Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Cirugía paraguaya
versão On-line ISSN 2307-0420
Cir. parag. vol.46 no.3 Asunción dez. 2022
https://doi.org/10.18004/sopaci.2022.diciembre.34
Case report
Stomach volvulus. About a case
1 Hospital Escuela del Litoral. Paysandú, Uruguay.
El vólvulo gástrico es una entidad rara y urgente. Definido como la rotación gástrica sobre su eje más de 180 grados, determina una estenosis al pasaje del contenido gástrico, distensión y derivando en el compromiso de la irrigación parietal. El atraso en su diagnóstico y/o tratamiento deriva en estrangulación o perforación gástrica. Presentamos un paciente de 90 años con un vólvulo gástrico, su abordaje diagnóstico y terapéutico con gastropexia laparoscópica con buenos resultados.
Palabras Claves: Vólvulo gástrico; obstrucción de la salida gástrica; gastropexia laparoscópica
Gastric volvulus is a rare entity and an emergency condition. It is defined as gastric rotation on its axis > 180 degrees, it conditions stenosis to the passage of gastric content, and distension that eventually leads to compromise of parietal irrigation. A delayed diagnosis and/or treatment leads to strangulation or gastric perforation. This is the case of a 90-year-old patient with gastric volvulus, her diagnostic and therapeutic approach with laparoscopic gastropexy with good clinical outcomes.
Keywords: Stomach volvus; Gastric outlet obstruction; Laparoscopic gastropexy.
INTRODUCTION
Stomach volvulus is defined as an abnormal rotation of the stomach on its axis that leads to luminal obstruction whether transient due to spontaneous devolvulation or it can compromise the parietal vasculature leading to stomach ischemia. In the latter case, morbidity and mortality rates reach 80% triggering emergency surgeries1. Its highest incidence rate has been reported during the 5th decade of life though other authors describe higher incidence rates in children. There is no prevalence based on race or sex.
This case shows our own experience at our center on a case report of gastric volvulus with laparoscopic surgical resolution with good clinical outcomes.
CASE REPORT
This is the case of a 90-year-old woman without follow-up examinations or a significant past surgical history who presented to the ER with clinical signs of cyclic vomiting syndrome of the entire stomach content of 72-hour evolution. Vomiting appeared greenish in color. These signs were accompanied by a 24-hour material transit retention in the patient’s stomach.
The patient’s physical examination revealed a substandard physical condition, dehydration, painful expressions at palpation, and no fever. Hemodynamics was normal with presence of soft, depressible, and distended abdomen that was painful to diffuse superficial palpation. No elements of peritoneal irritation were seen. A nasogastric tube was inserted with presence of abundant green color content. Approximately 1000 cc were drained. The x-ray image of the dorsal abdomen acquired in the decubitus and standing positions reveals the presence of a major gastric distension with rotation of the stomach on its axis (Figure 1).

Figure 1. Abdominal x-ray in the dorsal decubitus position showing an image consistent with gastric volvulus, large gastric distention, and nasogastric tube inside. Displaced transverse colon underneath.
The abdominal and pelvic computed tomography scan with IV contrast performed revealed the presence of gastric malrotation with pyloric antrum elevation of gastric volvulus appearance confirming the obstruction (Figure 2). Also, the stomach appears with significant retention of content and mural cystic neurofibromatosis. No pneumoperitoneum is confirmed, but presence of adjacent fluid. Presence of elevated left hemidiaphragm with a small amount of left pleural effusion.
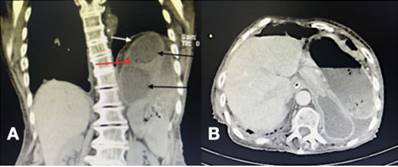
Figure 2. Computed tomography scan. Panel A: coronal view showing gastric malrotation with antrumpylorus elevation causing the obstruction and looking like gastric volvulus. Also, presence of mild left pleural effusion. Black arrows: stomach with significant fluid content; red arrow: mural cystic neurofibromatosis; white arrow: left hemidiaphragm elevation. Panel B: axial view. Small amount of fluid adjacent to the stomach. No pneumoperitoneum.
The patient’s progression was good and abdominal pain receded after placing the nasogastric tube with scarce vomiting. The esophagogastroduodenal x-ray acquired with oral hydrosoluble contrast revealed the presence of stopped material at gastric body level without passage of contrast towards the duodenum (Figure 3).

Figure 3. Esophagogastroduodenal x-ray with oral hydrosoluble contrast reveals the presence of stopped content at gastric body level without passage of contrast towards the duodenum.
Therefore, an exploratory emergency laparoscopy was performed that confirmed spontaneous devolvulation and gastric body distention without elements of parietal ischemia or associated hiatal defect. Gastropexy of the greater curvature was performed towards parietal peritoneum with 2 polypropylene meshes without complications (Figure 4).

Figure 4. Laparoscopic gastropexy. Presence of two polypropylene meshes fixated from the gastric greater curvature towards the parietal peritoneum.
Good postoperative progression. The nasogastric tube was removed after 24 hours. Afterwards, the patient was fed orally without abdominal pain, fever, preserved transits, and with a nice-looking surgical wound. This led to the patient’s discharge from the hospital. The outpatient control of the patient 1 week later confirmed that she remained totally asymptomatic.
DISCUSSION
Stomach volvulus is a rare entity and an emergency condition. Delayed diagnosis and/or treatment can be associated with complication like gastric strangulation or perforation. It can be due to multiple causes determining obstruction to the passage of gastric content—distension —leading to parietal irrigation.
Idiopathic and secondary predisposing factors have been reported. The former are elongations or lack of ligaments that fixate the stomach to the peritoneum, abnormally distended stomach, hernias or diaphragmatic eventrations, erratic spleen or malrotation with asplenia. The latter are reductive gastric surgeries (Nissen’s technique), ruptured gastric ligaments due to liver transplant, trauma, and gastric neoplasms2.
We should mention that although the patient had no past surgical history, she did have an abnormally distended stomach. No hiatal hernia—frequently associated with such condition—was seen according to the medical literature available.
Borchardt’s triad can guide the diagnosis of acute gastric volvulus. It is made up of clinical elements like pain and epigastric distension, nausea with violent vomiting or impossibility to vomit, and the impossibility of passing the nasogastric tube (mainly in children), present in 70% of the cases3.
According to Singleton, gastric volume is classified by its axis on which the stomach spins: organoaxial rotation, mesentericoaxial, and a combination of the two. In the former the stomach rotates on an axis that connects the gastroesophageal junction to the pylorus, the antrum rotates in opposite direction to the gastric fundus this being the most common of all (59%) and commonly associated with diaphragmatic defects4.
Regarding treatment, the current tendency is to use less invasive techniques (endoscopic, laparoscopic or both), which is highly beneficial in high-surgical anesthetic risk patients. Recommendation here is to correct the position of the stomach to later fixate it in its normal position and repair the diaphragmatic defect associated with it. A less commonly used alternative is gastropexy with gastrocolic ligament section (Tanner’s technique), gastrectomy, gastrojejunal anastomosis, and fundus-antrum anastomosis (Opolzer’s technique) among other5.
Regarding treatment, laparoscopy was decided, which had very good results and achieved a clear benefit solving the actual acute disease and sparing a more aggressive procedure that would have added more morbidity and mortality to the patient.
REFERENCES
1. Martínez García R, Peris Tomas N, Del Pozo CD, Vazquez Tarragón A, Martinez Mas E, Trullenque Juan R, Martinez Abad M. Tratamiento del vólvulo gástrico agudo mediante abordaje laparoscópico. Cir Esp. 2013 Mar; 91(3): 189-93. doi: 10.1016/j.ciresp.2012.03.011. Epub 2012 May 22. [ Links ]
2. Sánches S, Vique L, Ardiles O, Herquiñigo R. Vólvulo gástrico: ¿Por qué recordarlo? Revisión a propósito de un caso. Rev. Chil. Radiol. 2012;18(3):129-135. [ Links ]
3. Cabrera-Tovar MG, Renedo-Ri´os JL, Tejeda-Tapia HD. Vólvulo gástrico. Informe de un caso. Acta Pediátr. Méx. 2009; 30(3): 163-6. [ Links ]
4. Gálvez-Valdovinos R, Marín-Santillán E, Funes-Rodríguez JF, López-Ambriz G. Manga gástrica laparoscópica en vólvulo gástrico secundario a eventración diafragmática en paciente adulto. Cir Cir. 2016 Mar-Apr; 84(2): 140-3. doi: 10.1016/j.circir.2015.06.010. [ Links ]
5. Sánchez-Pérez MA, Luque-de León E, Muñoz-Juárez M, Moreno-Paquentin E, Cordera-González de Cosío F, Maydón-González H. Tratamiento laparoscópico del vólvulo gástrico asociado a hernia hiatal en el paciente de edad avanzada. Rev Gastroenterol Mex. 2010; 75(2): 218-22. [ Links ]
Received: April 25, 2022; Accepted: August 11, 2022











 texto em
texto em 



