Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Cirugía paraguaya
On-line version ISSN 2307-0420
Cir. parag. vol.46 no.3 Asunción Dec. 2022
https://doi.org/10.18004/sopaci.2022.diciembre.37
Case report
Percutaneous treatment of psoas muscle abscess secondary to spondylodiscitis
1Hospital Regional Salto, Uruguay.
El objetivo del siguiente trabajo es describir el tratamiento percutáneo de un absceso localizado en el músculo psoas, entidad poco frecuente y presentación clínica inespecífica lo que constituye un desafío diagnóstico. Su detección ha mejorado con la utilización de técnicas de imagen. La fiebre, dolor abdominal y del miembro inferior ipsilateral son las manifestaciones habituales. La antibioticoterapia junto al drenaje (percutáneo o quirúrgico) debe considerarse el tratamiento de elección.
Palabras claves: Absceso de psoas ilíaco; espondilodiscitis; drenaje percutáneo
The objective of the following study is to describe the percutaneous treatment of psoas muscle abscess, a rare entity with nonspecific clinical presentation, which stands as a diagnostic challenge. Its detection has improved with the use of imaging modalities. Fever, abdominal pain, and ipsilateral lower limb pain are the most common clinical signs. Antibiotic therapy together with drainage (percutaneous or surgical) should be considered the treatment of choice.
Keywords: Iliopsoas abscess; Spondylodiscitis; Percutaneous drainage
INTRODUCTION
Psoas muscle abscess is a rare entity. A rate of 0.4% for every 100 000 inhabitants has been reported being more common in men compared to women¹. On the clinical level, it presents as fever, back pain, and walking disorders². This is the case of a 64-year-old patient with a psoas muscle abscess due to spondylodiscitis successfully treated with antibiotic therapy and percutaneous drainage.
CASE REPORT
This is the case of a 64-year-old man with diabetes mellitus type II and arterial hypertension. The patient showed a 12-day history of asthenia, adynamia, walking difficulties, abdominal and back pain of growing intensity, fever, and chills. The abdominal examination reveals pain to the right side without peritoneal irritation, pain to palpation over the right iliac fossa, and active and passive mobilization of the ipsilateral lower limb.
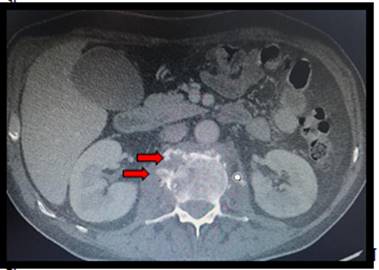
Hemogram results show leukocytosis of 19 400/mm3 with 90.3% neutrophils, hemoglobin, 11.1 g/dL, normal platelet counts, C-reactive protein levels of 173.38 mg/dL, and erythrocyte sedimentation rates of 132 mm/h. Abdominal ultrasound reveals the presence, at right paravertebral level, of a 14 cm x 4 cm long, well-demarcated, non-vascularized, hypoechoic image suggestive of fluid collection at such level. Given the ultrasound findings, an abdominal, pelvic, and thoracic computed tomography scan with IV contrast is performed. It reveals the presence of disc space narrowing in L2 and L3 vertebrae, and irregularities of vertebral discs, which are all findings consistent with spondylodiscitis (see Figure 1), which is, in turn, associated with extensive fluid/abscess collection of the right psoas muscle measuring 155 mm x 45 mm x 45 mm (see Figure 2).
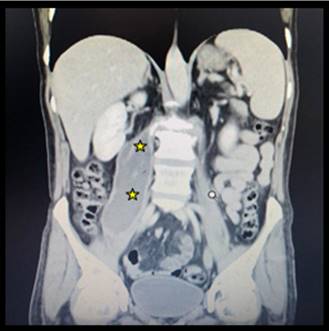
Figure 2. Abdominal and pelvic coronal computed tomography scan. Right iliac psoas muscle abscess (yellow arrows).
Empirical antibiotic therapy with IV pieracillin/tazobactam 4gr/0.5gr every 6 hours is started. Tomography-guided percutaneous drainage is performed, and a 12-Fr drainage tube is uneventfully inserted with the trocar technique without complications. A total of 100 cc of purulent fluid are obtained. The sample was then sent to perform an antibiogram, cytological examination, and adenosine deaminase diagnostic testing (ADA) (Figure 3).
The sample ends up growing Staphylococcus aureus. After discussion with the infectious disease unit, the patient is administered antibiotics: 2 gr of IV cefazoline every 8 hours plus 300 mg of oral rifampicin every 12 hours. The patient’s disease progression is good with clinical improvement, and normal infectious parameters.
Drainage is removed after 12 days. IV antibiotic therapy is maintained for a month and extended for another 2 months orally to end up completing 3 months of antibiotic therapy. The trauma doctor indicates immobilization, and orthopedic stabilization with plaster corset followed by physical therapy with good progression.
Currently, after the completion of antibiotic treatment, the patient remains in outpatient control in the trauma center, infectious disease unit, and surgery unit. He remains asymptomatic and has had zero relapses.
DISCUSSION
Psoas muscle abscess was a known complication of tuberculous spinal column. Currently, it is the most common cause of pyogenic infection and can be primary (hematogenous dissemination) or secondary being the most common cause of spondylodiscitis³.
The classic triad of clinical presentation of fever, back pain, and limp is seen only in 30% of the cases, which complicates its diagnosis even further². At bacteriological level, the most common microorganism is Staphylococcus Aureus that represents up to 65% of the cases followed by Escherichia coli the latter being associated with urinary tract or GI infections, old age, immunosuppression, and diabetes⁴. Lab test results that support diagnosis include leukocytosis, elevated erythrocyte sedimentation rate and C-reactive protein as it was the case of our patient.⁴
Regarding imaging diagnosis, the ultrasound can be useful to assess intramuscular collections. However, utility is limited in deep retroperitoneal structures due to the patient’s anatomy (obesity for example), and gas interposition, and presents a 60% sensitivity only. Computed tomography scan and nuclear magnetic resonance imaging offer better diagnostic accuracy with similar sensitivity rates between 80% and 87%. Between both imaging modalities, computed tomography scan is especially useful given its good sensitivity, greater availability, and lower cost⁵.
Regarding the therapeutic arsenal, there are 2 basic pillars here: targeted antibiotic therapy based on microbiological profiles and surgical or percutaneous drainage. Currently, the technique of choice is the latter due to the good results and lower rates of complications.⁶,⁷
Surgical drainage (used alone or in combination with percutaneous techniques) is spared for multiloculated abscesses with extensive compromise of structures, and abscesses due to some specific conditions, among them, inflammatory bowel disease, pyelonephritis, epidural abscesses with spinal compression, among other⁸,⁹. Imaging-guided percutaneous approach is a safe and less invasive alternative, which should be considered as the first-line therapy because it yields results similar to surgical drainage with less morbidity, and a shorter length of stay¹⁰.
The authors declared no conflicts of interest whatsoever, and they equally contributed to the production of this study.
REFERENCES
1. Bartolo DC, Ebbs SR, Cooper MJ. Psoas abscess in Bristol: a 10-year review. Int J Color Dis. 1987; 2(2): 72-6. [ Links ]
2. Kaya S, Kaya S, Kava S, Comoglu S. A disease that is difficult to diagnose and treat: evaluation of 343 spondylodiscitis cases. J Int Med Res. 2021 nov; 49(11): 3000605211060197. doi: 10.1177/03000605211060197. PMID: 34851766; PMCID: PMC8647245. [ Links ]
3. Ibrahim FM, EL-rady F, Abd El-Rady MA. Transverse process osteotomy for surgical drainage of primary iliopsoas abscess and secondary cases combined with spondylodiscitis. International Orthopaedics, 2020. -. doi:10.1007/s00264-020-04732-5 [ Links ]
4. Fernández Ruiz M, Estébanez Muñoz M, López Medrano F, Aguado JM. Absceso del músculo iliopsoas: Tratamiento y evolución en una serie de 35 pacientes. Enferm Infecc Microbiol Clin 2012; 30(6): 307-311. [ Links ]
5. Silva AM, Schmalbach LA. Absceso del psoas y osteomielitis de la columna lumbar. Caso clínico. Arch Argent Pediatr. 2016; 114 (5): e333-7. [ Links ]
6. Tan YX, Cheong WL, Fong TS. Gas-Forming Psoas Abscess Secondary to Lumbar Spondylodiscitis. Cureus. 2021 Apr 9;13(4): e14388. doi: 10.7759/cureus.14388. PMID: 33981508; PMCID: PMC8106948. [ Links ]
7. Takada T, Terada K, Kajiwara H, Ohira Y. Limitations of using imaging diagnosis for psoas abscess in its early stage. Intern Med 2015; 54(20): 2589-2593. [ Links ]
8. Miller ELC, Miller LFF, Carvalho JG, et al. Psoas muscle abscess simulating acute appendicitis: A case report. Int J Surg Case Rep. 2016; 25: 139-42 [ Links ]
9. Hsieh MS, et al. Features and treatment modality of iliopsoas abscess and its outcome: A 6-year hospital-based study. BMC Infect Dis 2013; 13: 578 [ Links ]
10 . Lock Vargas Y, Joo Fernández H, Díaz Villanueva P, Campana Román P, Valencia Avalo D. Absceso de psoas. Revista Científica Ciencia Médica, 2018; 21(1): 113-117. [ Links ]
Received: September 01, 2022; Accepted: November 12, 2022











 text in
text in