Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Cirugía paraguaya
versión On-line ISSN 2307-0420
Cir. parag. vol.48 no.1 Asunción abr. 2024
https://doi.org/10.18004/sopaci.2024.abril.28
Case report
Heyde Syndrome: surgical treatment of aortic stenosis associated with lower gastrointestinal bleeding
1Hospital General de Luque. Cirugía General, Luque, Paraguay
In many cases, the origin of lower gastrointestinal bleeding is not completely elucidated. The highest percentage of cases have their origin in the colon, with diverticula and angiodysplasias being the most common causes. Heyde syndrome is a rare diagnosis that consists of the association of GI bleeding due to angiodysplasia and aortic stenosis, due to a degenerative process and an acquired deficiency of von Willebrand factor type IIA.The objective of this work is to present a rare case of HDB, whose treatment consists of surgery.
Keywords: Lower gastrointestinal bleeding; Heyde syndrome; Von Willebrand factor; Aortic stenosis; Angiodysplasia; intestinal bleeding; Aortic valve replacement
En muchas ocasiones, el origen del sangrado gastrointestinal bajo no se dilucida completamente. El mayor porcentaje de casos tiene su origen en el colon, siendo los divertículos y las angiodisplasias las causas más comunes. El síndrome de Heyde es un diagnóstico poco frecuente que consiste en la asociación de sangrado gastrointestinal por angiodisplasia y estenosis aórtica, debido a un proceso degenerativo y un déficit adquirido de factor von Willebrand tipo IIA. El objetivo de ese trabajo es presentar un caso poco común de HDB, cuyo tratamiento consiste en cirugía.
Palabras clave: Hemorragia digestiva baja; Síndrome de Heyde; Factor de Von Willebrand; Estenosis aortica; Angiodisplasia; Sangrado intestinal; Reemplazo valvular aórtico.
INTRODUCTION
Heyde syndrome is an uncommon association amongst aortic stenosis and low intestinal bleeding, which has been a study objective in the past few years, with major advances in its physiological comprehension and treatment.1 In this work, we present a clinical case of Heyde syndrome and its evolution.
CLINICAL CASE
64-year-old male patient reports lipothymia and marked paleness to a low-complexity assistance center’s ambulatory consultation, where an acute anemia diagnosis is performed. Requested laboratory studies yield 6.9g/dL hemoglobin (Hb) and 20.7% hematocrit. Due to the results, a 2-volume concentrated red blood cells transfusion is decided and the patient is discharged with a stool guaiac test order. The following month to said consultation, the patient reports to our emergency services due to a 4-day evolution of several instances of bloody stools of moderate amounts. Does not present lipothymia, weakness, dizziness nor other accompanying symptoms. The physical exam presents vital signs within normal parameters, pale skin and mucous, without systemic repercussions. The exam also presents non-painful soft and depressible abdomen, no defenses nor irritation. Rectal examination yields hematochezia on the glove’s fingertip. The rest of the physical exam’s data does not provide valuable.
Laboratory studies are requested upon admission, yielding 8.9g/dL Hb, 27% hematocrit, 8,580/mm3 white blood cells, 66% neutrophils, 270,000/mm3 platelets, 100% prothrombin time, 0.8mg/dL creatinine, and 20mg/dL urea. The electrocardiogram upon admission yields: R precordial amplitude increase on sinus rhythm, suggesting a left ventricular hypertrophy, no ischemic changes.
An upper gastrointestinal endoscopy is performed which yields a hiatal hernia, chronic gastritis, and erosive duodenitis, while the colonoscopy shows grade II internal hemorrhoids. Upon uncertain diagnosis, a double abdomen and pelvis contrast CT scan is requested, which yields bowel wall thickening of the ascending colon and cecum, suggesting guided study assessment. (see Figure 1)
The patient is discharged stable and in good general state without signs of bleeding, 10g/dL Hb, 32.5% hematocrit, in plans of having an enteroscopy and an ambulatory-type follow-up.
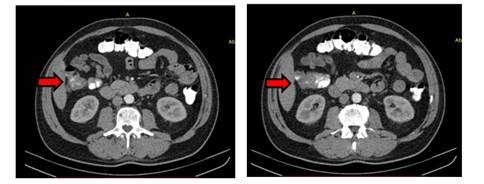
Figure 1. Double abdomen and pelvis contrast CT scan. Focal, asymmetric bowel wall thickening is observed, which compromises the ascending colon.
The patient is readmitted 6 weeks afterwards due to a 3-day evolution of hematochezia in sizable quantities, without systemic repercussions nor other accompanying symptoms. Presents 9.0g/dL Hb and 27% hematocrit upon laboratory admission.
During inpatient stay, the patient presents bloody stool persistency in great quantities (hematochezia) hence an emergency upper gastrointestinal endoscopy is performed, which did not yield valuable data. The patient remains with hidden digestive bleeding, in plans of having an angiotomography and enteroscopy.
The abdomen angiotomography yields focal bowel wall embossment of the ascending colon underneath the hepatic angle compatible with the first hypothesis through an angiodysplasia. (see Figure 2)
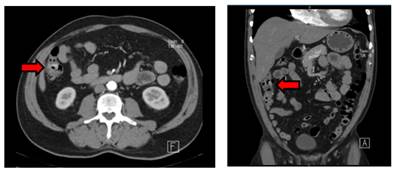
Figure 2. Abdomen angiotomography, arterial phase. Visible focal bowel wall embossment, underneath the colon’s hepatic angle. (Left: axial cut / Right: coronal cut)
With the probable diagnosis of angiodysplasia and due to the lower digestive bleeding episodes on several occasions, it is decided to prepare the patient for a total colectomy. Amongst presurgical studies, an echocardiogram is requested, which yielded a degenerative aortic valve with severe stenosis, mitral leakage, and slight tricuspid regurgitation.
Due to the gastrointestinal tract angiodysplasia’s relation with aortic stenosis, a Heyde syndrome diagnosis is reached, and aortic valve replacement is proposed as definitive treatment. Amongst requested analysis, vWF 160UI/dl antigen (regular value of 50-150UI/dl) and vWF 108UI/dl activity (50-150UI/dl) are highlighted.
The patient was treated with aortic valve replacement surgery 4 months after the diagnosis. Currently showing proper evolution without recurring bleeding to this date.
DISCUSSION
Heyde syndrome was described for the first time in the year 1958 by Dr. Edward Heyde, an intern in Vancouver. It’s an association between aortic stenosis and bleeding by intestinal angiodysplasia, the result of an acquired deficit of the von Willebrand factor (vWF) type IIA. Angiodysplasia is a degenerative disease of the intestinal mucous which predisposes gastrointestinal bleeding. Its association with aortic stenosis is well known but Heyde syndrome diagnosis is a rare case1. Aortic stenosis usually generates hemorrhagic diatheses due to high-molecular-weight multimers’ selective deficit of the vWF².
Heyde syndrome’s pathophysiology involves a loss of said multimers with an essential function in hemostasis and an altered platelet function, which favors angiodysplasia bleeding.
In its mature form, the vWF stores itself in Weibel-Palade bodies inside endothelial cells and are gradually freed into the blood flow. It serves a central function in platelet adhesion and aggression, acting as an endothelial damage detector. Likewise, it plays a crucial role in coagulation as it joins and stabilizes the VII factor (F-VII), protecting it from proteolysis and taking it to the injury’s location. The proportion in which the different vWF multimers circulate is crucial to maintain a normal hemostasis. The bigger-sized multimers have more proaggregative activity than the lesser-sized ones, being especially important in high-flux and tangential stress vascular areas, such as angiodysplasias.
From a structural perspective, angiodysplasias are characterized by being arterial or venous capillaries which are dilated and distorted, reaching up to 5mm diameter. These anomalies are located in the gastrointestinal tract’s submucous. These malformations’ peculiarity is that they lack a middle layer, which results in increased permeability and a notable predisposition to recurring bleeding. Angiodysplasias tend to predominate on the cecum and ascending colon, being able to expand from the cardia to the anal sphincter.
Both the aortic stenosis and angiodysplasias tend to increase their prevalence as age advances. There is proof that suggests that valve disease frequently triggers a hemorrhagic predisposition due to a high-molecular-weight multimers’ selective deficit of the vWF³. This deficit, known as acquired type IIA von Willebrand disease, favors angiodysplasias’ bleeding which coexist within the patient.
Hence the Heyde syndrome’s pathophysiology is concisely summarized.
These has been proved in various studies where, after aortic valve replacement, these multimers’ levels and platelet functions went back to normal values.
When there is suspicion of Heyde syndrome diagnosis, it’s crucial to investigate other possible sources of gastrointestinal bleeding, such as duodenal ulcer, diverticulosis, colon cancer and inflammatory intestinal diseases, among others. In every patient that presents gastrointestinal bleeding, it’s recommended to perform a colonoscopy to get a full and precise diagnosis.
When the presence of angiodysplasia and gastrointestinal bleeding is detected, it’s important to consider the possibility of an aortic stenosis and actively search this diagnosis to be able to reach a Heyde syndrome conclusion. This diagnosis is confirmed through specific laboratory methods, which allows a precise definition of the disease.
In our case, along with the Heyde syndrome’s probable diagnosis a dosage and von Willebrand factor activity study is requested, yielding slightly elevated vWF Ag (160UI/dl of NV of 50-150UI/dl) and vWF Normal activity (108 UI/dl of NV of 50-150 UI/dl).
It’s important to highlight that in type IIA von Willebrand disease’s case, the vWF Ag dosage tends to fluctuate, it can be normal, slightly decreased or increased. In our patient’s case it was slightly increased. This could be explained by the aortic stenosis which causes a blood flow decrease and damage of the vascular endothelium, triggering the release of vWF stored in the endothelial cells, resulting in an increase in vWF Ag levels within the blood flow. Besides, intestinal angiodysplasia, which is a common characteristic in Heyde syndrome, can cause a chronic gastrointestinal hemorrhage. This hemorrhage can lead to a compensatory response from the hemostatic system, including the release of vWF, which can also contribute to the increase on vWF Ag levels. It’s important to highlight that high levels of vWF Ag in Heyde syndrome tend to be the result of a physiological response to underlying conditions, meaning, aortic stenosis and intestinal angiodysplasia. However, interpreting these levels must be done with the complete clinical context of the patient and other pertinent diagnostic tests. The decisive analysis for the diagnosis is vWF multimer analysis through electrophoresis.
The most appropriate treatment is valve replacement. ⁴
Heyde syndrome is a rare pathology but an entity that we have to be aware of when it comes to evaluate a patient’s history of bleeding or anemia, especially when bleeding’s origin is not visible on the complementary studies. It’s indispensable for the adequate detection and interpretation of its manifestations and appropriate handling of the valve disease, in a multidisciplinary environment.
The most appropriate treatment is the resolution of the aortic valve obstruction. The valve replacement reverts the basic pathophysiological disorder, reversing the subsequential platelet disfunction and angiodysplasias’ bleeding coinciding or favored by the aortic stenosis itself.
REFERENCES
1. Heyde EC. Gastrointestinal bleeding in aortic stenosis. N Engl J Med. 1958;259:196. [ Links ]
2. Vaz A, Correia A, Martin B, Capelo J, Ferreira P, Henriques P, et al. Heyde Syndrome: The link between aortic stenosis and gastrointestinal bleeding. Rev Port Cardiol. 2010; 29(2): 309-14 [ Links ]
3. King RM, Pluth JR, Giuliani E.R. The association of unexplained gastrointestinal bleeding with calcific aortic stenosis. Ann Thorac Surg, 1987; 44: 514-516 [ Links ]
4. Garcia-Martin A, Moreno A, Moro C. Si´ndrome de Heyde. Rev Esp Cardiol. 2011; 64(1): 75-77. doi:10.1016/j.recesp.2010.06.005 [ Links ]
5. Warkentin TE, Moore JC, Morgan D.G. Aortic stenosis and bleeding gastrointestinal angiodysplasia: is acquired von Willebrand's disease. Lancet 1992; 340: 35-37 [ Links ]
6. Céspedes Rodríguez HA, Céspedes Rodríguez HR, Fernández Pérez R. Sindrome de Heyde. Rev. Cubana Cir. 2020 Sep;59(3): e908 Epub 10-Nov-2020. [ Links ]
7. Veyradier A, Balian A, Wolf M, Giraud V, Montembault S, Obert B, Dagher I, Chaput JC, Meyer D, Naveau S. Abnormal von Willebrand factor in bleeding angiodysplasias of the digestive tract. Gastroenterology. 2001 Feb; 120(2): 346-53. doi: 10.1053/gast.2001.21204. PMID: 11159874. [ Links ]
8. Hernández-Zamora E, Zavala-Hernández C, Quintana-González S, Reyes-Maldonado E. Enfermedad de von Willebrand, biología molecular y diagnóstico. Cir Cir. 2015 May-Jun; 83(3): 255-64. doi: 10.1016/j.circir.2015.05.010. Epub 2015 Jun 6. PMID: 26055290. [ Links ]
9. Vahanian A, Baumgartner H, Bax J, Butchart E, Dion R, Filippatos G, Flachskampf F, Hall R, Iung B, Kasprzak J, Nataf P, Tornos P, Torracca L, Wenink A; Task Force on the Management of Valvular Hearth Disease of the European Society of Cardiology; ESC Committee for Practice Guidelines. Guidelines on the management of valvular heart disease: The Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology. Eur Heart J. 2007 Jan;28(2):230-68. doi: 10.1093/eurheartj/ehl428. Epub 2007 Jan 26. PMID: 17259184. [ Links ]
Author data
6Dr. Víctor Raúl Luraschi Centurión (Luracho@gmail.com), Medical Director, Chief of General Surgery Services. Hospital General de Luque, General Surgery, Luque, Paraguay
7Dra. Rita Monthzerrat Miranda Vergara (brujichi@gmail.com), Chief of General Surgery Service Hall. Hospital General de Luque, General Surgery, Luque, Paraguay
17Dr. Roun Kim (rouni87@hotmail.com), General Surgeon. Hospital General de Luque, General Surgery, Luque, Paraguay
8Responsible editor: Helmut A. Segovia Lohse. https://orcid.org/0000-0003-3255-5345. Universidad Nacional de Asunción. Facultad de Ciencias Médicas. San Lorenzo, Paraguay. Ministerio de Salud Pública y Bienestar Social. Hospital General de Lambaré. Paraguay
ETHICAL CONSIDERATIONS
There were no identified ethical issues in the handling of the clinical case. Informed consent was obtained from the patient for the publishing of their medical history.
FUNDING
AUTHOR’S CONTRIBUTIONS
CONFLICT OF INTERESTS
Received: July 19, 2023; Accepted: April 16, 2024











 texto en
texto en 



