Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Cirugía paraguaya
versão On-line ISSN 2307-0420
Cir. parag. vol.47 no.1 Asunción abr. 2023
https://doi.org/10.18004/sopaci.2023.abril.12
Original article
Prevalence of appendiceal tumors in post-operated appendectomy patients in the emergency room of the IPS Central Hospital from January through December 2020
1Hospital Central del Instituto de Previsión Social. Asunción, Paraguay.
Introduction:
Appendiceal tumors have a variable appearance. Onset is often appendiceal inflammatory clinical signs. They can be diagnosed through histological studies of the surgical piece. Appendiceal specimens obtained at Hospital Central del Instituto de Previsión Social were studied by the anatomical pathology lab on a routine basis.
Objectives:
To know the exact prevalence of appendiceal tumors in emergency appendectomies performed in such hospital from January 2020 through December of that same year.
Results:
A total of 7 cases (0.81%) of appendiceal tumors were obtained from 860 appendectomies (6 cases of adenoma, and 1 case of moderately differentiated grade 2 infiltrating adenocarcinoma of the cecal appendix). This is the case of a 76-year-old woman.
Conclusions:
The most common anatomopathological diagnosis of tumor etiology in this population was adenoma followed by adenocarcinoma. These were diagnosed during the 6th and 7th decades of life. The study included a total of 860 patients with a mean age of 31.81 years being appendiceal signs more common during the 2nd and 3rd decades of life.
Keywords: Appendiceal tumors; Acute appendicitis; Appendectomy.
Introducción:
Los tumores apendiculares tienen una presentación variable, en muchas ocasiones, como un cuadro inflamatorio apendicular. Estos tumores se diagnostican con el informe histológico de la pieza operatoria. Las muestras de las apendicetomías realizadas en el Hospital Central del Instituto de Previsión Social fueron estudiadas por el Servicio de Anatomía Patológica de forma rutinaria.
Objetivos:
Conocer la prevalencia de tumores apendiculares en apendicectomías de urgencia realizadas en el citado Hospital entre enero y diciembre del 2020.
Resultados:
Se obtuvieron un total de 7 casos (0,81%) de tumores apendiculares de 860 apenedicectomías, 6 casos de adenoma y un caso de adenocarcinoma infiltrante moderadamente diferenciado grado 2 de apéndice cecal. Este es el caso de una paciente de 76 años.
Conclusión:
El diagnostico anatomopatológico de naturaleza tumoral más frecuente en esta población es el adenoma seguido del adenocarcinoma. Se observaron en el sexto y séptimo decenios de la vida. El estudio incluyó a un total de 860 pacientes con una media de edad de 31,81 años siendo los cuadros apendiculares más frecuentes durante el segundo y tercer decenios de la vida.
Palabras clave: Tumores apendiculares; apendicitis aguda; apendicetomía
INTRODUCTION
Appendix is a normal true diverticulum of the caecum. Same as any other diverticulum, it shows a tendency to become swollen in an acute and chronic way. Acute appendicitis is a relatively common entity. Lesions including tumors can also damage the appendix. However, they are far less common1.
Vermiform appendix is tubular and flexuous and it is located in the medial and lower regions of the caecum, some 2 cm or 3 cm below the ileal orifice. It measures 9 cm in length and ends in a round-shaped extremity2). Appendiceal mucosa is of colonic type with a cylindrical epithelium. Mucin-producing neuroendocrine and goblet cells can be found around its tubular structure. Lymphatic tissue can be found in the appendiceal submucosa, which makes some hypothesize that the organ is involved in the immune function of the body3.
Acute appendicitis is the most common disease of the appendix, and the main cause for surgical abdomen4,5. Appendiceal inflammation is an important problem of public health with a lifetime incidence rate of 8.6% in men and 6.7% in women. The highest incidence rate has been described during the 2nd and 3rd decades of life. Although the rate of appendectomies in developed countries has dropped over the past few decades, it is one of the emerging abdominal surgeries to this date6.
Proximal appendiceal lumen obstruction elevates pressure in its distal portion through mucus secretion and air production by the bacteria it contains. The progressive distension of the appendix alters venous drainage, which eventually causes mucosal ischemia. With obstruction comes ischemia across the entire thickness of the appendix, which eventually causes perforation3.
The etiology of appendicitis is maybe lumen obstruction that can be due to lymphoid hyperplasia in pediatric populations. In adults, it can be due to fecalites, fibrosis, foreign bodies (food, parasites, stones) or neoplasms3,6.
Timely diagnosis is the best way to implement early treatment with fewer complications, which is significantly challenging because of the different signs of clinical presentation7. The proper treatment for uncomplicated acute appendicitis is emergency appendectomy3.
Appendix disease represents over 50% of the activity displayed in general surgery. Also, it includes rare cases like primitive tumors in that organ: 90% are carcinoid, 8% mucoceles, and only 2% adenocarcinomas8). Appendiceal tumors correspond to 0.4% of all GI neoplasms reported9). A total of 1% of all appendicectomies performed are due to appendiceal tumors4,6,9-11. Malignant tumors are confirmed through pathological analysis (0.9% to 1.4% of all appendicectomies performed)4,12) with similar numbers given by different authors3.
Most primary appendiceal cancers occur when patients are between 55 and 65 years old except for carcinoid tumor, which is more prevalent during the 3rd decade of life. Risk seems to be the same for both men and women9. Incidence rate, though, is higher in women compared to men (4:1 ratio) and they often occur after 55.
In a large series of appendiceal tumors from the Surveillance, Epidemiology, and End Results (SEER) database from the U.S. National Cancer Institute with data from 1973 through 2007, it was confirmed that the most common histological type is mucinous adenocarcinoma followed by type 1 intestinal adenocarcinoma. Neuroendocrine neoplasms represent, only, 11% of all primary appendiceal tumors reported10.
The WHO categorizes cecal appendiceal tumors into 2 different groups: epithelial and non-epithelial. The former group includes adenomas, carcinomas, carcinoid tumors (well-differentiated neuroendocrine tumors), tubular, mucinous, and mixed carcinoids (carcinoid-adenocarcinomas) while the latter group includes including neuromas, lipomas, leiomyomas, GI stromal tumors, leiomyosarcomas, and Kaposi sarcomas, among other9,14,15.
Although rare, appendiceal tumors need proper treatment. In any procedures, whether scheduled or emergency, unexpected neoplasms can be found at any time. It is estimated that the onset of 50% of appendiceal neoplasms is appendicitis, and are diagnosed in the anatomopathological study of the surgical piece. Nonetheless, variable presentations have been reported3). The routine anatomopathological study of cecal appendix can show unsuspected anomalies in around 5% of the cases being appendiceal tumors an important part of these findings14.
Overall, if a mass is incidentally found during surgery, appendicectomy is performed followed by tumor study since most tumors are mucoceles or small carcinoids. However, in the presence of lymphomas or large tumor masses, chemotherapy and extensive surgery would be required. In the presence of an adenocarcinoma, the algorithm of treatment is not as accurate and, therefore, more controversial9). Appendiceal adenocarcinoma is rare (incidence rate from 0,08 to 0,1%) if we look at the data of all appendicectomies performed. Treatment is the same as the one used with cecal adenocarcinoma consisting of right hemicolectomy with regional lymphadenectomy3.
This study was conducted to expose the prevalence of appendiceal tumors in patients treated with emergency appendicectomy at our center, and the different types of neoplasms found in the anatomopathological study conducted.
MATERIAL AND METHOD
This was an observational, descriptive, cross-sectional, and retrospective study of patients treated with emergency appendectomy due to inflammatory acute abdomen of probable appendiceal origin at Hospital Central del Instituto Previsión Social from January through December 2020.
Surgical files and biopsy reports of the study patients were used for data mining purposes. Surgical files of patients with postoperative diagnoses of acute abdomen of a different etiology (eg, inflammatory pelvic disease, complicated ovarian cyst, primary peritonitis, mesenteric adenitis, ileitis, etc.) appendectomies performed in the context of scheduled surgeries for a different condition, appendiceal phlegmon where cecal appendix could not be identified and, therefore, without anatomopathological study, and specimens with poor fixation and, also, no studies were all excluded from this study.
The information obtained was analyzed confidentially in full observance of all bioethical principles. Codes for the files of each patient were used. No informed consent was deemed necessary since data were obtained from health records. No maleficent or discrimination risk existed or any commercial conflicts of interest.
After obtaining the approval of the research protocol, and having been granted access to the Hospital Computed System (HCS) database, data were stored in an Excel® spreadsheet from January through December 2020 in compliance with the inclusion and exclusion criteria described above. Descriptive statistics was used with distribution-based summarized measurements, tables of frequency, and sector and bar charts. Data were collected, described, and tabulated on a Microsoft Office® Excel® spreadsheet.
Table 1 Comparison among preoperative diagnosis, intraoperative finding, and anatomopathological diagnosis
| Preoperative diagnosis | Intraoperative finding | Anatomopathological diagnosis |
|---|---|---|
| Acute appendicitis | Hard cecal appendix | Adenocarcinoma of cecal appendix |
| Acute appendicitis | Gangrenous cecal appendix | Serrated adenoma |
| Acute appendicitis | Gangrenous cecal appendix | Serrated adenoma |
| Acute appendicitis | Gangrenous cecal appendix | Serrated adenoma |
| Acute appendicitis | Gangrenous cecal appendix | Serrated adenoma |
| Acute appendicitis | Phlegmonous cecal appendix | Serrated adenoma |
| Acute appendicitis | Congestive cecal appendix | Serrated adenoma |
RESULTS
A total of 860 patients treated with emergency appendectomy due to inflammatory acute abdomen of probable appendiceal etiology at Hospital Central Instituto Previsión Social from January through December 2020 were included in the study. The mean age of the study patients was 31.81 years, 58.84% of whom were men (Chart 1).
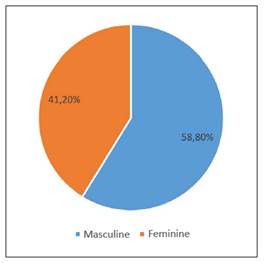
Chart 1. Study population based on sex. Patients treated with emergency appendectomy due to inflammatory acute abdomen of probable appendiceal etiology at Hospital Central del Instituto de Previsión Social from January through December 2020.
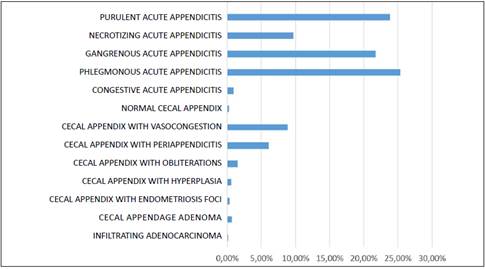
These were among the most common non-neoplastic findings made: phlegmonous, gangrenous, and purulent acute appendicitis, among other (Chart 2).
The anatomopathological report of 6 cases confirmed the presence of adenoma in cecal appendix coexisting with acute appendicitis in 0.70% of the cases. The mean age was 60 years with male predominance (66.67%)
One single case was found (0.12%) with a biopsy report of moderately infiltrating grade 2 adenocarcinoma of cecal appendix: the neoplasm shows irregular margins infiltrating into the subserosa. In addition to the surgical margin compromised, there is presence of acute and chronic infiltration with microabscess formation (acute appendicitis). This is the case of a 76-year-old woman treated with a second surgical act to perform a right colectomy.
DISCUSSION
In the analysis of 860 patients with a postoperative diagnosis of acute appendicitis, a total of 7 appendiceal tumors were confirmed in the anatomopathological study of these patients’ surgical pieces. Acute appendicitis was present in all cases same as it happened in the study conducted by Baltazar-Alba et al.9 These findings corresponded to 0.82% of the cases studied, which are consistent with the data obtained by F. Charles Brunicardi et al., and Courtney M. Townsend et al.3,6
The most common histological type in this population was appendiceal adenoma followed by adenocarcinoma of the cecal appendix, which varies compared to other studies in which the most common malignant tumor was carcinoid or neuroendocrine tumors3,6,9. The most common benign tumor was appendiceal neuroma14, and mucinous neoplasms15. Benign tumors were predominant in men in a 4 to 2 ratio, which is different from the findings made by Álvarez-Álvarez S et al.14 regarding neoplastic tumors (0.12% of the cases). It occurred in a woman, a similar result was obtained by Álvarez-Álvarez S et al.14 These occurred predominantly during the 6th and 7th decades of life. Mean age was 60.5 years. This is a different result compared to the study conducted by Baltazar-Alba et al.9 (Mean age, 40.6 years).
CONCLUSIONS
The most common anatomopathological diagnosis of tumor etiology in this population was adenoma followed by adenocarcinoma. They were seen more predominantly during the 6th and 7th decades of life. The study included a total of 860 patients with a mean age of 31.81 years. Appendix disease was more common during the 2nd and 3rd decades of life (predominantly in male patients). Surgical findings made in the hard cecal appendix were categorized as gangrenous, phlegmonous, congestive and necrotic cecal appendix, and appendiceal phlegmon. After studying the biopsy reports of the specimens obtained from the appendectomies performed, appendiceal inflammatory processes and tumors of benign and malignant etiology were identified. The appendiceal tumors identified were serrated adenoma of the cecal appendix, and adenocarcinoma.
REFERENCES
1. Kumar V, Abbas AK, Aster JC. Robbins Patología Humana. Décima. Elsevier; 2018. p. 643-636. [ Links ]
2. Latarjet M, Ruiz Liard A. Anatomia Humana. Quinta. Vol. 2. Médica Panamericana; 2019. p. 1584 -1587. [ Links ]
3. Courtney M, Townsend R, Beauchamp D, Evers BM, Mattox KL. Sabiston Tratado de Cirugia. Fundamentos Biologicos de la Práctica Quirúrgica Moderna. 20.a ed. Elsevier; 2018. 1307-1310. [ Links ]
4. Pantoja Pachajoa DA, Bruno MA, Parodi M, Viscido G, Mandojana F. Patología apendicular: de lo frecuente a lo infrecuente. Methodo Investigación Aplicada a las Ciencias Biológicas [Internet]. 2017;2(4):126-128 Disponible en: https://methodo.ucc.edu.ar/index.php/methodo/article/view/55 [ Links ]
5. Vinueza Aguay G, Gallegos Ponce C, Morales Solís J, Vinueza López G. Diagnóstico histopatológico de la apendicitis aguda en el Hospital Regional Docente Ambato 2015. Investigación y Desarrollo 2016; 2022; 10(1): 12-18. [ Links ]
6. Brunicardi FK, Andersen DK, Billiar TR, Dunn DL, Hunter JG, Kao LS, et al. Schwartz’s Principles of Surgery. 11.a ed. Vol. 2. Mc Graw Hill; 2019. [ Links ]
7. Ávila MJ. Apendicitis aguda: revisión de la presentación histopatológica en Boyacá, Colombia. Revista Colombiana de Cirugía [Internet]. 2015;3(29): 125-130. Disponible en: https://www.revistacirugia.org/index.php/cirugia/article/view/338 [ Links ]
8. Arias-Moreno R, Treviño-Taboada EP, García-Bravo LM. Tumores apendiculares, cistoadenoma mucinoso. Sal Jal 2021;8(2):119-23. [ Links ]
9. Baltazar-Alba I, Iñiguez-Martínez C, Vázquez-Isidro E, Campo FM-M del, Ulloa-Robles JJ, Amezcua-Gálvez JE, et al. Prevalencia de neoplasias apendiculares: Revisión clínico-patológica de apendicectomías durante 6 años. Rev Med MD. 2019;9.10(2):119-24. [ Links ]
10. Fulle C A, Castillo R R, Moreno L P, Orellana G M, Cabreras S M, Briones N P, et al. Análisis de casos de adenocarcinoma apendicular y su manejo en una serie de 10 años en el Hospital Doctor Sótero del Río. Revista chilena de cirugía. ago 2017;69(4):297-301. [ Links ]
11. Piñón-García K, Almeida-Esquivel Y, Correa-Borrell M. Adenocarcinoma mucinoso diagnosticado postapendicectomía bajo anestesia general orotraqueal. Revista Electrónica Dr Zoilo E Marinello Vidaurreta. may de 2021;46(3):2234. [ Links ]
12. Villegas-Tovar E, González-Chávez MA, Lemus-Ramírez RI, López-Ramírez AY, Faes-Petersen R, Gidi AD-G, et al. Tumores apendiculares como causa de apendicitis aguda. Experiencia de 10 años en un hospital privado. Med Sur. 2016;22(2):76-81. [ Links ]
13. Ángeles PD, Vega X, Palacios J. Tumor mucoso apendicular. Revista Colombiana de Cirugía . mar 2016;31(1):57-60 [ Links ]
14. Álvarez-Álvarez S, González-Pérez LG, Sánchez-Pérez EA, Madrigal-Téllez MA, Hurtado-López LM. Prevalencia de tumores apendiculares en pacientes operados de apendicectomía en el Hospital General de México Dr. Eduardo Liceaga, revisión a 10 años. Cirujano General. 2016;38(1):7-11. [ Links ]
15. Trujillo-Díaz JJ, Ruiz-Soriano M, Ortiz de Solórzano-Aurusa J, Andrés-Asenjo BD, Corrales-Cruz D, Beltrán-de Heredia Rentería JP. Neoplasias benignas no carcinoides del apéndice cecal: presentación de 36 casos durante los últimos 17 años en un hospital de tercer nivel. Cirugía y cirujanos. dic 2019;87(6):630-5. [ Links ]
16. Morales AJP, Jiménez DC, Anderson IA, Marrero DF, Machado LP, Loandy SM. Tumor neuroendocrino, mucocele y adenoma tubulo-velloso: tres lesiones infrecuentes en el apéndice cecal: Neuroendocrine tumours, mucocele, and tubulovillous adenoma: three uncommon lesions in the cecal appendix. ARS MEDICA Revista de Ciencias Médicas. agosto 2021;46(3):32-9. [ Links ]
Authors’ contributions: All the authors share responsibility for the study idea, drafting of the manuscript, bibliographic search, and final review.
Received: November 26, 2022; Accepted: February 03, 2023











 texto em
texto em