Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Cirugía paraguaya
versión On-line ISSN 2307-0420
Cir. parag. vol.48 no.1 Asunción abr. 2024
https://doi.org/10.18004/sopaci.2024.abril.21
Original Article
Experience in the treatment of complex perianal fistulas in a public hospital. 2018-2022
1Ministerio de Salud Pública y Bienestar Social. Centro Médico Nacional, Hospital Nacional. Departamento de Cirugía General, Servicio de Coloproctologìa. Itauguá, Paraguay.
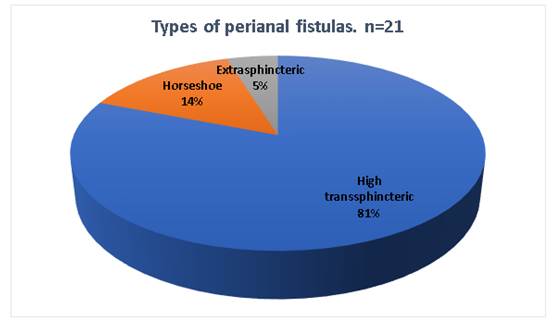
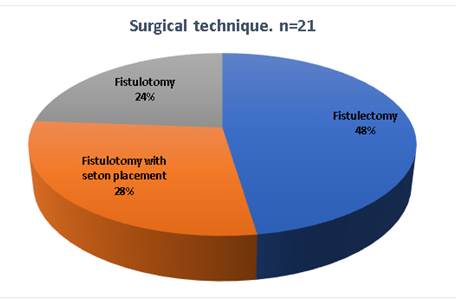
Introduction: Complex perianal fistula treatment is controversial; it requires a precise anatomical and auxiliary diagnosis methods’ knowledge to offer the best result possible for the patient. Objective: To describe the experience of complex perianal fistula treatment within the Public Hospital during the 2018 - 2022 period. Materials and Methods: Observational, descriptive, cross sectional, non-probabilistic study of consecutive patients with a complex perianal fistula diagnosis admitted to coloproctology services in the Itauguá National Hospital during the January 2018 - December 2022 period, of which 21 fit the complex perianal fistula criteria. Results: Of the 21 patients, 76% were male, with an average age of 35 ± 10 years old, the main consultation reason was anal secretion in 19 patients. Regarding the fistula type, an 81% high transsphincteric fistula was identified, as for the treatment, in 48% a fistulectomy was performed, and regarding complications, only 10% of patients suffered from fistula recurrence which was treated through a fistulectomy with seton placement. Conclusion: Complex perianal fistula is an infrequent periorificial pathology, the data obtained from physical examination and the possibility to effectuate complementary studies with advanced technological resources are fundamental to a satisfactory resolution.
Keywords: perianal fistula; complex fistula; fistulectomy; endorectal ultrasound; nuclear magnetic resonance
Introducción: El tratamiento de la fistula perianal compleja es controvertido, requiere de un conocimiento anatómico preciso y de métodos auxiliares de diagnóstico para ofrecer el mejor resultado posible al paciente. Objetivos: Describir la experiencia en el tratamiento de las Fístulas Perianales complejas en un Hospital Público en el periodo 2018 - 2022. Material y Métodos: Estudio observacional descriptivo de corte transversal, no probabilístico de casos consecutivos de pacientes con diagnóstico de fistula perianal compleja ingresados en el servicio de coloproctología del Hospital Nacional de Itauguá en el periodo de enero de 2018 hasta diciembre de 2022, de los cuales 21 cumplen con los criterios de inclusión de fistula perianal compleja. Resultados: De los 21 pacientes, 76% fueron hombres, con una media de edad de 35 años ± 10, el principal motivo de consulta fue secreción anal en 19 pacientes. En cuanto al tipo de fístula se identificó un 81% de fístula transesfinteriana alta, en cuanto al tratamiento, se realizó en un 48% fistulectomìas, en cuanto a las complicaciones, solo en un 10 % de los pacientes se constató recidiva de la fístula que fue tratada con fistulotomía con colocación sedal. Conclusión: La fístula perianal compleja es una patología periorificial poco frecuente, son fundamentales los datos obtenidos por el examen físico y la posibilidad de efectuar estudios complementarios con recursos tecnológicos avanzados para su resolución satisfactoria.
Palabras claves: fístula perianal; fístula compleja; fistulectomía; ecografía endorrectal; resonancia magnética nuclear
INTRODUCTION
Complex perianal fistula treatment is controversial; it requires a precise anatomical and auxiliary diagnosis methods’ knowledge to offer the best result possible for the patient. A complex fistula on the anus is difficult to diagnose and treat, requiring careful approaches due to the high risk of complications and recurrences1.
In over 90% of cases, fistulas are caused by a cryptoglandular-level infection, from there, it spreads from the intersphincteric space to perirectal anatomical spaces, allowing several morphological variables which define the complexity of this pathology. On the remaining 10% its origin can be secondary to Crohn’s disease, radiotherapy, tuberculosis, concussion, iatrogenic, among others. Not all perianal orifices correspond to perianal fistula. The tract between the intersphincteric space and external orifice normally defines the type of fistula. Its frequency is greater in men than in women1-2.
Regarding classification, Parks suggested a classification based on the relation between the fistula and external anal sphincter. Four types were described: Intersphincteric (the tract goes through only the internal sphincter, most common, represents around 60% of cases), Transsphincteric (the tract goes through both sphincters: constitutes around 25% of cases), Suprasphincteric (the tract goes above the external sphincter, in the puborectalis, representing less than 5%), Extrasphincteric (the tract goes outside the sphincters: does not origin within the crypt. Are caused by concussions, inflammatory bowel disease, or pelvic sepsis. Constitute less than 5% of cases)2.
Generally, anal fistulas are simple, which is to say, present an external orifice, evident internal orifice, and a unique, rectilinear, and low tract between the two. The surgical solution is easy and involves a complete plane laying, many times in ambulatory surgery regimen and with low anal incontinence risk. When the described situation varies, a complex anal fistula must be taken as a possibility. The complexity criteria are dictated by the fistula’s anatomical characteristics or by the surgical intervention’s complexity which is crucial to cure and preserve continence3). (see Table 1)
Table 1. Complex Fistula Characteristics
| Complex Fistula Characteristics |
|---|
| Suprasphincteric, high transsphincteric, and some middle transsphincteric fistulas. |
| Anterior face fistula on woman. |
| Extrasphincteric fistulas. |
| Secondary tract and intermediate cavity fistulas. |
| Relapsed fistulas. |
| Fistulas without internal orifice. |
| Horseshoe fistula. |
| Fistulas with several internal orifices or orifices situated on top of the pectineal line. |
| Rectovaginal fistulas, the ones after radiotherapy and patients with an inflammatory bowel disease (IBD), especially Crohn’s disease. |
DIAGNOSTIC
Diagnostic is based on anamnesis and physical exploration, occasionally including an anoscopy. A well-trained finger is still an exceptionally useful tool for the study of anal fistula. At first the external orifice is studied and additional orifices and debridement or previous intervention scars are investigated. Next, the subcutaneous induration which goes from the external orifice to the anus’ deepness, is palpated. This maneuver is not only useful for evaluating the tract’s direction, but it even helps to identify additional trajectories or indurations. Afterwards, a rectal feel to identify the internal orifice is performed. This is identified as a small protuberance or depression usually situated on the dented line in high correlation to the traditional Goodsall rule4.
Endoanal ultrasound with rotating sound is an exploration that offers high-definition real-time images, with focal distance of up to 6 cm across the entire rectum and anal canal’s perimeter, which allows the study of most fistulas. The oxygenated water instillation through the external orifice increases the precision to study the tract and localize the internal orifice. 5
MRIs also provides very exact information about the anal fistula’s morphology, especially when an endoanal coil is used. It’s a more sophisticated and costly exploration which requires adequate infrastructure and a radio-diagnostic specialist with deep knowledge in anorectal anatomy and data of interest for the surgeon. It’s very useful to value extrasphincteric plans, but more difficultly differentiates sphincteric muscles6.
Fistulography has been displaced by ultrasound and MRI. Most likely, its use must be restricted nowadays in cases in which these two explorations don’t contribute useful data. CT scans, especially with the introduction of fistulous orifice contrast, can complement fistulography indications7.
Surgical options for implementation include Fistulotomy (laid plan): consists of the full fistulous tract’s longitudinal opening. Usually associated with a marsupialization of the fistula’s edges, this procedure is used on simple fistulas, however, it can also be used in complex fistulas3.
Fistulectomy: it’s the extraction of the fistulous tract, a type of technique to preserve the sphincter, procedure which allows precise resection of the fistula’s tract, hence reducing the chance of losing a secondary tract8.
Advancement endorectal flap: Probably the most used method for high fistula treatment. Total or partial removal of the internal orifice and fistulous tract, a flap is designed which includes mucous and part of the internal anal sphincter’s fibers that displaces in craniocaudal-wise to completely cover the fistula’s previous orifice and creates a barrier against the rectum’s pressure, bringing healthy and vascularized tissue, which favors definitive cicatrization9.
Sealant or fibrin glue: This technique, described several years ago, consist of scraping and washing the fistulous tract with oxygenated water, and introducing a sound, a combination of fibrinogen and thrombin (fibrin), to seal the entire tract and favor its cicatrization. It’s indicated in fistulas which present only a single tract, without intermediate cavities nor infection, and well-defined internal and external orifices. Healing indexes are varied, ranging from 14 to 85%, taking into account what its failure does not prevent the use of any other posterior method9.
Collagen plug: consists of a porcine small intestine’s acellular derivative of extracellular matrix, which allows the inclusion and remodeling of scar tissue9.
The seton: the internal and external orifice are linked and knotted on the exterior, presenting several uses such as, cutting seton, which is progressively tightened until the sphincteric muscles are sectioned. Drainage seton, to trigger the formation of a fibrous tract when there’s an active fistula infection10.
LIFT (Ligation of the Intersphincteric Fistula Tract), consists of the fistulous tract’s ligation to the intersphincteric plan’s level, fully preserving the sphincters. It has a healing rate ranging from 68% to 83%, with an average healing time of 6 to 7 weeks11.
TROPIS (Transanal opening of intersphincteric space), like LIFT, where the fistula’s tract is linked and cut on the intersphincteric plan, while in TROPIS, the intersphincteric portion of the fistula is opened (the roof is removed) on the anal canal. The roof removal is done for the intersphincteric portion of the tract is completely drained12.
PERFACT (Proximal superficial cauterization, emptying regularly fistula tracts and curettage of tracts) is a useful method for complex anal fistulas, even in abscess-associated fistulas, supralevator fistulas and when the internal opening cannot be located. The PERFACT procedure involves two steps: superficial cauterization of the mucous in and around the internal opening and maintenance of all clean tracts13.
VAAFT: (Video-assisted anal fistula treatment), it’s a procedure in which a rigid endoscope is used, where curettage, fistulous tract cauterization and closure of internal orifice are performed, one of its limitations being that there must be an external orifice14.
The objective of the present work was to describe the experience in complex perianal fistula treatment in a Public Hospital within the 2018 - 2022 period. We consider the knowledge and handling of this pathology important, even if infrequent, as in untrained hands it has the potential to leave aftermaths such as incontinence and recurrence.
MATERIALS AND METHODS
An observational descriptive, cross sectional, non-probabilistic study of consecutive cases of patients with a complex perianal fistula diagnosis admitted to coloproctology services within the Itauguá National Hospital during the January 2018 through December 2022 period was performed. Inclusion criteria were as followed: adult patients of both sexes with complex perianal fistula diagnosis (according to Table 1) who have complete clinical files, of which 21 fulfill the complex perianal fistula inclusion criteria. The data was harvested into Excel spreadsheets. Confidentiality of individual data was kept, and the result exposition has been guaranteed to be collectively, or in the case that it’s shown individually the privacy of the patient is maintained. The limitations were the small size of the sample group, a few incomplete files, the handling criteria of the specialists involved in surgical procedures and finally, despite there being trained professionals in endorectal ultrasound, the cost isn’t accessible for all patients and the Itauguá National Hospital doesn’t provide said study nor nuclear magnetic resonance.
RESULTS
99 clinical backgrounds were revised from perianal fistula patients, who were admitted into coloproctology services, during the January 2018 through December 2022 period, of which 21 fulfill the complex perianal fistula criteria, which represents the 21.2% of the total clinical backgrounds revised. In the present revision, 16 patients were male (76%) and 5 were female (24%), 3:1 ratio.
The most frequent age range was between 31 to 40 years old. The main consultation reason was anal secretion in 19 patients and anal pain in 2 patients.
As for the fistula type, 17 patients (81%) presented high transsphincteric fistula, 3 patients (14%) horseshoe fistula, 1 patient (5%) extrasphincteric fistula (see Graphic 1).
Only in 6 patients a preoperatory colonoscopy was performed.
As for treatment, 10 fistulectomies (48%), 6 fistulotomy with seton placement (28%) were performed, and in 5 patients (24%) only a fistulotomy. All procedures were performed with spinal anesthesia.
In patients which the seton was left, the average adjustment period was 7 days and the seton fall time was 21 days. The average inpatient time was 3 days (67%) and 5 days (33%). Spinal anesthesia was performed on all patients. Sphincter preservation technique was not performed on any patients.
As for complications, only in 2 patients (10%) fistula recurrence was found, which was treated with seton placement fistulotomy, yielding proper evolution in both cases. Patient follow-up of up to 6 months after surgery was performed, observing only the aforementioned complications (2 recurrences).
Routine anal continence assessment nor incontinence grade scoring were performed on any patients during preoperatory nor postoperatory, continence evaluation was performed alongside interrogation and physical exam within checks up to 6 months after the surgical event, no patient reported gas nor feces incontinence. No mortality cases.
DISCUSSION
Perianal fistulas have been a common pathology, but problematic at the same time. Within the studied period regarding sex distribution, it was recorded that 16 patients were male and 5 were female, Carr and col. found an increase prevalence in men rather than women, with a rate of 12.3 cases for every 100.000 and 5,6 cases for every 100.000, respectively. These authors also found that the average age at the moment of diagnosis was of 38 years old, similar data to the present study15.
As for consultation reason, the most frequent one was anal secretion, followed up by anal pain, Machain and col. found that the most frequent symptoms were paint, pruritus and secretions. Of them pain represented the main motive of consultation with 41%; (n=46) followed by secretions with a 32% of the total (n=36). These authors also found, with relation to the most frequent fistulous tracts were the lower transsphincteric with 46.4% (n=52) and intersphincteric with 36.6% (n=41), followed by high transsphincteric with 11.6% (n=13), extrasphincteric and horseshoe were both found in 2.68% each (n=3). Unlike our series, in which 81% of patients presented high transsphincteric fistulas, 14% of patients presented horseshoe fistulas and 5% extrasphincteric fistulas16.
Regarding the surgical technique found in the present series, even though the literature is very clear in relation to complex fistulas, in which the sphincter preservation techniques are recommended (advance flap, LIFT, VAAFT, etc.), leaving fistulotomies and/or fistulectomies for simple fistulas, just as Charalampopoulos and col recommend, our series found that all cases were treated with fistulectomies (48%), fistulotomies with seton placement (28%) and only fistulotomy in (24%)17.
Subhas and col. in a revision of literature related to the use of setons in anal fistula treatment, found that the cutting seton falls after 30 days, with adjustments every 7 days, unlike our present series, in which it falls after 21 days, with a similar adjustment every 7 days18.
In another series Chuang y col., in a study about 112 patients with complex perianal fistula diagnosis, treated through setons, proved that the use of elastic band, adjusted at weekly intervals is safe and effective, with a shorter recovery time for the wound, lower recurrence and less continence disorders19.
CONCLUSION
As conclusion we can say that the complex fistula percentage was of 21.2%. The average age was 35 years old. As for gender the most prominent one was the male sex. The main consultation reason was anal secretion.
Regarding treatment, 10 fistulectomies, 6 fistulotomies with seton placement and in 5 patients only a fistulotomy was performed. Fistula recurrence was reported in 2 patients, which were treated with seton placement fistulotomy. In patients in which the seton was left, the average adjustment time was 7 days and the seton fall time was 21 days. The average inpatient time was 3 and 5 days.
Spinal anesthesia was performed on all patients. Sphincteric preservation techniques were not performed on any patients. No mortality was present in the series. Patient follow-up of up to 6 months was performed after the surgery.
REFERENCES
1. Cavero Ibiricu A, Simó Fernández V, Pastor Teso E, Arredondo Chaves J. Complex Perianal Fistula. Cir Esp (Engl Ed). 2018 Aug-Sep;96(7):452. English, Spanish. doi: 10.1016/j.ciresp.2017.12.010. Epub 2018 Feb 12. PMID: 29448985. [ Links ]
2. Parks A.G., Gordon P.H., Hardcastle J.D.: A classification of fistula-in-ano. Br J Surg 63. 1-12.1976. [ Links ]
3. Gaertner WB, Burgess PL, Davids JS, Lightner AL, Shogan BD, Sun MY, Steele SR, Paquette IM, Feingold DL; Clinical Practice Guidelines Committee of the American Society of Colon and Rectal Surgeons. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Management of Anorectal Abscess, Fistula-in-Ano, and Rectovaginal Fistula. Dis Colon Rectum. 2022 Aug 1; 65(8): 964-985. doi: 10.1097/DCR.0000000000002473. Epub 2022 Jul 5. PMID: 35732009. [ Links ]
4. Steele SR, Hull TL, Hyman N, Maykel JA, Read TE, Whitlow CB. The ASCRS textbook of colon and rectal surgery. 4th ed. 2022. [ Links ]
5. Jhaveri KS, Thipphavong S, Guo L, Harisinghani MG. MR Imaging of Perianal Fistulas. Radiol Clin North Am. 2018 Sep;56(5):775-789. doi: 10.1016/j.rcl.2018.04.005. Epub 2018 Jul 11. PMID: 30119773. [ Links ]
6. Teymouri A, Keshvari A, Ashjaei A, Ahmadi Tafti SM, Salahshour F, Khorasanizadeh F, Naseri A. Predictors of outcome in cryptoglandular anal fistula according to magnetic resonance imaging: A systematic review. Health Sci Rep. 2023 Jun 22;6(6): e1354. doi: 10.1002/hsr2.1354. PMID: 37359408; PMCID: PMC10286857. [ Links ]
7. Bhatt S, Jain BK, Singh VK. Multi Detector Computed Tomography Fistulography In Patients of Fistula-in-Ano: An Imaging Collage. Pol J Radiol. 2017 Sep 15; 82: 516-523. doi: 10.12659/PJR.901523. PMID: 29662582; PMCID: PMC5894016. [ Links ]
8. Lee KY, Lee J, Han EC, Kwon YH, Ryoo SB, Park KJ. Coring-out fistulectomy for perianal cryptoglandular fistula: a retrospective cohort study on 20 years of experience at a single center. Ann Surg Treat Res. 2022 Mar; 102(3): 167-175. doi: 10.4174/astr.2022.102.3.167. Epub 2022 Mar 4. PMID: 35317352; PMCID: PMC8914524. [ Links ]
9. Amato A, Bottini C, De Nardi P, Giamundo P, Lauretta A, Realis Luc A, Piloni V. Evaluation and management of perianal abscess and anal fistula: SICCR position statement. Tech Coloproctol. 2020 Feb; 24(2): 127-143. doi: 10.1007/s10151-019-02144-1. Epub 2020 Jan 23. PMID: 31974827. [ Links ]
10. Durgun C, Tüzün A. The use of a loose seton as a definitive surgical treatment for anorectal abscesses and complex anal fistulas. Adv Clin Exp Med. 2023 Oct; 32(10): 1149-1157. doi: 10.17219/acem/161162. PMID: 36920266. [ Links ]
11. Charalampopoulos A, Papakonstantinou D, Bagias G, Nastos K, Perdikaris M, Papagrigoriadis S. Surgery of Simple and Complex Anal Fistulae in Adults: A Review of the Literature for Optimal Surgical Outcomes. Cureus. 2023 Mar 8;15(3): e35888. doi: 10.7759/cureus.35888. PMID: 36911578; PMCID: PMC9993441. [ Links ]
12. Garg P, Mongia A. Transanal opening of the intersphincteric space (TROPIS): a novel procedure on the horizon to effectively manage high complex anal fistulas. Ann Coloproctol. 2024 Feb;40(1):74-81. doi: 10.3393/ac.2022.01263.0180. Epub 2023 Oct 24. PMID: 38414123; PMCID: PMC10915533. [ Links ]
13. Garg P, Garg M. PERFACT procedure: a new concept to treat highly complex anal fistula. World J Gastroenterol. 2015 Apr 7;21(13):4020-9. doi: 10.3748/wjg.v21.i13.4020. PMID: 25852290; PMCID: PMC4385552. [ Links ]
14. Tian Z, Li YL, Nan SJ, Xiu WC, Wang YQ. Video-assisted anal fistula treatment for complex anorectal fistulas in adults: a systematic review and meta-analysis. Tech Coloproctol. 2022 Oct; 26(10): 783-795. doi: 10.1007/s10151-022-02614-z. Epub 2022 Mar 28. PMID: 35347492. [ Links ]
15. Carr S, Velasco AL. Fistula-in-Ano. 2023 Jul 31. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. PMID: 32491449. [ Links ]
16. Machaín GM, Domínguez R, Sosa I, Nayar GD, Páez LI. Recidiva de fístulas perianales post quirúrgicas en la Segunda Cátedra de Clínica Quirúrgica, Hospital de Clínicas, San Lorenzo año 2008-2019. An. Fac. Cienc. Méd. (Asunción) [Internet]. 2021 Aug [cited 2024 Mar 28]; 54(2): 97-102. Available from: http://scielo.iics.una.py/scielo.php?script=sci_arttext&pid=S181689492021000200097&lng=en. https://doi.org/10.18004/anales/2021.054.02.97 [ Links ]
17. Charalampopoulos A, Papakonstantinou D, Bagias G, Nastos K, Perdikaris M, Papagrigoriadis S. Surgery of Simple and Complex Anal Fistulae in Adults: A Review of the Literature for Optimal Surgical Outcomes. Cureus. 2023 Mar 8;15(3): e35888. doi: 10.7759/cureus.35888. PMID: 36911578; PMCID: PMC9993441. [ Links ]
18. Subhas G, Singh Bhullar J, Al-Omari A, Unawane A, Mittal VK, Pearlman R. Setons in the treatment of anal fistula: review of variations in materials and techniques. Dig Surg. 2012;29(4):292-300. doi: 10.1159/000342398. Epub 2012 Aug 31. PMID: 22948115. [ Links ]
19. Chuang-Wei C, Chang-Chieh W, Cheng-Wen H, Tsai-Yu L, Chun-Che F, Shu-Wen J. Cutting seton for complex anal fistulas. Surgeon. 2008;6(3):185-188. doi: 10.1016/S1479- [ Links ]
Conflict of interest
Author declares no conflict of interests and respects ethical conducts and proper publication practices.
Author’s contribution
Author participated in the creation and design of the work; bibliographic search, data recollection, writing and critical revision in search of important intellectual content, critical revision, and final approval; and agrees to the responsibility of all aspects of the work to guarantee that matters related to the precision or integrity of any part of the work is researched and resolved adequately.
Ethical considerations
Confidentiality of individual data was kept and has been guaranteed that the results will be exposed collectively, or in case of being individual maintaining said privacy.
Funding
Received: October 25, 2023; Accepted: April 15, 2024











 texto en
texto en