Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Cirugía paraguaya
versão On-line ISSN 2307-0420
Cir. parag. vol.46 no.2 Asunción ago. 2022
https://doi.org/10.18004/sopaci.2022.agosto.27
Case report
Incidental intraoperative finding of subcapsular liver hematoma post-ERCP. Case report
1Hospital Central del Instituto de Previsión Social. Asunción, Paraguay.
La presencia de un hematoma subcapsular hepático (HSH) posterior a una colangiopancreatografía retrógrada endoscópica (CPRE) es una complicación infrecuente de dicho procedimiento, habiendo sido reportados solo unas decenas de casos hasta la fecha. Presentamos el caso de una paciente de 28 años, en quien se encontró de forma incidental un hematoma hepático de gran tamaño durante una colecistectomía posterior a una CPRE por colédocolitiasis. El hematoma fue tratado de manera conservadora, con posterior drenaje percutáneo en contexto ambulatorio.
Palabras clave: hematoma hepático subcapsular; cpre; colecistectomia
The presence of a subcapsular hepatic hematoma (SHH) after an endoscopic retrograde cholangiopancreatography (ERCP) is an uncommon complication of this procedure; only a few dozens of cases have been reported to this date. This is the case of a 28-year-old woman in whom a very large hepatic hematoma was incidentally found during cholecystectomy after an ERCP due to choledocholithiasis. The hematoma was treated conservatively with subsequent percutaneous drainage in an outpatient context.
Keywords: subcapsular hepatic hematoma; ERCP; cholecystectomy
INTRODUCTION
The complications of an endoscopic retrograde cholangiopancreatography (ERCP) have a prevalence of approximately 10% being the most common of all digestive hemorrhages, pancreatitis, cholangitis or perforation. The presence of a SHH after an ERCP is a rare complication of this procedure, only a few dozen cases having been reported to this date. Treatment depends on the form of presentation, which can occur as a contained hematoma, or as a ruptured hematoma, which should be considered a true surgical emergency. This study presents the case of a finding of a contained SHH following an ERCP treated in a conservatively.
CASE REPORT
This is the case of a 28-year-old woman without a past medical history of interest, who came to the ER with epigastric pain of 12-hour evolution that radiated to her right hypochondrium—of colic type—of moderate intensity that partially subsided with common analgesic drugs. The patient also had nausea and vomits on several occasions plus choluria, without acholia. The blood testing performed at admission revealed: white blood cells (WBC) 7300 IU; neutrophiles (N), 81%; hemoglobin (HB), 11.7 g/dL; total bilirubin (TB) 3.76 mg/dL; direct bilirubin (DB), 2.80 mg/dL, alkaline phosphatase (AP), 518 mg/dL; aspartate transferase alanine (AST), 103 IU; alanine aminotransferase (ALT), 445 IU; and gamma glutamyl-transferase (GGT), 921 IU. The abdominal ultrasound performed revealed the presence of a gallbladder with multiple lithiasis, large caliber choledochus with image suggestive of lithiasis inside of it. The magnetic cholangio-resonance revealed the presence of several non-dilated intrahepatic biliary ducts, common hepatic and choledochus duct of 7 mm in caliber, a 4 mm image of signal void at choledochus orifice level. This examination showed a liver without abnormalities. (See Figure 1)
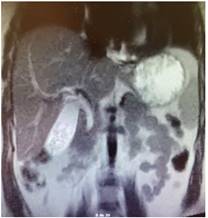
Figure 1. Coronal view of the cholangio-resonance prior to the ERCP. It shows the unharmed liver. Also, it shows a 4 mm image of signal void at choledochus orifice level.
In view of these findings, it was decided to present the case to the Digestive Endoscopy unit with an indication for ERCP. It revealed topical papilla and biliary duct cannalization. Comparatively, it was confirmed that choledochus had a stone of approximately 9 mm inside of it. Guided papillotomy was performed without complications with removal of the choledochal stone with a balloon extractor and control cholangiography with free biliary duct. At the end it bleeding was reported that was controlled by injecting diluted peripapillary adrenalin.
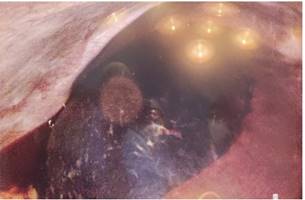
It was decided to schedule a laparoscopic cholecystectomy 24 hours after the procedure where hematic fluid was observed in 150 cc approximately distributed in the right paracolic gutter, subcapsular hepatic hematoma of, approximately, 15 cm in diameter, located in the hepatic surface at segment VII and segment VIII level which appeared to be unharmed, distended gallbladder with thin walls with multiple infra-centimetric stones, thin and long cystic duct. Choledochus appears to have a preserved caliber. (See Figure 2). In view of this finding, it is decided to perform a laparoscopic cholecystectomy that was executed without complications and follow watchful waiting of surgical treatment of hepatic hematoma at that moment. Tubular drainage was left in the right paracolic gutter.
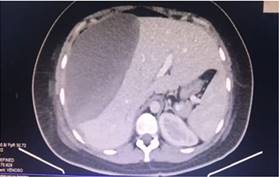
Following surgery, the patient had a torpid evolution, with HB dropping from 11.7 gd/dL down to 8 gd/dl, requiring blood transfusions, in addition to daily fever peaks. Therefore, on day 9 after the surgery, a computed axial tomography scan with double contrast was indicated. It revealed that the liver had increased in size measuring 185 mm in the AP in the right lobe, inhomogeneous parenchyma with extensive hematoma probably subcapsular, dense, and heterogeneous, with fluid level measuring 200 mm x 185 mm x 98 mm with an approximate volume of 1800 cc. It raises the diaphragm to the right and displaces the kidney caudally in the absence of biliary duct dilatation. (See Figure 3). It was decided to follow conservative treatment and antibiotic therapy completing 9 days of intravenous amoxicillin/sulbactam and then 8 days on intravenous cefotaxime/metronidazole. Twenty days after surgery, an abdominal ultrasound was performed that revealed a smaller liver compared to the previous image (1000 cc of subcapsular fluid approximately). In view of this report and due to the patient’s clinical improvement, it was decided to discharge the patient on oral antibiotic therapy.
During the outpatient control 10 days after discharge, it was confirmed that fever and asthenia persisted, which is why the case was referred to the percutaneous surgery unit, where it was decided to place multipurpose drainage via percutaneous access. A total of 1400 cc of dark hematic fluid was removed. Twentyfour hours later the patient was discharged with drainage slope and outpatient control, which is the state in which the patient remains to this date.
(1%-to-7%) followed by acute cholangitis (1-4%), bleeding (1%), and duodenal perforation (less than 1%). The procedural mortality rate following an intervention is 0.2%. Other rarer complications are the formation of hepatic abscesses, paralytic ileus, pneumothorax, pneumomediastinum, and SHH(3.4). SHH is among the rarest complications of this procedure, only 62 cases have been reported by the medical literature to this date5. The mechanism of this complication is not yet fully understood. The main hypothesis on how the biliary duct lesion is caused is the use of the guidewire when the choledochus is being cannulated, which may be damaging the hepatic parenchyma and tearing the adjacent blood vessels, thus causing the hematoma. Another hypothesis would be that the lesion is due to the traction exerted by the balloon extractor, which ruptures both the biliary canaliculi and the blood vessels consequently causing the hematoma6.
A total of 14 out of the 62 cases reported presented with ruptured hematoma, a complication often occurring as a surgical emergency starting with abdominal pain, low blood pressure and hypovolemic shock resulting in death in 4 of the cases reported (7.5%)5.
Another form of presentation is the one that occurred in the present case, which was an incidental finding during a post-ERCP laparoscopic cholecystectomy showing symptoms 48 hours after the endoscopic procedure. Symptom onset in the medical literature was variable; the case of most delayed onset described was 15 days after the ERCP.
Treatment depends on each case. Hemodynamically stable patients can be treated conservatively. This case was treated with antibiotic therapy and percutaneous drainage. Cases that present with hemodynamic instability like ruptured hematoma should be treated with emergency surgery5.6.
REFERENCES
1. Baron TH, Mallery JS, Hirota WK, Goldstein JL, Jacobson BC, Leighton JA, et al. The role of endoscopy in the evaluation and treatment of patients with pancreaticobiliary malignancy. Gastrointest Endosc. noviembre de 2003;58(5):643-9. [ Links ]
2. ASGE Standards of Practice Committee, Maple JT, Ben-Menachem T, Anderson MA, Appalaneni V, Banerjee S, et al. The role of endoscopy in the evaluation of suspected choledocholithiasis. Gastrointest Endosc. enero de 2010; 71(1): 1-9. [ Links ]
3. García-Cano Lizcano J, González Martín JA, Morillas Ariño J, Pérez Sola A. Complicaciones de la colangiopancreatografía retrógrada endoscópica: Estudio en una unidad pequeña de CPRE. Revista Española de Enfermedades Digestivas. marzo de 2004; 96(3): 163-73. [ Links ]
4. Freeman ML. Complications of endoscopic retrograde cholangiopancreatography: avoidance and management. Gastrointest Endosc Clin N Am. julio de 2012; 22(3):567-86. [ Links ]
5. Pivetta LGA, da Costa Ferreira CP, de Carvalho JPV, Konichi RYL, Kawamoto VKF, Assef JC, et al. Hepatic subcapsular hematoma post-ERCP: Case report and literature review. Int J Surg Case Rep. 6 de junio de 2020; 72:219-28. [ Links ]
6. Baudet J-S, Arguiñarena X, Redondo I, Tadeo E, Navazo L, Mendiz J, et al. Hematoma hepático subcapsular. Una rara complicación de la CPRE. Gastroenterología y Hepatología. 1 de febrero de 2011; 34(2):79-82. [ Links ]
Received: February 18, 2022; Accepted: July 19, 2022











 texto em
texto em