Introduction
HIV is not only a public health problem, since once widespread, the epidemic has far-reaching consequences for all social sectors and for the development itself. It can decimate the workforce, create large numbers of orphans, exacerbate poverty and inequality, and place tremendous pressure on health and social services1. According to data from the Ministry of Public Health and Welfare (MSPyBS), since the beginning of the epidemic in 1985, until 2021, a total of 25 050 people were registered with an HIV diagnosis, of which 6 967 were categorized as AIDS and the accumulated mortality until 2022 was 9,413 cases2.
Healthcare-associated infections (HAIs) are complications that increase patient morbidity and mortality, length of hospital stay, and related costs, and have a significant impact on the healthcare system3. Few studies have evaluated HAIs in an HIV population4,5; however, studies have suggested that patients with HIV are at an increased risk of contracting an HAI because they have high rates of hospitalization and longer hospital stays, and they are at high risk of contracting infections considering their immunosuppressed status4-6.
These infections are characterized by being acquired during medical care and can be caused by bacteria, viruses, fungi, or parasites7. The risk of developing HAI is higher in patients with HIV infection than in those without. This is because HIV weakens the immune system, making it more susceptible to infections8.
The use of invasive devices, presence of opportunistic diseases, renal failure, and ICU stay are risk factors for contracting HAIs in an HIV-positive population9. Furthermore, there is no consensus on the most common HAIs in patients with HIV, and whether this population has a higher risk of acquiring HAIs caused by multidrug-resistant organisms (MDRO)10. The objective of this study was to determine mortality due to infections associated with healthcare in patients with HIV in Paraguay from January to December 2018 to 2021.
Methodology
An observational, descriptive, cross-sectional study was carried out with non-probabilistic convenience sampling on mortality due to Infections Associated with Health Care in Patients with HIV in Paraguay from January to December 2018 to 2021.
The study population consisted of people over 18 years of age who died with a diagnosis of HIV infection and IAAS of both sexes during that period. The study variables were demographic (age, sex, place of residence, population), HIV-related (Baseline CD4 count (cells/mm3), Baseline Viral Load (RNA copies/mL plasma), Stage of HIV infection at the time of diagnosis, Time from HIV diagnosis to death (months), comorbidities at the time of death, isolated microorganisms, and presence and location of IAAS.
HAIs were defined as urinary tract infections (UTI), bloodstream infections (STI), respiratory tract infections (RTI), or a combination of these infections, which developed at least 48 hours after hospital admission. If a patient was discharged and then readmitted within 72 h, this was also considered an HAI. The study was approved by the Institutional Ethics Committee, and the ethical principles of the Helsinki for biomedical research were adhered to. The data were entered into a Microsoft Office Excel© 2016 spreadsheet, after data quality control, the variables were exported and analyzed with the Stata 17.0® statistical software. The results were presented as measures of central tendency, dispersion, and a table of proportions.
Results
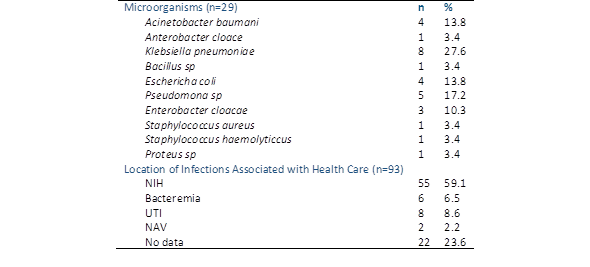
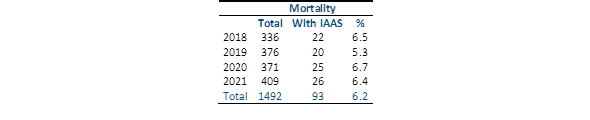
93 patients with IAAS were included in the study, of which 34.4% were between 20 and 29 years old, 19.3% were between 40 and 49 years old, 73.1% were male, and 74.2% resided in Asunción and Central. Regarding the type of population, 79.3% were in the general population, 77.6% were diagnosed with AIDS, and 68.6% had a baseline CD4 count of less than 200 cells/mm3. Of the 40.7%, the time from HIV diagnosis to death was greater than 40 months, and the most frequent comorbidity was AIDS-related cancer (Table 1). Of the microorganisms isolated from patients with healthcare-associated infections, eight were Klebsiella pneumoniae, five were Pseudomonas spp., and four were Escherichia coli and Acinetobacter baumannii. Regarding the location of the IAAS, 59.1% were due to NIH, 8.6% due to UTI, and 6.5% due to bacteremia (Table 2). The mortality rate during 2020 was 6.7%, during 2018 it was 6.5% and during 2021 it was 6.4% (Table 3).
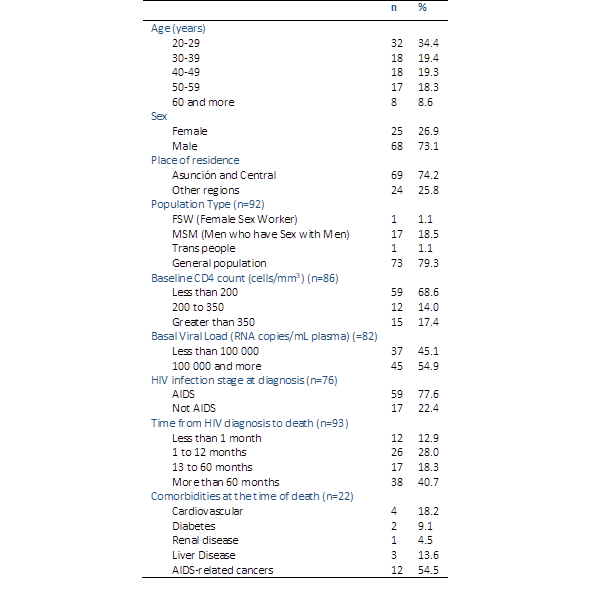
Table 1 Demographic, clinical, and laboratory characteristics of people with hiv who died from healthcare-associated infections between 2018 and 2022 (n=93
Discussion
Mortality due to HIV/AIDS is mainly associated with late diagnosis, poor adherence to treatment, and no treatment11. These factors favor an increase in opportunistic infections and neoplasia, which are responsible for most deaths in untreated patients3,12. Furthermore, virological failure is associated with high mortality, which highlights the need to pay greater attention to this at-risk population, and in untreated cases, death usually occurs two years after the onset of clinical symptoms3,9.
The fact that most patients in this study were diagnosed with AIDS indicates that the infection was detected at an advanced stage. Hu X et al.12) and Khan MA13) highlighted that this may be due to factors such as lack of access to medical care, stigmatization, and discrimination faced by people with HIV/AIDS.
A low baseline CD4 count is an indicator of advanced infection14. CD4 is a type of white blood cell that helps the immune system fight infections. When the CD4 count is low, the immune system is weakened and more susceptible to opportunistic infections, which predisposes to HAIs, as highlighted by Castro-Lima VAC et al.6) and Rojas D7.
Although the study found a long time from HIV diagnosis to death, it indicates that the disease progressed slowly, which differs from the findings of Gao et al.15, GBD 2015 Mortality and Causes of Death Collaborators16, and Deng et al.17. Late diagnosis continues to represent a problem in Paraguay, with a significant diagnostic gap owing to the country's diagnostic gap2. The most frequent comorbidity was AIDS, which indicates that opportunistic infections were the most common cause of death in these patients2,3. The high prevalence of IAAS in patients with HIV is explained by immunosuppression caused by the virus. HIV attacks cells of the immune system, hindering their ability to fight infections. Consequently, HIV patients are more susceptible to bacterial, fungal, and viral infections18-20.
In general, the results of this study showed that HIV/AIDS infection in Paraguay continues to be a public health problem that disproportionately affects men. Diagnosis remains late in the advanced stages of the disease in both sexes, with a high mortality rate. Measures need to be implemented to improve access to diagnosis, medical care, and infection prevention to reduce the impact of the disease on public health. The combined prevention strategy for HIV infection, defined by the UNAIDS, aims to reduce new HIV infections. Furthermore, it was found that during this study, 1492 people died, of which 6.2% were attributed to IAAS and remained constant during the four years of the analyzed cohort.
The limitations of the study mainly focus on the quality of the information available on HIV-related deaths; therefore, it is extremely relevant to propose strategies to improve the quality of the information. In conclusion, it is possible to indicate that people with HIV, especially those who have been diagnosed in advanced stages of the disease, are more likely to develop HAIs and are related to mortality. This is due to the presence of multiple opportunistic infections and comorbidities that favor a high number of hospitalizations and longer hospital stays.