes-González G, Rodicio Miravalles JL. Obstrucción intestinal secundaria a hernia crural incarcerada. Cir Esp. 2014.; 83(1).Pp 345-55. Disponible en: http://scielo.iics.una.py/scielo.php?script=sci_nlinks&pid=S2307-0420202100010001200010&lng=en [ Links ]
13. Bustos NS, Santanciero SR, Minotto PC, Romero SF. Herniorrafía laparoscópica sin malla. Rev Chil Cir. 2016;506-8. Disponible en: https://www.scielo.cl/scielo.php?script=sci_arttext&pid=S0718-40262016000600009 [ Links ]
14. Pastó Pomar E, Lalán G MJ, Pardo Olivares E, Tuero G, Humberto J. Hernioplastias en las complicaciones agudas de las hernias inguinocrurales. Medisan 2016 Jul 6; 3(1). 56-60. Disponible en: https://www.redalyc.org/pdf/3684/368444988003.pdf [ Links ]
15. Madden M, Dorian M. Hernies crurales: techniques de réparation. J Chir Paris. 2012; 5(3). Pp 15-18. Disponible en: http://scielo.iics.una.py/scielo.php?script=sci_nlinks&pid=S2307-0420202100010001200013&lng=en [ Links ]
16. Rian S, Yenh D. Hernies crurales, leur étranglement et leur traitement chirurgical. Chirurgie. 2015;834-8. Disponible en: https://www.science.gov/topicpages/c/chez+les+enfants.html [ Links ]
17. Echeverria I, Lira Soto N. Hernias inguinocrurales: evaluación de la técnica del Dr. Ivan Humpierres H. Bol Méd Postgrado. 2011; (1) 2. Pp 22-7. Disponible en: http://scielo.iics.una.py/scielo.php?script=sci_nlinks&pid=S2307-0420202100010001200015&lng=en [ Links ]
18. Abraham Arap J. Hernias inguinales y crurales (hernias de la ingle). Rev Cuba Cir. 2010;2(3). Pp 234-235. Disponible en http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0034-74932009000200010 [ Links ]
19. Aguilar Valdés J, Maurant Mallo E, Mazorra Romero A, García Caballero O. Morbilidad por síndrome oc|lusivo de intestino delgado. Arch Méd Camaguey. 2010;8(2). Pp 67-70. Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1025-02552001000200012 [ Links ]
20. Frering V, Gignoux B, Duchamp C, Blanchet MC, Darnis B, Amblard I. Hernie crurale a Lyon - Synmtomes et traitement. 2019. Disponible en: https://www.chirurgien-digestif.com/hernie-crurale [ Links ]
Authors’ contribution: All the authors participated in the search for information, data collection, drafting, critical revision of the manuscript, and final approval.
Received: November 30, 2022; Accepted: February 21, 2023











 texto em
texto em