Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Cirugía paraguaya
versão On-line ISSN 2307-0420
Cir. parag. vol.46 no.2 Asunción ago. 2022
https://doi.org/10.18004/sopaci.2022.agosto.22
Case report
Mechanochemical intravenous ablation (MOCA) of saphenous vein with the Clarivein® Catheter. First experience at Centro Paraguayo de Varices (CEPAVA), Paraguay. Report of the first 3 cases.
1Universidad Nacional de Asunción, Hospital de Clínicas. San Lorenzo, Paraguay
2Hospital Metropolitano de Maringá, Brasil
Los procedimientos endovenosos térmicos son los procedimientos de elección en el tratamiento de las varices por insuficiencia de la vena safena en la actualidad. Sin embargo, estas técnicas requieren anestesia tumescente, lo que incrementa las molestias y el dolor durante el procedimiento. Así mismo, el calor produce malestar postoperatorio y conlleva un riesgo de lesión neurológica y de la piel. La ablación mecánico química con el catéter ClariVein®, al no emplear anestesia tumescente ni calor, se asocia con una baja tasa de dolor durante y después del procedimiento, un menor riesgo de lesión neurológica y de la piel, con unas tasas de oclusión anatómica y de mejoría en las escalas de severidad y de calidad de vida similares a las técnicas de ablación térmica en el corto plazo.
Palabras Claves: procedimientos endovenosos; varices; vena safena; ablación mecánico química; catéter ClariVein
Currently, thermal intravenous procedures are the procedures of choice to treat varices due to saphenous vein insufficiency. However, these techniques require tumescent anesthesia, which increases discomfort and pain during the procedure. In addition, heat causes postoperative discomfort and is associated with a risk of neurological and skin lesions.
Since mechanochemical ablation with the ClariVein® catheter does not use tumescent anesthesia or heat, it is associated with a low rate of pain during and after the procedure, less risk of neurological and skin lesions, and anatomical occlusions, and better rates on the severity and quality of life scales similar to those of thermal ablation techniques in the short term. We describe the results of the first three patients treated at Centro Paraguayo de Varices.
Keywords: endovenous procedures; varicose veins; saphenous vein; chemical mechanical ablation; ClariVein catheter
INTRODUCTION
Intravenous ablation of saphenous insufficiency through mini mally invasive thermal intravenous procedures such as EVLA laser and radiofrequency have become the treatments of choice for the management of varices with 90% occlusion rates. As a matter of fact, since 2005, it has been performed at the Centro Paraguayo de Varices (CEPAVA) with few complications, minimal scarring, and short recovery times.(1-3 The need for tumescent anesthesia in these procedures increases the patient’s discomfort during the procedure. Also, there are times that the thermal effect in both procedures has been associated with neurologic and skin damage as potential complications during the postoperative period.(4 Ultrasound-guided intravenous chemical ablation (EVCA) is another tool in the therapeutic armamentarium to treat venous insufficiency that does not require tumescence, but does require several sessions and it has worse results compared to thermal procedures.(1.2.5-6) The MOCA procedure with the ClariVein® catheter does not require tumescent anesthesia and it prevents nerve and skin le sions since it does not require thermal energy, with occlusion rates between 94% and 97%.(7) The objective of this article is to present the early experience with MOCA with the three first cases performed in Paraguay at CEPAVA.
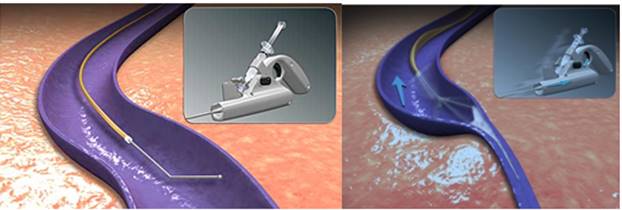
CASE PRESENTATION
The patients were previously assessed at the Centro Paraguayo de Varices (CEPAVA) and Hospital de Clínicas de la Facultad de Ciencias Médicas de la Universidad Nacional de Asunción, both based in Paraguay. All patients were examined with lower limb venous color Doppler ultrasound in the dorsal recumbent and standing positions. After that, three female patients between 28 and 37 years of age were selected. One of them had congenital aphasia with a diagnosis if venous insufficiency of internal sa phenous vein with reflux > 1 second both at the saphenofemoral junction and the saphenous trunk up to the distal third of the thigh unilaterally. The size of the saphenous trunk went from 7 mm to 10 mm as maximum diameters. The procedure was performed at the CEPAVA. All punctures were ultrasound-guided, after marking and locally anesthetizing the puncture site, with a 16 G needle and introduction of a 5-Fr catheter using Seldinger technique. The catheter of the previously armed ClariVein® device is introduced and ultrasound-guided until its tip is positioned 2 cm away from the SFJ. Tumescent anesthesia is not used here. The device is activated (fig. 1 ) with a maximum spinning speed of 3500 rpm and removed at a speed of 1 cm every 6 to 7 seconds as 2% liquid polidocanol is instilled across the entire trajectory of the vein treated with a dose of 10 cc (fig. 2). At the end of the procedure the target limb is wrapped up with an elastic bandage and the patients are discharged 30 minutes later with indications to keep the elastic bandage on for 48 hours, which will be later exchanged for 20-30 mmHg elastic compression socks for 2 weeks. Also, patients are instructed to come back for follow-up examinations in this period of time and take common analgesic drugs if they feel discomfort. Patients were controlled 24 hours, 72 hours, and 1 month after the procedure with ultrasound controls. No major complications were reported (deep vein thrombosis (DVT), pulmonary thromboembolism (PTE)). Mild ecchymosis was reported at the puncture site. The patients reported grade 1-2 pain on a scale of 10 during the procedure. None of the three patients used analgesic drugs in the postoperative period or presented with nerve or skin lesions. Three months after the procedure, it was reported that the three patients showed total occlusions of the saphenous trunk.
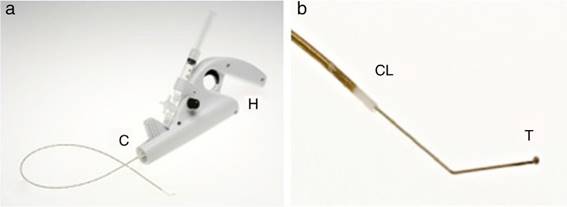
Figure 1. Panel a: the ClariVein® device consists of a motor (H) and an infusion catheter (C). Panel b: metal guidewire distal border—the sclerosant agent spreading element—protrudes outside the catheter (CL) with an angled tip (T).
DISCUSSION
The need to include minimally invasive techniques to treat varices, as well as the huge success reported with thermal techniques using local anesthesia like intravenous laser and radiofrequency made us go on with our research with this new method: MOCA with Clarivein® catheter that happens to be highly effective and requires no tumescent anesthesia, adding 2 different types of venous lesions in the treatment; 1) mechanical damage caused by the tip of the catheter rotating inside the vein, and 2) chemical sclerosis. Many studies have confirmed the efficacy and safety profile of the MOCA treatment with occlusion rates above 94%/97%,1-4.7) not only for the great saphenous vein (GSV), but also for the small saphenous vein (SSV). No major complications like DVT, PTE or nerve lesion were reported. Procedural time and pain during and after the procedure are significantly smaller com pared to RF and EVLA.(7) In the largest study published to this date,3) Van Eekeren et al. assessed 268 incompetent limbs of 210 GSV, 44 SSV, and 14 anterolateral tributaries. The occlusion rate was 99% at 6 weeks and 94% at 6 months. Superficial thrombo phlebitis was repoted in the target vein, and hematomas in the venous access in 21% and 26% of the cases, respectively. (3 No major complications were reported, although thrombophlebitis, indurations, localized hematomas, and mild hyperpigmentation were reported at the puncture site.4 Mechanochemical ablation has been associated with less postoperative pain and faster recovery times compared to thermal intravenous techniques.
REFERENCES
1. Van den Bos R, Arends L, Kockaert M, Neumann M, Nijsten T. Endovenous therapies of lower extremity varicosities: A meta-analysis. J Vasc Surg. 2009 Jan; 49(1):230-9. doi: 10.1016/j.jvs.2008.06.030. [ Links ]
2. Rasmussen LH, Lawaetz M, Bjoern L, Vennits B, Blemings A, Eklof B. Randomized clinical trial comparing endovenous laser ablation, radiofrequency ablation, foam sclerotherapy and surgical stripping for great saphenous varicose veins. Br J Surg. 2011 Aug; 98(8):1079-87. doi: 10.1002/bjs.7555. [ Links ]
3. National Institute for Health and Care Excellence. Varicose veins in the legs pathway. (CG168) (CG168) http://guidance.nice.org.uk/CG168 (Published: 24 July 2013, accessed 1 May 2014). [ Links ]
4. van Eekeren RRJP, Boersma D, Konijn V, de Vries JPPM, Reijnen MMJP. Postoperative pain and early quality of life after radiofrequency ablation and mechanochemical endovenous ablation of incompetent great saphenous veins. J Vasc Surg. 2013 Feb; 57(2):445-50. doi: 10.1016/j.jvs.2012.07.049. [ Links ]
5. van Eekeren RRJP, Boersma D, de Vries JPPM, Zeebregts CJ, Reijnen MMJP. Update of endovenous treatment modalities for insufficient saphenous veins-a review of literature. Semin Vasc Surg. 2014 Jun; 27(2): 118-36. doi: 10.1053/j.semvascsurg.2015.02.002. [ Links ]
6. Bishawi M, Bernstein R, Boter M, Draughn D, Gould C, Hamilton C, et al. Mechanochemical ablation in patients with chronic venous disease: A prospective multicenter report. Phlebology. 2014 Jul; 29(6):397-400. doi: 10.1177/0268355513495830. [ Links ]
7. Nicolaides A, Kakkos S, Eklof B, Perrin M, Nelzen O, Neglen P, et al. Management of chronic venous disorders of the lower limbs Guidelines according to scientific evidence. Int Angiol. 2018 Jun; 37(3):181-254. doi: 10.23736/S0392-9590.18.03999-8. [ Links ]
3Conflicts of interest: declared no conflicts of interest whatsoever. In addition, they claim ownership on the copyrights for the publication of the images being used.
Received: February 09, 2022; Accepted: April 10, 2022











 texto em
texto em