Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Cirugía paraguaya
versão On-line ISSN 2307-0420
Cir. parag. vol.47 no.1 Asunción abr. 2023
https://doi.org/10.18004/sopaci.2023.abril.16
Original article
Characterization of right colectomies due to oncological pathologies according to the approach route in the general surgery service of the IPS Central Hospital, in the period 2018-2020
1Hospital Central del Instituto de Previsión Social. Asunción, Paraguay.
Introduction:
Colorectal cancer is the most common malignant neoplasm of the digestive tract. More than 95% corresponds to adenocarcinoma. The incidence is similar in men and women. In the General Surgery Service of the IPS Central Hospital, a large number of right colectomies are performed electively for neoplastic pathologies.
Objective:
To describe the clinical, surgical and anatomopathological characteristics of colonic resections with oncological margin according to the approach route performed in the context of tumor pathologies of the right colon, at the IPS Central Hospital, 2018-2020.
Methodology:
A descriptive, retrospective, cross-sectional observational study was carried out. Results: 115 patients were included, the average age was 64.2 years, 55.7% female and 88.0% presented Adenocarcinoma. Regarding the approach route for colonic resection with oncological margin, in 76% it was conventional; in 6.9% by conventional route, they presented suture dehiscence and 4.6% died. The mean number of nodes resected was 18.8 ±9.9. It was found that 89.0% of those who underwent laparoscopic surgery had a hospital stay of 1-10 days and 85.0% conventional surgery. Conclusion: The average age was 64 years and the female sex predominated. The most frequent anatomopathological diagnosis was Adenocarcinoma; the most commonly used approach was the conventional one. The most frequent post-surgical complication was suture dehiscence, which occurred in a higher percentage in those patients with a conventional approach, and the hospital stay was longer in patients operated using a conventional approach.
Key words: Colon cancer; colectomy; laparoscopic surgery
Introducción:
El cáncer colorrectal es la neoplasia maligna más común del tubo digestivo. Más del 95% corresponde a adenocarcinoma. La incidencia es similar en varones y mujeres. En el Servicio de Cirugía General del Hospital Central del IPS,se realizan de forma electiva un gran número colectomías derechas por patología neoplásica.
Objetivo:
Describir las características clínicas, quirúrgicas y anatomopatológicas de las resecciones colónicas con margen oncológico según vía de abordaje realizadas en el contexto de patologías tumorales del colon derecho, en el Hospital Central IPS, 2018-2020.
Resultados:
Se incluyó a 115 pacientes, el promedio de edad fue 64,2 años, el 55,7% de sexo femenino y el 88,0% presentó adenocarcinoma. En cuanto a la vía de abordaje para la resección colónica con margen oncológico, en el 76% fue convencional, en el 6,9% por vía convencional, presentaron dehiscencia de sutura y el 4,6% fallecieron. La cantidad promedio de ganglios resecados fue de 18,8 ± 9,9. Se constató que el 89,0% de los intervenidos por vía laparoscópica presentaron una estancia hospitalaria de 1-10 días y el 85,0% por vía convencional.
Conclusión:
El promedio de edad fue de 64 años y predominó el sexo femenino. El diagnóstico anatomopatológico más frecuente fue el Adenocarcinoma; la vía de abordaje mayormente realizada fue la convencional. La complicación post quirúrgica más frecuente fue la dehiscencia de sutura, la cual se presentó en mayor porcentaje en aquellos pacientes con vía de abordaje convencional, y la estadía hospitalaria fue mayor en los pacientes intervenidos según vía de abordaje convencional.
Palabras clave: Cáncer del colon; colectomía; cirugía laparoscópica
INTRODUCTION
Colorectal cancer is identified among the most common malignant neoplasms of the digestive tract. Over 95% of the cases can be categorized as adenocarcinomas. Its incidence rate is similar in men and women and has remained relatively constant over the past 20 years. Regarding its location, adenocarcinoma at right large intestine location predominates over the left location. Currently, it is a significant problem of public healthcare in developed countries. This type of cancer ranks fourth among the most common types of cancer worldwide1,2.
Since the preliminary stage of colon cancer is, in many cases, an adenomatous polyp, all colon polyps must be removed entirely if they have carcinoma in situ (high-grade or serious dysplasia) during an endoscopic polypectomy. However, they do not require any additional treatment. The scar of the excision can be tattooed with ink so the surgeon can locate the area to be resected3.
The proper staging of oncological pathology is determined, to a large extent, by the nodes resected in the course of the surgical procedure, which according to the latest classification of the Union for International CancerControl (UICC) it was proposed to be 12 nodes. Lymph node dissection conditions prognosis and justifies the complementary treatments4.
Surgery is identified as the main treatment for colorectal cancer depending on its location and stage. Intestinal reconstruction is performed by latero-lateral, termino-lateral or termino-terminal ileocolic anastomosis either manually or through mechanic suture, the results being similar. In case this condition shows obstruction or perforation, the prognosis becomes more complex and its therapeutic management varies with a rate of acute colon obstruction5,6 between 60% and 90%.
To achieve satisfactory results in terms of patient recovery and oncological safety, some principles should be observed. First, the choice of the access route depends on the patient, the characteristics of the tumor and the surgeon’s experience. If a large tumor (> 7 cm) needs to be resected or is adhered to adjacent structures and en bloc resection is necessary, classic surgery is advised. As the surgeon gains more experience, his capacity to treat larger or more complex tumors facilitates solving more cases via laparoscopy7,8.
Conversion to classic surgery occurs between 7% and 29% of the cases including uncontrollable bleeding, tumor invasion, and organ damage, among others. Research has shown that patients who are passed on to surgery do not show worse evolution than those who undergo surgery via traditional route, which is why authors promote and recommend laparoscopic surgery to all patients without a formal contraindication9,10.
Depending on the location of the tumor, resections consist of left hemicolectomy, right hemicolectomy, transversectomy, sigmoidectomy, low anterior resection, ultra-low anterior resection and abdominoperineal or Miles’ amputation. They can be performed either through conventional or laparoscopic approach11.
Right colectomy for cancer treatment is the resection of the terminal ileum, the ascending colon, the right region of the transverse colon, and the entire lymph node drainage area that is located on the right side of the superior mesenteric axis. Although it was originally described as an open approach, after it was introduced, the laparoscopic approach has demonstrated to be better in terms of less morbidity and mortality with similar oncological outcomes compared to conventional surgery12.
The laparoscopic approach has all the benefits associated with less parietal aggression, such as evisceration or ratio of events. In addition to minimizing the risk of accidents associated with direct manipulation of viscera. It allows the decollation of all the sectors of the colon turning it into a completely mobile organ that can be removed through small incisions that can be used for mesogastrium ligation, resection, anastomosis, and removal of the target segment. Currently, laparoscopic colorectal resection is a common surgical procedure all over the world, and whenever possible, the method of choice to treat colorectal tumors13-15.
The length of stay of colorectal surgical resection can be up to 11 days with a rate of complication up to 48% in elective surgeries with conventional perioperative management even despite the laparoscopic approach16. Most cases of hemicolectomies are well-tolerated by the patients despite a transient increase in the frequency of bowel movements. This procedure has minor physiological consequences. On the other hand, proctocolectomies or total colectomies are associated with much more short- and long-term complications, many of which are directly associated with ileostomy reconstruction to restore intestinal transit17.
The early complications associated with ileoanal anastomosis with ileostomy following a colectomy include anastomotic leaks occurring in, approximately, 1% of the cases, stenosis at the site of anastomosis (11%), pelvic sepsis, and abscesses within the ileostomy (5% and 20%, respectively). Finally, it is estimated that in 30% of patients pouch will fail with mortality rates around 3%. 18) The long-term consequences of ileal pouch surgery include incontinence with an average frequency of 25% approximately. Fertility is a relevant consideration in patients with ileal pouches19.
For the procedure to be successful, we should mention that several factors determine success, among them, the surgeon’s training, the volume of patients hospitalized, the topography of the tumor in the colon, the patient’s age, the stage of the tumor, and its clinical presentation20.
The objective of this study was to describe the clinical, surgical, and anatomopathological characteristics of colon resections with tumor margins depending on the access route used in the context of tumor diseases of the right colon at the Central IPS Hospital from 2018 through 2020.
MATERIAL AND METHODS
This was a descriptive, cross-sectional, observational study with retrospective data. Target population: colon cancer patients. Accessible population: Colon cancer patients treated at the General Surgery Unit of IPS Central Hospital from 2018 through 2020. Inclusion criteria: adults, both sexes treated with surgery at the General Surgery Unit of IPS Central Hospital from 2018 through 2020. Exclusion criteria: clinical, surgical and anatomopathological health records with incomplete data. Observation and analysis unit: clinical, surgical, and anatomopathological health records registered at the Hospital Computer System (HCS). Study variables: age, sex, anatomopathological diagnosis, access route, type of complication, lymphadenectomy, length of stay.
Data collection tools: database was uploaded from January 2018 through to December 2020 in an Excel spreadsheet specially made for this purpose including the study variables. Data collection methods: after the research protocol was approved with the corresponding authorization to access the health records registered in the Hospital Computer System (HCS). Data were entered by the person in charge of the study from January 2018 through December 2020 including both the inclusion and the exclusion criteria in an Excel spreadsheet. Statistical analysis: descriptive statistics was applied with summary measures based on distribution, frequency table, and sector and bar charts. Both the mean and the standard deviation were estimated regarding discrete variables. Regarding qualitative variables, both frequency and percentage were estimated. The software used for the analysis for data analysis was Excel 2016 and Software Stata.
Quality control: the study data were entered following a pre-established spreadsheet, and controlled by the author of the research to prevent any mistake from being made during the data input. A preliminary analysis was conducted to make sure data would be entered correctly.
Ethical aspects: Authorization was requested from the Head of the General Surgery Unit to be able to use the database. The confidentiality of personal data was safeguarded by using a number code that identified each health record (only known by the researcher). Informed consent was not deem necessary. However, the protocol was evaluated by the IPS Central Hospital Research Ethics Committee. Prior to that, approval of the research proposal was obtained by this Committee.
RESULTS
The study included 115 patients with colon cancer treated at the IPS Central Hospital General Surgery Unit from 2018 through 2020. Their meaan age was 64.2 ±13.9 years, 55.7% of them were women, and 44.3% men.
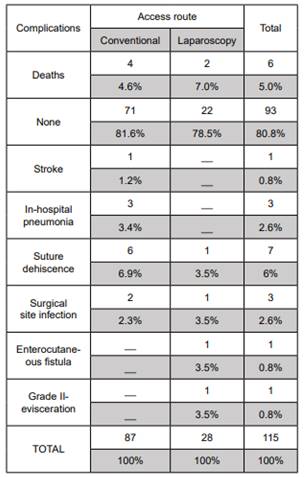
Regarding the anatomopathological diagnosis of the study population, adenocarcinoma was confirmed in 88.0% of the patients followed by adenoma (3.0%) and adenosquamous carcinoma (3.0%) (Chart 1).
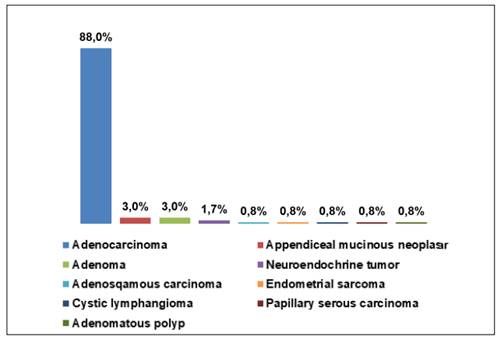
Chart 1. Study population based on the anatomopathological diagnosis achieved. Patients with colon cancer patients treated at the IPS Central Hospital General Surgery Unit from 2018 through 2020.
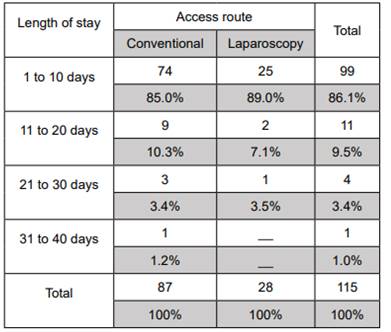
Regarding the access route for colon resection with tumor margins in the study population, it was confirmed that 76% of all resections were performed via conventional access compared to 24.0% that were performed via laparoscopy (Chart 2).
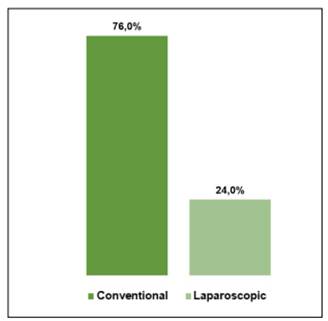
Chart 2. Study population according to the access route for colon resections with tumor margins. Patients with colon cancer patients treated at the IPS Central Hospital General Surgery Unit from 2018 through 2020.
Regarding postoperative complications based on the access route used in patients who underwent right colectomy it was confirmed that 6.9% of those who underwent surgery via conventional access showed suture dehiscence while 4.6% died (Chart 3).
The mean number of nodes resected according to the protocol established for lymphadenectomies in right colectomies due to tumors was 18.8 ± 9.9. It was confirmed that 89.0% of the patients treated with surgery via laparoscopy had lengths of stay of 1-10 days compared to 85.0% of the patients treated with surgery via conventional access. We should mention that the time period of 11 to 40 days occurred more often among patients treated with conventional access compared to those treated with laparoscopy (Chart 4).
DISCUSSION
After processing the data from the 115 patients with colon cancer treated with surgery with an indication for colon resections with tumor margins, a mean age of 64.2 ±13.9 years was reported, 55.7% of whomewere women and 44.3% men.These results differ from the study conducted by Domínguez and Sirtori 12) in which men were more prevalent in the sample studied with 53.1% being the mean age, 66.4 ± 14.7 years. Also, it was different from the study conducted by Rodríguez Infante 19) in which 69.2% of the patients treated with surgery were men and 30.8% women. The mean age was 69 years of age.
On the other hand, the study conducted by Sánchez Gallego et al.9 also demonstrated that men predominant in 57.1% of the cases. However, regarding mean age (65 ±78) it was observed that it was similar to our study.
Regarding the anatomopathological diagnosis of the study population, adenocarcinoma was observed in 88.0% of the patients followed by adenoma (3.0%), and adenosquamous carcinoma (3.0%), which is consistent with what the study conducted by Domínguez and Sirtori reported12 in which 84.4% of the tumors found were adenocarcinomas.
Regarding the access route for colon resection with tumor margins in the study population, it was seen that 76% of the cases were performed via conventional access and 24.0% via laparoscopy, which revealed that the former was predominant. This is consistent with what the 468-patient study conducted by Rodríguez Infante found, 19) that 13.8% of the patients underwent surgery via laparoscopy while 86.2% did so via conventional access.
Domínguez and Sirtori12 mention that the benefits of minimally invasive surgery has been widely described in the medical literature. Regarding its use to treat colorectal cancer, this management was first described back in 1990. However, throughout the first decade following it was first described, it was questioned due to the feasibility of this approach associated with colorectal cancer with high rates of tumor recurrence, metastasis in trocar orifices, difficulty detecting synchronic tumors and inadequate oncological resections. This, added to the technological delay of developing countrieshas hindered the boom of this technique in other diseases. However, over the past few years, multiple studies that demonstrated the efficacy and safety profile of this procedure to treat colorectal cancer. Also, that the complications described at the beginning were due to the use of inadequate surgical techniques and/or ignorance both in the theoretical and practical aspects of colorectal cancer surgery rather than the laparoscopic approach per se.
Taking into account what is mentioned by these authors and the results revealed by the present study, it is important to know the reason why the conventional route is used more in general surgery services, despite the fact that there is scientific evidence that supports the laparoscopic technique as being efficacious in the surgical treatment of colorectal cancer.
A total of 80% of the population studied did not show any complications. However, it was observed that among the postoperative complications reported based on the access route used 6.9% of those who underwent surgery via conventional access showed suture dehiscence and 4.6% died. This was more prevalent than what was seen among patients treated via laparoscopy, which is somehow similar to the results from the study conducted by Castro and Ramírez et al. 17) where most of the 107 patients treated with colon resection showed no complications of any kind. However, in patients who did show complications, it was seen that surgical infection was the most common complication of all, which is not consistent with our study.
On the other hand, the study conducted by Vivanco Armijos 7) revealed that the rate of laparoscopic complications was 2.3% as opposed to 9.4% in the surgeries performed via conventional route, which is, in fact, consisent with our study.
Based on their own results, González-Valverde 18) mention that there is a higher risk of showing anastomosis dehiscence if surgery extendes for over 180 min and that access route, surgical technique used, and age do not play a role in the development of this complication. It was not possible to confirm such a claim in our study since data on the surgical time of patients treated could not be access. Therefore, it would be a good idea to try to demonstrate this hypothesis in similar studies.
The mean number of nodes resected according to the protocol established for lymphadenectomies in right colectomies due to tumors was 18.8 ± 9.9. This result is consistent with what the study conducted by Domínguez and Sirtori found12 where > 10 nodes were resected in 59.4% of the population. Similarly, in most patients included in the study conducted by Vivanco Armijos 7) more than 10 nodes were resected.
It was confirmed that 89.0% of the patients who underwent surgery via laparoscopy remained hospitalized for 1-10 days compared to 85.0% of the patients treated via conventional route. We should mention that stays of 11 to 40 days were more common in patients treated via conventional route compared to those treated via laparoscopy. This result is somehow similar to that reported by the study conducted by Domínguez and Sirtori12 since the length of stay of 50% of the patients operated via laparoscopy was somewhere between 5 and 6 days. In 43.7% of the patients this length of stay as < 4 days.
CONCLUSIONS
The mean age of the study population was 64 years (women predominantly). The most common anatomopathological diagnosis in the population was adenocarcinoma followed by adenoma and adenosquamous carcinoma. Access route mostly used in these patients for colon resection with oncological margin was the conventional one. The most common postoperative complication was suture dehiscence that occurred mostly in patients treated via conventional approach. The mean number of nodes resected according to the protocol established for lymphadenectomies in right colectomies due to tumors was 18. Length of stay was longer in patients treated with surgery through conventional approach.
REFERENCES
1. Zúñiga Ávalos D. Proceso de cuidado enfermero perioperatorio en paciente sometido a resección de intestino grueso [Internet] [Tesis de Especialidad]. [San Luis Potosí]: Universidad Autónoma de San Luis Potosí; 2017 [citado 14 de octubre de 2021]. Disponible en: Disponible en: https://repositorioinstitucional.uaslp.mx/xmlui/handle/i/4594 [ Links ]
2. Cerdas Soto L. Caracterización clinicoepidemiológica de los pacientes con cáncer colorrectal intervenidos en el Hospital San Rafael de Alajuela. Revisión bibliográfica sobre el Cáncer Colorrectal y su abordaje comparado con el realizado en el Hospital San Rafael de Alajuela [Internet] [Tesis de Especialidad]. [Costa Rica]: Universidad de Costa Rica; 2021 [citado 15 de octubre de 2021]. Disponible en: Disponible en: https://www.kerwa.ucr.ac.cr/handle/10669/84233 [ Links ]
3. Corral de la Calle MA, Encinas de la Iglesia J. Ecografía de la patología infecciosa y tumoral del intestino y el peritoneo. Radiología. 2021;63(3):270-90. [ Links ]
4. Lara Perlaza LM. Análisis del tratamiento quirúrgico en pacientes con adenocarcinoma de recto localmente avanzado sometidos a neoadyuvancia preoperatoria en el ION -SOLCA Guayaquil período 2013 - 2016 [Internet] [Tesis de Especialidad]. [Guayaquil]: Universidad de Guayaquil; 2018 [citado 14 de octubre de 2021]. Disponible en: Disponible en: http://repositorio.ug.edu.ec/handle/redug/39147 [ Links ]
5. 2015 European Society of Coloproctology Collaborating Group. Predictors for Anastomotic Leak, Postoperative Complications, and Mortality After Right Colectomy for Cancer: Results From an International Snapshot Audit. Dis Colon Rectum. 2020;63(5):606-18. [ Links ]
6. Lohsiriwat V. Learning curve of enhanced recovery after surgery program in open colorectal surgery. World J Gastrointest Surg. 2019;11(3):169-78. [ Links ]
7. Vivanco Armijos HB. Impacto en la morbilidad de la técnica quirúrgica abierta vs cerrada en cáncer de colon en Solca Quito, periodo marzo 2012 a marzo 2017 [Internet] [Tesis de Especialidad]. [Quito]: Universidad Central del Ecuador; 2019 [citado 14 de octubre de 2021]. Disponible en: Disponible en: http://www.dspace.uce.edu.ec/handle/25000/20108 [ Links ]
8. Ripollés-Melchor J, Ramírez-Rodríguez JM, Casans-Francés R, Aldecoa C, Abad-Motos A, Logroño-Egea M, et al. Association Between Use of Enhanced Recovery After Surgery Protocol and Postoperative Complications in Colorectal Surgery: The Postoperative Outcomes Within Enhanced Recovery After Surgery Protocol (POWER) Study. JAMA Surg. 2019;154(8):725-36. [ Links ]
9. Gallego LA, Rodallega AO, Barbosa R, Abueta AYM, Martínez Jaramillo CE, Senejoa Nuñez NJ, et al. Cirugía para enfermedad colo-rectal vía laparoscópica por el servicio de coloproctología del Hospital Militar Central (2005 - 2015). Rev Colomb Gastroenterol. 2018;33(1):8-15. [ Links ]
10. Ban KA, Berian JR, Ko CY. Does Implementation of Enhanced Recovery after Surgery (ERAS) Protocols in Colorectal Surgery Improve Patient Outcomes? Clin Colon Rectal Surg. 2019;32(2):109-13. [ Links ]
11. Maurette RJ, García Ejarque MD, Ruíz H, Bregante ML, Bogetti DJ, Cillo M, et al. Abordaje laparoscópico simultáneo del cáncer de colon con metástasis hepáticas. Rev Argent Cir. 2019;111(4):245-67. [ Links ]
12. Domínguez Herrera J, Sirtori Campo G. Caracterización de pacientes y resultados de la cirugía laparoscópica en cáncer colorrectal. Organización clínica general del norte periodo julio de 2014 a marzo de 2017 [Internet] [Tesis de Especialidad]. [Barranquilla]: Universidad Libre Seccional Barranquilla; 2017 [citado 14 de octubre de 2021]. Disponible en: Disponible en: http://repository.unilibre.edu.co/handle/10901/10726 [ Links ]
13. Avellaneda N. Resultados en el tratamiento quirúrgico del cáncer de colon por vía laparoscópica. Análisis retrospectivo. Rev Argent Coloproctol [Internet]. 2021 [citado 14 de octubre de 2021];32(2). Disponible en: Disponible en: https://revistasacp.com/index.php/revista/article/view/80 [ Links ]
14 . Vaccarezza H, Vaccarezza DR. Resecciones colorrectales laparoscópicas en una comunidad rural. Rev Argent Cir. 2018;110(4):195-201. [ Links ]
15. Pedrazzani C, Conti C, Mantovani G, Fernandes E, Turri G, Lazzarini E, et al. Laparoscopic colorectal surgery and Enhanced Recovery After Surgery (ERAS) program. Medicine (Baltimore). 2018;97(35):e12137. [ Links ]
16. Guevara Jabiles A, Cedeño Ascoy EE, Berrospi Espinoza FM, Aguilar Onofre E, Chávez Passiuri I, Luque-Vásquez C, et al. Recuperación mejorada después de cirugía en cáncer colorrectal. Instituto Nacional de Enfermedades Neoplásicas. Acta Médica Peru. 2021;38(2):89-96. [ Links ]
17. Castro Barrera GP, Ramírez Molestina JN. Complicaciones tempranas y tardías en pacientes de 30 a 80 años que se realizaron resección colónica en el Hospital General “Guasmo Sur” del 1 de enero del 2018 hasta el 31 de diciembre del 2019. [Internet] [Tesis de Grado]. [Guayaquil]: Universidad Católica de Santiago de Guayaquil; 2021 [citado 14 de octubre de 2021]. Disponible en: Disponible en: http://repositorio.ucsg.edu.ec/handle/3317/16765 [ Links ]
18. González-Valverde FM, Vicente-Ruiz M, Gómez-Ramos MJ. Factores asociados a dehiscencia en cáncer de colon. Cir Cir. 2019;87(3):347-52. [ Links ]
19. Rodríguez Infante A. Cirugía abierta versus laparoscópica en pacientes con cáncer de recto en el área central de Asturias: morbilidad, calidad de vida y supervivencia [Internet] [Tesis Doctoral]. [Oviedo]: Universidad de Oviedo; 2019 [citado 14 de octubre de 2021]. Disponible en: Disponible en: https://digibuo.uniovi.es/dspace/handle/10651/54056 [ Links ]
20. Rodríguez Infante A, Fernández Martínez D, Monasterio Díaz MP. Resultados a corto plazo, recurrencia local, supervivencia global y calidad de vida en pacientes intervenidos de cáncer de recto: Revisión sistemática comparativa entre abordaje abierto y laparoscópico. Arch Coloproctol. 2019; 2(1): 22-22. [ Links ]
AUTHORS’ CONTRIBUTIONS: Dr. Cesar Matoza, Dr. Pablo Schaerer, and Dr. Ariel Benegas had the study idea, conducted it, were involved in the bibliographic references, and conducted its final review. Dr. Adriana Echeverría conceived the reference research, and reviewed all anatomopathological reports.
Received: January 06, 2023; Accepted: March 03, 2023











 texto em
texto em