Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Cirugía paraguaya
versión On-line ISSN 2307-0420
Cir. parag. vol.48 no.1 Asunción abr. 2024
https://doi.org/10.18004/sopaci.2024.abril.34
Case report
Ludwig's angina asociate with acute mediastinitis as a consequence of a non odontogenic infection. Case report. Instituto de prevision social
1Hospital Central del Instituto de Previsión Social, Servicio de Cirugía General. Asunción, Paraguay.
The 70-90% of Ludwig’s angina cases are due to dental origin, a lower percentage correspond to cases of sialadenitis, peritonsillar abscesses, and mandibular trauma. There are few reports of non-dental origin cases, making this cause a rare condition. The treatment is similar in both cases: with early diagnosis, directed antibiotic therapy and a good surgical drainage.
Keywords: Submaxilitis; angina; Surgical drainage
El 70-90% de los casos de angina de Ludwig se deben a procesos infecciosos de origen dental. Un menor porcentaje se deben a casos como: sialoadenitis, abscesos amigdalinos o trauma maxilofacial. Existen pocos reportes de casos de orígenes no odontogénicos, constituyendo este origen como raro. El tratamiento es similar en ambos casos, teniendo como claves: el diagnóstico temprano, antibioticoterapia dirigida y drenaje quirúrgico oportuno.
Palabras claves: submaxilitis; angina; drenaje quirúrgico
INTRODUCTION
Ludwig’s angina was described in 1836 by Doctor Wilhelm Friedrich Von Ludwig. This being a septic and generally severe process if the mouth’s soft tissue which progresses rapidly towards the neck If this infectious process cannot find an exterior drainage, it will indefectibly advance towards the thorax. It’s associated with diseases or conditions that affected the organism’s defenses such as alcoholism, malnutrition, and organ transplant. But they can be present in patients with no such conditions1.
Its diagnosis is especially based on clinical and imagery criteria. Clinical manifestations must be rapidly identified, occurrence of pain in the area, along with lockjaw and tongue elevation, which alerts an early diagnosis1.
The infection’s advance towards submandibular, sublingual, and submental spaces consequentially causes the collapse of the oropharynx and hypopharynx2.
Ludwig’s angina is of odontogenic origin in most cases (70-90%). Dental cavities or necrotizing ulcerative gingivitis are the main causes. But the non-odontogenic causes, such as submaxilitis, peritonsillar abscess or maxillary sinusitis, as well as maxillofacial trauma, represent the other 10%. Ludwig’s angina may bring forth a glottis oedema with necrotizing fasciitis and necrotizing descending mediastinitis as it progresses on, which has an increased mortality rate2.
The non-odontogenic origin triggers a similar syndrome, making the diagnosis more difficult and time consuming. The oral cavity’s inspection must be thorough and regulated. The infection starts underneath the mylohyoid muscle’s crest and progresses to deeper spaces of the neck. The retropharyngeal space, known dangerous space, works as an easy way for propagation to the mediastinum. Mediastinitis is a rare complication which results in the infection’s propagation, first to the parapharyngeal space and from there to the retropharyngeal space and upper mediastinum3.
The patient reports painful and septic-type typical facies, with local swelling and breathing difficulty, absence of lymphadenopathy and lack of frank collections are telling of this disease. Indurations with subcutaneous emphysema alongside the neck can be palped. The characteristic thickened neck can also be seen, commonly referred to as “bull neck’4.
Treatment
The treatment is directed to stop the infection’s progression with systemic antibiotics of ample specter, covering polymicrobial agents, and after the patient and air way’s stabilization, the possibility of surgical drainage is evaluated5.
The surgical treatment’s goal is to ultimately drain the collections. Whichever the handling method is, thorough drainage of the collections must be assured. Inadequate access to the neck or lack of deep spaces’ drainage would compromise the response to the surgical treatment. It’s also important to identify and treat the causing agent of Ludwig’s angina. Eliminating the causing factor on the first surgery, is the key to the initial treatment5.
Microbiology
The most commonly identified organisms in these types of origin-independent infections are the viridans streptococci. Being these agents, typical on the oral cavity. Negative gram aerobes can also be isolated, such as staphylococcus aureus, including the methicillin-resisting ones which also contribute to the deep neck space infections, especially in children, immunocompromised and other at-risk patients5.
The streptococcus anginosus (streptococcus milleri) are a particularly virulent viridans group. Many odontogenic infections may carry oral anaerobes with them such as species of Peptostreptococcus, Fusobacterium nucleatum or pigmented bacteroids (Prevotella melaninogenica and Porphyromonas spp)6.
The following is a case of a patient who developed Ludwig’s angina of non-odontogenic origin.
CASE PRESENTATION
We present the case of a male patient, 67 years old, from the Department of Paraguarí, businessman. Reports arterial hypertension currently in treatment with oral antihypertensives, non-diabetic, neither reports any other systemic pathologies. Former smoker for more than 20 years and moderate alcohol drinker.
Has an 8-day evolution history, localized stinging-type pain in the right submandibular region, which exacerbates and radiates the neck area with the passing of days. Local swelling with temperature changes and local erythema. Reports progressive dysphagia to solid food. The patient explains that the pain increased in intensity, manifesting a lack of response to domestic treatment with common analgesics and warm compresses. Furthermore, shows a decrease of the general state with feverish feeling and progressive dysphagia. The patient reports swelling under the tongue with halitosis, not related to any dental piece.
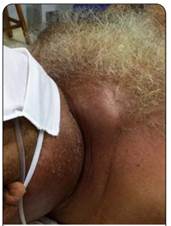
Arrives at the Hospital of the Social Prevision Institute’s emergency department 8 days after the symptoms began, in a normal general state with tachycardia, fever, evident swelling of the submandibular region, and postural respiratory distress (see figure 1 and 2).

Figure 1. inflammatory signs on the submandibular region and crackles. Patient with respiratory distress and laryngeal stridor.
Inspection of the oral cavity yields opening distress (lockjaw) along with white tongue. Dental pieces of the upper and lower maxillary show chronic periodontitis, but with no associated local acute process. Inspection of the mouth’s floor yields evident swelling, painful and erythematous, along with fetid and purulent fibrinous exudate over the mucous surface.
Laboratory tests upon admission corroborate a sepsis state with: 26,500/mm3 leukocytosis, 89% neutrophilia, 13.1g/dL hemoglobin, 37.6% hematocrit, 235,000/mm3 platelets, 5.58mg/dl total bilirubin, 61 mg/dl urea, 1.45mg/dl creatinine, 136mEq sodium, 4.2mEq potassium, 77% prothrombin time, PCR +.
Thorax X-ray upon admission: light widening of the upper mediastinum, right pleural effusion with densification of the cardiac area. No air present within the subcutaneous cellular tissue neither within the mediastinum.
CT scans were simple at 24 hours from admission to emergency services. Densification of soft tissue with air within the subcutaneous cellular tissue (submandibular, cervical, and mediastinum) was recorded. Deep neck spaces and the thorax’s anterior wall with local edemas of the soft tissues were observed to be compromised. Some liquid collections within the submandibular space. Right pleural effusion with densification of the hilar tract, and pneumomediastinum is recorded (see Figure 3 y 4 ).
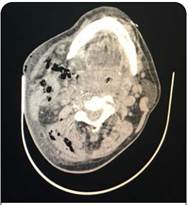
Figure 3. Air bubbles on the simple CT scan showing dissection of the planes and masseteric, pre-vertebral, and vascular spaces’ invasion.
A cervical ultrasound is performed, which does not reveal collections, only yields air within the subcutaneous cellular tissue.
The patient is admitted into the intensive care unit where antibiotic therapy with ampicillin plus 3-gram sulbactam every 8 hours begins.
Enters the operating room approximately 24 hours after being admitted into emergency services, where a fibrolaryngoscopy reveals an important glottis enema, with tracheal deviation. Orotracheal intubation is successful.
We perform a classic lateral cervicotomy over the inner edge of the sternocleidomastoid muscle, finding ample muscular and soft tissue necrosis. (see figure 5) We broaden the incision on both directions due to the infection’s extension, besides performing a tracheostomy.

Figure 5. Ample lateral cervicotomy. Abundant gangrene and fetidness of the tissues. Handling was broad, enabling access to all neck spaces. Dissection pattern of the tissues from the neck to the anterior mediastinum was noted.
We perform a debridement of all affected tissues. In the submaxillary cell we record multiple collections but partitioned in less than 1cm3. Necrosis of the glandular tissue with loss of its architecture. The authors attribute this as the possible origin due to the lack of other possible ones. Despite an exhaustive search of some dental and/or gingival infectious process in regard to the maxillofacial surgery team, no attributing origins to any dental process were found.
Due to the infection’s depth and compromising of the scalene muscles, we decided to extract fibers from the brachial plexus. We also recorded necrosis and great affection of the sternocleidomastoid, mylohyoid muscle which we redried. The main stem of the spinal nerve was sectioned and cauterized due to its viability being compromised. We recorded a septic thrombophlebitis of the inner jugular vein confirming Lemierre’s triad, whose literature cites a syndrome characterized by bacteremia, thrombophlebitis, and oropharyngeal infection. We proceeded to open the vein through a thrombectomy and double ligature of its edges.
We performed a cleanse of the surgical wound with an iodine solution and left chlorhexidine and oxygenated water compresses. The skin is handled by separated stitches for a second look of the neck. (see Figure 6)

Figure 6. Post-operative look with impregnated compresses of oxygenated water and chlorhexidine. Drainages on continuous aspiration were placed.
After 24 hours we proceeded to reinspect the neck and placed Jackson-Pratt-type aspirational drainages. We recorded purulent material egression from the mediastinum, by which along with thorax surgery we opted for an anterolateral thoracotomy.
In this operatory act, 48 hours after the patient’s admission, we performed a thoracotomy through anterolateral handling. We proceeded to the toilette and pleuro-pulmonary decortication due to a thickened pleura, and dense pleural and purulent liquid. We placed a pleural drainage tube and retro sternal tube for cleansing.
After 72 hours from admission, and on the third surgery. We noted right collarbone’s compromission with purulent material egression, by which we proceeded with its dislocation and exclusion.
The patient did not require another surgical intervention. However, through daily follow-ups and exhaustive cleansing of the operatory wound, we achieved good results.
The retrosternal tube for cleansing was utilized for 5 days, for cleaning with a physiological saline solution, it was then withdrawn. The pleural drainage tube was withdrawn on the 35th day after its placement.
Secretion farming: Streptococcus constellatus, Staphylococcus Aureus. Received antibiotic therapy of ample specter with tigecycline for 14 days, and Meropenem and Vancomycin for 20 days directed to positive Cocos and Bacilos Gram.
During in-patient time in the intensive care unit, the patient acquired a pneumonia associated to the respirator by Acinetobacter baumannii and colonization by Klebsiella pneumoniae, carbapenemases producer. The patient also developed a neck-leveled auto-limited pleuro-atmospheric fistula which did not require surgical treatment. (see Figure 7)
Major neck asymmetry with akinesia was recorded. Trapezius and deltoid muscle atrophy with non-incapacitating postural deviation.
Patient was discharged after 63 days of in-patient stay, and presents a 9-month follow-up up to this date (see Figure 8).
DISCUSSION
Ludwig’s angina had a mortality close to 100% in the pre-antibiotic era, with the arrival of antibiotics its mortality decreased to a 50%. However, its associated mortality to mediastinitis still reaches 70%5.
According to Flynn, the ideal surgical technique must assure access and communication between the involved subaponeurotic spaces assuring the change in atmosphere between the anaerobic and aerobic flora and be able to maintain enough time for the proper placement of drainages6.
We have seen patients in our practices who have been insufficiently drained, compromising their favorable evolution.
We debated with the authors of this work the “true” origin of this case. The surgical finding of a necrotic submaxillary gland with pus in its interior and the absence of other possible origins plus the isolated farming of a Viridans (Constellatus) species leads us to conclude the acute submaxilitis as the causing entity.
Post-operational follow-up of this type of patients is fundamental, with critical medicine, infectiology, and surgical equipment, farming must be varied to better adjust to the best possible antibiotic. The keys to the treatment center around 3 fundamental pillars: 1- general support measures. 2- antibiotic treatment of ample specter and 3- proper surgical treatment7.
REFERENCES
1. Calderón Peñalver Pablo Arnaldo, Rodríguez Miranda Ovidio Gustavo, Señor Castañeda Suset, García Céspedes Damarys. Angina de Ludwig. Presentación de un caso. Rev.Med.Electrón. [Internet]. 2016 Feb [citado 2023 Oct 11] ; 38(1): 87-96. Disponible en: Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1684-18242016000100009&lng=es . [ Links ]
2. Chow AW, Duran ML, UpToDate [Internet]. [citado 27 de enero de 2023]. Disponible en: Disponible en: https://www.uptodate.com/contents/deep-neck-space-infections-in-adults?search=ludwig+angina%2C+case+report&source=search_result&selectedTitle=2%7E150&usage_type=default&display_rank=2 [ Links ]
3. Fynn TR, Shanti RM, Levi MH, Adamo AK, Kraut RA. Severe odontogenic infections, part 1: prospective report - PubMed [Internet]. [citado 31 de enero de 2023]. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/16781343/ [ Links ]
4. Sears CL, Calderwood SB. UpToDate [Internet]. [citado 27 de enero de 2023]. Disponible en: Disponible en: https://www.uptodate.com/contents/ludwig-angina?search=ludwig+angina%2C+case+report&source=search_result&selectedTitle=1%7E150&usage_type=default&display_rank=1 [ Links ]
5. Wald ER, Morve SE, Gleen CI. UpToDate [Internet]. [citado 27 de enero de 2023]. Disponible en: Disponible en: https://pro.uptodatefree.ir/Show/6079 [ Links ]
6. Gagliardi Lugo AF, Contreras MG, Zeballos J. Angina de Ludwig. Reporte de 2 casos - Science Direct [Internet]. [citado 11 de octubre de 2023]. Disponible en: Disponible en: https://www.sciencedirect.com/science/article/pii/S1130055812001499 [ Links ]
7. Stevens DL, Baddour LM UpToDate [Internet]. [citado 27 de enero de 2023]. Disponible en: Disponible en: https://www.uptodate.com/contents/ludwig-angina?search=ludwig+angina&source=search_result&selectedTitle=1%7E11&usage_type=default&display_rank=1 [ Links ]
CONFLICT OF INTEREST
ETHICAL CONSIDERATIONS
FUNDING
AUTHOR’S CONTRIBUTION
Received: August 01, 2023; Accepted: April 01, 2024











 texto en
texto en