INTRODUCTION
Tuberculosis (TB) is the ninth leading cause of death worldwide and the main cause as a single infectious agent, which places it above HIV/AIDS1,2. The challenges for the year 2020 of the "End Tuberculosis" strategy consist of reducing the absolute number of deaths by 35% and the incidence rate by 20%, compared to 2015, as well as ensuring that no family affected by TB must assume the high costs generated by the disease3.
Latin America is home to around 600 different indigenous groups, with a total population of 26.3 million. The living conditions of these populations are deficient, often presenting poverty, marginalization, and precarious health conditions. Mexico, Bolivia, Guatemala, Peru and Colombia gather 87% of the indigenous people of Latin America and the Caribbean, with a population that is between a maximum of 9.5 million (Mexico) and a minimum of 1.3 million inhabitants (Colombia)4.
The Paraguayan population that self-identifies as indigenous belongs to 19 ethnic groups that are distributed in 5 different linguistic families: Guaraní (Aché, Avá Guaraní, Mbya, Pai Tavytera, Guaraní Ñandeva, Guaraní Occidental), Maskoy (Toba Maskoy, Enlhet Norte, Enxet Sur, Sanapaná, Angaité, Guaná), Mataco Mataguayo (Nivaclé, Maká, Manjui), Zamuco (Ayoreo, Yvytoso, Tomáraho) and Guaicurú (Qom). According to 2017 statistics, the indigenous population of Paraguay is 122,461 people while the total population of Paraguay was 6,355,000 people in the same period.
Indigenous communities of the Americas have been identified as highly vulnerable to TB and have higher rates of TB morbidity and mortality than other groups. In Paraguay, 12.1% of the cases correspond to the indigenous population; with a reported incidence of 245 cases per 100.000 people in 2019 while in the total population of Paraguay the incidence was 39,5 cases per 100.000 in the same year5.
According to the United Nations Department of Public Information (DPI - NGO), (2010), “due to poverty, tuberculosis continues to disproportionately affect indigenous peoples across the globe. Even though tuberculosis control programs have been developed, these often do not benefit indigenous peoples due to issues related to poverty, precarious housing, lack of access to medical services and medicines, cultural barriers, linguistic differences, and geographical distance”6,7,8.
The National Tuberculosis Control Program in Paraguay (PNCT in Spanish) is the entity in charge of the Ministry of Public Health and Social Welfare to carry out the active search for cases, diagnosis, and treatment of patients with TB. The Program is expanding the use of molecular biology methods for diagnosis and is testing artificial intelligence for X-Ray images diagnosis.
In this study, the objective was to determine the epidemiological characterization, incidence, and prognostic factors of TB in indigenous patients of Paraguay in the years 2018-2022 to observe the historical panorama in this vulnerable population.
METHODS
A retrospective cohort study was carried out in indigenous patients diagnosed with TB whose data are registered in the National Tuberculosis Program of Paraguay, from January 2018 to July 2022. In Paraguay 100% of the Health Regions incorporate a TB/HIV epidemiological surveillance system in accordance with their epidemiological reality and carry out collaborative activities, 100% of the Health Regions carry out comprehensive multidrug-resistant tuberculosis (MDR-TB) surveillance within the TB Directly Observed Treatment Short-course or Tratamiento Acortado Estrictamente Supervisado (DOTS or TAES strategy). The TB laboratory network is integrated into the PNCT and complies with the established standards.
Data from patients who were incomplete in variables of interest to the study were excluded. The following variables were collected: sociodemographic variables, type of diagnosis, anatomical location, resistance to treatment, history of previous treatment, incidence of TB in the indigenous population. History of evolution: dead, alive with criteria of persistence, recurrence, or cure of the disease, lost to follow-up.
Access to the data from the Expert Program (software) was requested through a note addressed to the National Tuberculosis Program. Quality control was carried out with the Excel tool, verifying duplicates and inconsistencies. The Stata 17 program was used for data analysis.
Ethical issues
The privacy of the personal data of the patients was respected. This study was approved by the Research Ethics Committee of the National Institute of Health.
RESULTS
The indigenous population with TB in the period 2018-2022 was 1659, who were between 0 and 20 years old (25.4%), mostly was female (54.6%), and residing in Presidente Hayes (22.4%) in the rural area (74.3%), of the Mbya ethnic group (20.4%). Table 1 shows that 94.5% of the study population started treatment and 69.2% had a bacteriological diagnosis, 88.3% corresponded to new cases, 1.1% presented drug resistance, 96.1% had a pulmonary location, and 11.2% died.
Table 1. Demographic and clinical characteristics, new cases and mortality of the indigenous population with tuberculosis in Paraguay, 2018-2022. N: 1659
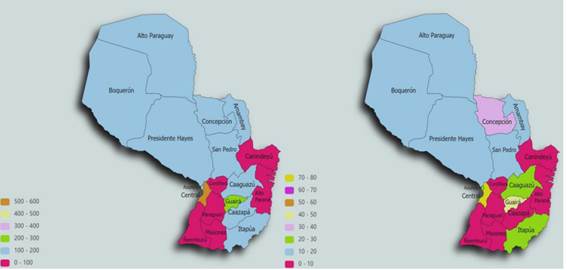
The number of new cases of TB in indigenous people was 307 in 2018, this figure increased in 2019 to 336, then in 2020 and 2021 it decreased to 286 and 319 respectively. In the study period of 2022, 216 new cases of TB were found. Figure 1 shows the incidence by geographical distribution. The incidence is more concentrated in Asunción and Central Department followed by the Guairá Department. The incidence of TB was associated with age and area of residence, being more incident in the youngest. The incidence was not associated with the HIV risk factor (Table 1).
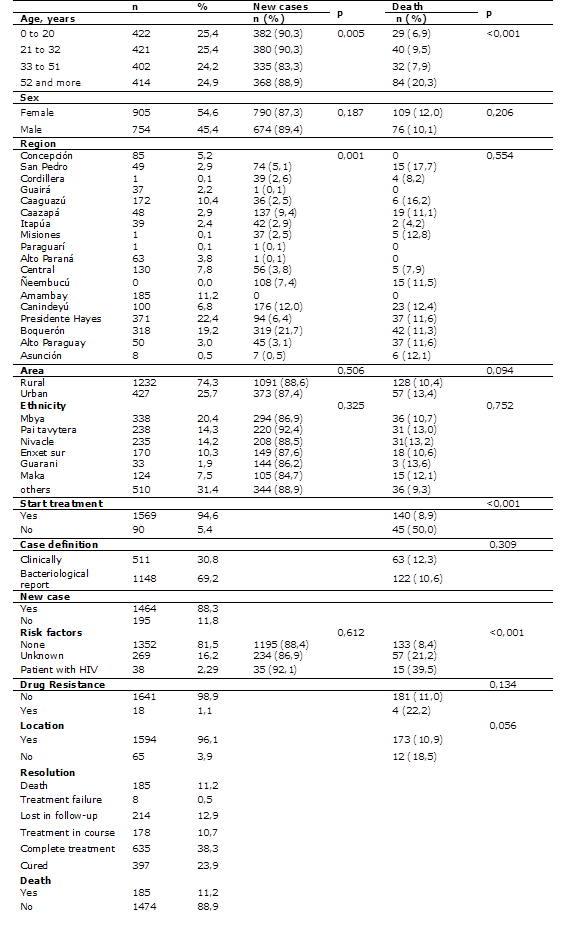
The highest number of deaths occurred in 2019 with 47 cases. In the first half of 2022, 26 patients with TB have died during the study period. Figure 1 shows the mortality by geographical distribution. The mortality is more concentrated in Asunción and Central Department, followed by Guairá and Concepción Departments. Mortality was associated with age, with the elderly being the most likely to die. Mortality was also associated with treatment and HIV co-infection, with those who did not initiate being more likely to die, as were those with HIV (Table 1). An older person, who did not start treatment, and who is coinfected with HIV is more likely to die from TB (Table 2).
Table 2. Multivariate analysis of risk factors associated with mortality in the indigenous population of Paraguay, 2018-2022. N: 1659
| OR (IC 95%) | OR* | p | AOR** | p |
|---|---|---|---|---|
| Age, years | ||||
| 0 to 20 | ref | ref | ||
| 21 to 32 | 1,17 (0,69 - 1,92) | 0,551 | 0,85 (0,48 - 1,50) | 0,586 |
| 33 to 51 | 1,42 (0,86 - 2,35) | 0,166 | 1,26 (0,74 - 2,75) | 0,385 |
| 52 and more | 3.44 (2,20 - 5,38) | <0,001 | 3,26 (2,03 - 5,24) | <0,001 |
| Start treatment | ||||
| Yes | ref | ref | ||
| No | 10,20 (6,52 - 15,97) | <0,001 | 9,82 (5,42 - 17,7) | <0,001 |
| Risk factors | ||||
| None | ref | ref | ||
| Unkown | 2,94 (2,07 - 4,18) | <0,001 | 1,25 (0,76 - 2,06) | 0,364 |
| VIH | 7,15 (3,62 - 14,09) | <0,001 | 9,86 (4,84 - 20,1) | <0,001 |
*Odds Ratio
**Adjusted Odds Ratio
DISCUSSION
In this study, the indigenous population with TB in the period 2018-2022 were mostly new cases, of which 11.2% died. The incidence of tuberculosis was associated with age and area of residence while mortality was associated with age, lack of treatment and coinfection of HIV.
In seven high-burden countries, an increase in the reported incidence rate has been observed between 2014 and 2018, with 82% in Venezuela, 58% in El Salvador, 6% in Brazil and Mexico, and 5% in Argentina2. In Peru, 702 indigenous people were found to have TB, making it evident that the incidence of TB in these indigenous populations is higher than that of the general population (106 per 100,000 inhabitants.)7. In the Aymara districts, an average incidence of smear-positive pulmonary TB of 33.35 per 100,000 inhabitants was identified8.
In this study, between 216 and 336 new cases were observed during the years 2018 to 2022, thus being one of the highest in the indigenous population in the region. In some studies, it is considered that being indigenous is a predisposing factor for TB9,10. Although the incidence rates are high in the departments of the Western Region, their low population density implies a lower number of cases in absolute numbers, which present a wide geographical dispersion compared to the rest of the country. On the other hand, the Central, Alto Paraná and Asunción departments, despite having lower rates, present 60% of the disease burden in the country.
The main obstacles to TB control in the population are difficulties of access; not only because of the distances, but also because of the lack of roads, the lack of roots on the part of certain groups, the overcrowding due to the lack of adequate housing and, in certain cases, the interpretation of TB as an “inflicted curse”. The living conditions of these populations are deficient, since there is often poverty, marginalization, and poor health conditions4. The high rates of poverty, unemployment, illiteracy, and unsatisfied basic needs that occur in the indigenous population contribute to the increase in TB cases in the population11. Indigenous settlements and rural dwellers are at high risk of TB12.
Regarding mortality, it is also high in this population, being related to the risk factor of coinfection with HIV as in other similar studies (13,14). Drug resistance is also a factor to consider15-18, although due to the few cases found in this study it is difficult to find an association. Observing the historical series, the TB mortality presents a relatively stable curve with an upward trend, probably due to improvements in the registration system or due to TB/HIV coinfection and late diagnosis.
As a limiting factor, there is the lack of some important data such as other risk factors, data not provided by the PNCT. It is important to establish actions focused on the indigenous population to stop the continued transmission of TB, for which more studies are necessary to understand the dynamics of TB transmission there. In order to control the infection in these populations identified as especially vulnerable, it is necessary to respond to their diverse needs from an intercultural perspective, that considers the value of their cultural practices, including their ways of life, their value systems, their traditions and worldviews.
New cases and mortality from TB in the indigenous population are high. The incidence of TB is associated with age and area of residence being more incident in the youngest and in the Presidente Hayes area. The elderly, who did not start treatment, and who are coinfected with HIV are more likely to die from TB.
There is a need to improve Primary Care, and adequate screening, treatment monitoring and prevention measures, as well as expanding studies on comorbidities in the first level of care, due to the high concentration of patients in this vulnerable population.