Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Cirugía paraguaya
versão On-line ISSN 2307-0420
Cir. parag. vol.46 no.2 Asunción ago. 2022
https://doi.org/10.18004/sopaci.2022.agosto.25
Case report
Antibiotic therapy as first step in the step-up approach. Case report
1Hospital Regional Salto, Uruguay
El objetivo del presente trabajo es describir un caso clínico de un paciente que presentó necrosis pancreática infectada y se trato de manera conservadora. Resultados: Si bien el primer paso del Step up Approach lo constituye el drenaje percútanlo, en casos seleccionados podrían manejarse con tratamiento médico. Conclusión: La antibioticoterapia está indicada siempre que se demuestre infección, en pacientes seleccionados podría ser el único tratamiento, se necesitan más estudios que lo avalen.
Palabras clave: Necrosis Pancreática Infectada; tratamiento antibiótico
Introduction: The objective of this study is to describe the case report of a patient with infectious pancreatic necrosis who was treated conservatively. Results: Although the first step of the step-up approach is percutaneous drainage, in selected cases, patients could be managed with medical treatment. Conclusion: antibiotic therapy is indicated if the presence of an infection is confirmed. In selected patients, it could be the only treatment. Still, further validation studies are needed.
Keywords: Infected pancreatic necrosis; antibiotic treatment
INTRODUCTION
Pancreatic necrosis can occur in 10% of the patients with acute pancreatitis and it is associated with a mortality rate from 15% to 20%. In confirmed infectious pancreatic necrosis, patients benefit from a minimally invasive approach focused on percutaneous drainage and/or endoscopic debridement (step-up approach). In selected cases of patients without multiorgan failure, antibiotic and conservative treatment can be used. This is the case report of infectious pancreatic necrosis where conservative treatment was performed.
CASE REPORT
Thirty-seven-year-old obese male patient. Consultation due to epigastric pain and neurovegetative syndrome. Physical examination: jaundice. Blood testing: total bilirubin levels of 5.46 mg/dL, direct bilirubin levels of 3.28 mg/dL. Amylasemia 3000 IU.
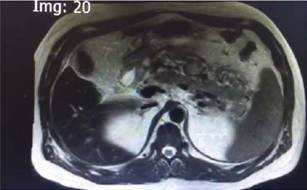
Abdominal ultrasound: multiple vesicular lithiasis, mobile, biliary pathway and pancreas not evaluable due to pain. Computed tomography scan: edematous pancreas. At 72 hours: persistent epigastric pain, bilirubin of 22mg/dL. Magnetic resonance cholangiopancreatography: slim biliary duct, contrast passage to duodenum, free biliary duct not confirmed (Figure 1). Endoscopy and papillotomy are performed, and biliary sludge and murky bile are extracted. Partial remission of pain, oral pathway reintegrated, torpid evolution. At 21 days epigastric pain and fever reoccur, with rising leukocytes. Computed tomography scan shows necrotic collection located in the epiploic transcavity, in the anterior sector of the pancreas from head to tail, there appears to be gas inside. Magnetic resonance imaging show necrotic collection of heterogeneous content (Figure 2). The watchful waiting approach is maintained based on antibiotic treatment with meropenem for 14 days, oral pathway suspended, parenteral nutrition, and proper pain management.
Infectious humoral parameters within normal ranges. Control computed tomography scan at 6 weeks reports small collection in the pancreatic tail, further cholecystectomy and cholangiography without any inconveniences.

Figure 1: Magnetic resonance cholangiopancreatography. Intra and extrahepatic billiary duct can be seen, contrast passage to duodenum, free biliary duct not confirmed.
DISCUSSION
Infectious pancreatic necrosis should be treated in a joint multidisciplinary approach with a gastroenterologist, surgeon, interventionist radiologist, intensivist, infectologist, and nutrition team². The infection pathogenesis is cause for debate although multiple pathways are considered, hematogenous, biliary, enteral, and bacterial translocation.
Antibiotic therapy is indicated in the presence of an infection or when there is imaging suspicion (eg, gas in necrotic collection) antibiotics with good pancreatic penetration if there are no other gastrointestinal alterations: the intestinal mucosa barrier is maintained and it prevents bacterial translocation, reduces infectious complications, organ failure, and mortality². When it is not possible, enteral nutrition can be performed through a nasogastric/jejunal or total parenteral feeding tube. In infectious pancreatic necrosis the first step of treatment begins with antibiotic therapy and percutaneous drainage delaying surgery. Its disadvantage is a higher risk of pancreaticocutaneous fistula. Drainage of early mini-invasive Wall of Necrosis has a Level of Evidence 1A; 1C to know when it is timely indicated, and 2C for sterile necrosis².
Step #2 is minimally invasive necrosectomy, which can be through endoscopy, video endoscopy (VARD Technique) or laparoscopy.
Pancreatic debridement should be avoided in the early acute stage (first 2 weeks because it increases both morbidity and mortality), and delayed until week#4¹.
The definition of pancreatitis severity both in the acute and in the early phase depends on organ failure. A prospective observational cohort study that analyzed organ failure and infection obtained an OR of 16.72; 95%CI, 7.04-32.56. P < .001. as opposed to pancreatic necrosis (OR, 1.73; 95%CI, 1.14-2.98. P = .008), multiorgan failure having the greated impact on mortality.
In our patient, given the clinical situation (hemodynamically stable and without organ failure), medical treatment was maintained in the intermediate care unit, antibiotic therapy was started, enteral nutrition, fluid resuscitation, and pain control.
Clinical improvement was observed at 24-48h. We should mention that our patient never had organ failure, which is why we chose to start antibiotic therapy and keep watchful waiting. The opportunity to perform a cholecystectomy in the presence of severe pancreatitis should be taken after week #6 or with evidence of imaging resolution³.
REFERENCES
1. Van Grinsven J, van Dijk S, Dijkgraaf M, Boermeester M, Bollen T, Bruno M et al. Postponed or immediate drainage of infected necrotizing pancreatitis (POINTER trial): study protocol for a randomized controlled trial. Trials. 2019; 20(1). DOI: 10.1186/s13063-019-3315-6. [ Links ]
2. Baron TH, DiMaio CJ, Wang AY, Morgan KA. American Gastroenterological Association Clinical Practice Update: Management of Pancreatic Necrosis. Gastroenterology. 2020 Jan; 158(1): 67-75.e1. doi: 10.1053/j.gastro.2019.07.064. [ Links ]
3. LeppäniemI A, Tolonen M, Tarasconi A, Segovia-Lohse H, Gamberini E, Kirkpatrick A, Ball C, et al. WSES guidelines for the management of severe acute pancreatitis. World J Emerg Surg. 2019 Jun 13; 14:27. doi: 10.1186/s13017-019-0247-0. [ Links ]
4. Boxhoorn L, Voermans R, Bouwense, S Bruno M, Verdonk C, Boermeester A, van Santvoort HC, Besselink M. Acute pancreatitis. Lancet. 2020 Sep 5; 396(10252): 726-734. doi: 10.1016/S0140-6736(20):31310-6. [ Links ]
5. Guo Q, Li A, Xia Q, Liu X, Tian B, Mai G, Huang Z, Chen G, et al. The role of organ failure and infection in necrotizing pancreatitis: a prospective study. Ann Surg. 2014 Jun; 259(6):1201-7. doi: 10.1097/SLA.0000000000000264. [ Links ]
Received: December 01, 2021; Accepted: May 01, 2022











 texto em
texto em