Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Cirugía paraguaya
versão On-line ISSN 2307-0420
Cir. parag. vol.46 no.3 Asunción dez. 2022
https://doi.org/10.18004/sopaci.2022.diciembre.31
Case report
Mediastinal ectopic parathyroid adenoma. A case report
1Universidad Autónoma de Nuevo León, Servicio de Cirugía General del Hospital Universitario “Dr. José Eleuterio González”, Monterrey, Nuevo León, México
El hiperparatiroidismo primario es causado por el aumento de la secreción de paratohormona, y se describió por primera vez en 1930. 80% de los casos son causados por un adenoma paratiroideo benigno y hasta el 16% pueden presentarse como ectópico. Femenina de 39 años, con multiples infecciones urinarias, urolitiasis, hipercalcemia y paratohormona aumentado. Gammagrama demostró adenoma paratiroideo ectópico en mediastino superior, mediante cervicotomía transversa, esternotomía media y gamma sonda, se resecó lesión sin eventualidades.
Palabras clave: paratiroidectomía; hiperparatiroidismo; paratiroides ectópica; paratiroides mediastinal
Primary hyperparathyroidism is due to the increased secretion of parathyroid hormone. It was described for the first time back in 1930. A total of 80% are due to benign parathyroid adenomas, and about 16% may present as ectopic. This is the case of a 39-year-old female with multiple urinary tract infections, urolithiasis, hypercalcemia, and increased parathyroid hormone. Gammagraphy revealed the presence of ectopic parathyroid adenoma in the superior mediastinum. Through transverse cervicotomy, median sternotomy, and using a gamma probe, the lesion was resected uneventfully.
Keywords: Parathyroidectomy; Hyperparathyroidism; Ectopic parathyroid; Mediastinal parathyroid.
Introduction
Primary hyperparathyroidism (PHPT) is due to an increased secretion of parathyroid hormone (PTH). It is the most common cause of hypercalcemia, above all, during postmenopause. It was described for the first time back in 19301.
Both its rate and prevalence have increased over the past decades thanks to the greater detection of mild hypercalcemia with the use of more biochemical tests with serum calcium that has increased the number of diagnoses of asymptomatic cases of PHPT. Its significance lies in its progression: up to a fourth of all patients ends up developing symptoms within the next 5 years1,2.
A total of 80% of all PHPTs are benign parathyroid adenomas, 15% to 20% are parathyroid hyperplasias, and less than 1% parathyroid carcinomas1.
Ectopic parathyroid glands (EPG), described in up to 16% of the cases, are due to the anomalous migration of these during development. They can be found in tissues that share their embryologic origin3. Imaging modalities are important for the diagnosis, location, and surgical planning of this entity. Parathyroidectomy (PT) is the ultimate treatment here3,4.
This is the case report of a female patient with PHPT due to ectopic parathyroid adenoma.
Clinical signs
This is the case of a 39-year-old woman with multiple episodes of urinary tract infections, renal colics, and nephrolithiasis. She presents with weakness, chronic fatigue, and hypercalcemia (10.9 mg/dL). PTH is analyzed and since elevated levels are found (138.3 pg/mL) PHPT is finally diagnosed.
Management of the patient included a computed tomography scan (see Figure 1) and a gammagraphy with Tc99-sestamibi (Figure 2) that revealed the presence of ectopic parathyroid adenoma of superior mediastinum location. Transverse cervicotomy access was used and medium sternotomy with pneumatic saw was performed under balanced general anesthesia. The radio-and-gamma probe guided minimally invasive parathyroidectomy performed revealed the presence of parathyroid adenoma at mediastinum level (Figure 3) that was resected uneventfully (Figure 4). No events were reported during the postoperative period resulting in lower levels of calcium and PTH.
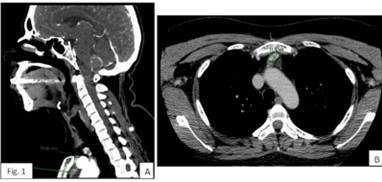
Figure 1. Computed tomography scan. Panel A: Sagittal view showing ectopic parathyroid adenoma 2 cm away from the sternal notch. Panel B: Axial view showing an oval-shaped nodular image with demarcated borders.
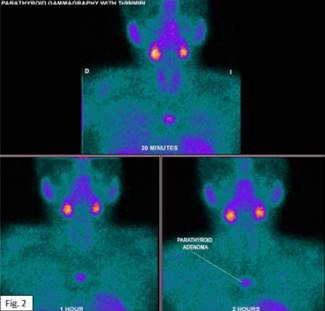
Figure 2. Images acquired through parathyroid gammagraphy with 99mTc-Sestamib showing the ectopic parathyroid adenoma at the superior mediastinum central region.
Discussion
PHPT is more common in women on a 4:1 ratio compared to men. The highest incidence rate has been reported within the first few years after menopause, which is consistent with estrogen loss. Up to 20% of the patients have a past medical history of renal colics1. Our case is consistent with the cases reported in the medical literature available today.
There are 3 different presentations of PHPT: symptomatic or classic (elevated calcium and PTH levels), asymptomatic or normohormonal (elevated calcium and normal PTH levels) and normocalcemic (normal calcium and elevated PTH levels). The latter can be a precursor of traditional PHPT(1, 2). Our patient had classic signs.
The risk factors reported are low calcium intake, low physical activity, large abdominal circumference, obesity, hypertension, neck radiation or nuclear exposure and prolonged lithium therapy1.
Up to 16% of the patients show EPG. Three different studies concluded that the most common regions are the thymus, the retro/paraesophageal space, and thyroid, which represent 56% to 89% combined. Between 6% and 26% have been described in the mediastinum5,6.
Signs and symptoms are due to hypercalcemia, among them, fatigue, weakness, polyuria, polydipsia, constipation, anorexia, vomiting, dehydration, arrhythmias, anxiety, altered mental state, and mood swings. Our patient also complained of fatigue, and chronic weakness1. Frailty-induced fractures, skeletal deformities, and bone pain are also possible. Also, presentation through hypercalciuria, nephrolithiasis, nephrocalcinosis, and reduced renal function1, as it happened in our case and its presentation of classical phenotype.
Diagnosis is achieved after detecting elevated hypercalcemia. Also, elevated PTH levels with ≥ 20 pg/mL in the context of hypercalcemia is consistent with the diagnosis1,7.
Preoperative imaging modalities facilitate surgery by accurately finding the adenoma like ultrasound, gammagraphy with 99m-tecnecium-sestamibi, computed tomography scan, magnetic resonance imaging, and PET8. Gammagraphy has higher sensitivity (89%) and ultrasound has less sensitivity (59% to 76%) although the latter is more widely available. Gammagraphy is considered the gold standard3,8.
Surgery is clearly indicated in patients with symptoms due to hypercalcemia or target organ failure (frailty-induced fractures or colics)1,7. Definitive treatment of choice is parathyroidectomy8. Cervical approach is often enough. However, 2% of the cases of mediastinal location require transsternal or transthoracic approach3.
The rates of healing for an experienced surgeon exceed 95% with a very low rate of complications (< 1% to 3 %) like hemorrhages, hypocalcemia, and recurring laryngeal never injuries1,2. Once parathyroidectomy has been performed, biochemical markers often go back to normal, and bone density goes up, thus reducing the risk of fracture and nephrolithiasis8.
Referencias bibliográficas
1. Silva BC, Cusano NE, Bilezikian JP. Primary hyperparathyroidism. Best Pract Res Clin Endocrinol Metab. 2018 Oct 1;32(5):593-607. [ Links ]
2. Zhu CY, Sturgeon C, Yeh MW. Diagnosis and Management of Primary Hyperparathyroidism. JAMA [Internet]. 2020 Mar 24 [cited 2022 May 17];323(12):1186-7. Available from: https://pubmed.ncbi.nlm.nih.gov/32031566/ [ Links ]
3. Boccalatte LA, Gómez NL, Olivera López S, Abuawad CY. Hiperparatiroidismo ectópico: Detección de la localización mediastinal. Med (B Aires) [Internet]. 2020 May 20 [cited 2022 May 20];80(1):39-47. Available from: http://www.scielo.org.ar/scielo.php?script=sci_arttext&pid=S0025-76802020000100006 [ Links ]
4. Udelsman R, Lin Z, Donovan P. The superiority of minimally invasive parathyroidectomy based on 1650 consecutive patients with primary hyperparathyroidism. Ann Surg [Internet]. 2011 Mar [cited 2022 May 17];253(3):585-91. Available from: https://pubmed.ncbi.nlm.nih.gov/21183844/ [ Links ]
5 5. Vaidya A, Curhan GC, Paik JM, Wang M, Taylor EN. Physical activity and the risk of primary hyperparathyroidism. J Clin Endocrinol Metab [Internet]. 2016 Apr 1 [cited 2022 May 17];101(4):1590-7. Available from: / pmc/articles/PMC4880164/ [ Links ]
6. Roy M, Mazeh H, Chen H, Sippel RS. Incidence and localization of ectopic parathyroid adenomas in previously unexplored patients. World J Surg [Internet]. 2013 Jan 12 [cited 2022 Mar 23];37(1):102-6. Available from: https://link.springer.com/article/10.1007/s00268-012-1773-z [ Links ]
7. Shen W, Düren M, Morita E, Higgins C, Duh QY, Siperstein AE, et al. Reoperation for persistent or recurrent primary hyperparathyroidism. Arch Surg [Internet]. 1996 [cited 2022 May 17];131(8):861-9. Available from: https://pubmed.ncbi.nlm.nih.gov/8712911/ [ Links ]
8. Khan AA, Hanley DA, Rizzoli R, Bollerslev J, Young JEM, Rejnmark L, et al. Primary hyperparathyroidism: review and recommendations on evaluation, diagnosis, and management. A Canadian and international consensus. Osteoporos Int [Internet]. 2017 Jan 1 [cited 2022 May 17]; 28(1):1. Available from: /pmc/articles/PMC5206263/ [ Links ]
Received: June 28, 2022; Accepted: September 19, 2022











 texto em
texto em 





