Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Cirugía paraguaya
versión On-line ISSN 2307-0420
Cir. parag. vol.48 no.1 Asunción abr. 2024
https://doi.org/10.18004/sopaci.2024.abril.12
Original Article
Comparison of characteristics and morbility in colorectal oncological surgeries with primary anastomosis in elderly patients according to the approach route
1Hospital Central del Instituto de Previsión Social. Asunción, Paraguay
Introduction: Colorectal cancer is common and has more morbimortality in the elderly. Laparoscopic surgery is used to treat it, showing benefits such as less bleeding and hospitalization time. Despite their vulnerability, the elderly can be benefited from minimally invasive surgeries. Materials and Methods: Observational, descriptive, and retrospective study to compare the characteristics and morbimortality of colorectal surgeries with programmed primary anastomosis according to the handling way in 65-year-old or older patients in the General Surgery Services of the Institute of Social Prevision’s General Hospital between December 2019 and August 2020. Results: Of the 26 patients, 30.7% was submitted to laparoscopic surgery and 69.2% to conventional surgery. Most of them were right colectomies. The anastomotic configuration did not significantly differ. Stapler use was 87.5% in laparoscopic surgery and 55.6% in conventional. There were anastomosis leaks in both groups (27.8% in conventional). Complications were classified according to Clavien-Dindo observing that more than a third were type 1 and 2. Conclusions: Most patients were operated by conventional surgery. Right colectomy was the most performed procedure, and the anastomosis leak was observed in both groups, although with a higher conventional surgery rate. Most complications were mild. More studies with bigger samples are required to evaluate the relationship between surgical technique, surgeon’s experience, and morbimortality.
Key words: Colorectal surgery; colorectal cancer; postoperative complications
Introducción: El cáncer colorrectal es común y tiene mayor morbimortalidad en los ancianos. La cirugía laparoscópica se usa para tratarlo, mostrando beneficios como menor sangrado y tiempo de hospitalización. A pesar de su vulnerabilidad, los ancianos pueden beneficiarse de técnicas mínimamente invasivas. Materiales y Métodos: Estudio observacional, descriptivo y retrospectivo para comparar las características y morbimortalidad de cirugías colorrectales con anastomosis primaria programada según la vía de abordaje en pacientes de 65 años o más en el Servicio de Cirugía General del Hospital Central del Instituto de Previsión Social entre diciembre 2019 y agosto 2020. Resultados: De los 26 pacientes, el 30,7% se sometió a cirugía laparoscópica y el 69,2% a cirugía convencional. La mayoría fueron colectomías derechas. La configuración anastomótica no difirió significativamente. El uso de grapadora fue de 87,5% en cirugía laparoscópica y 55,6% en convencional. Hubo fugas de anastomosis en ambos grupos (27,8% en convencional). Las complicaciones se clasificaron según Clavien-Dindo observándose que más de los 2/3 fueron tipo 1 y 2. Conclusiones: La mayoría de los pacientes fue operado por cirugía convencional. La colectomía derecha fue el procedimiento más realizado y la fuga de anastomosis se observó en ambos grupos, aunque con una tasa mayor en cirugía convencional. La mayoría de las complicaciones fueron leves. Se requieren más estudios con mayor muestra para evaluar relación entre técnica quirúrgica, experiencia del cirujano y morbimortalidad.
Palabras clave: Cirugía colorrectal; cáncer colorrectal; complicaciones postoperatorias
INTRODUCTION
Colorectal resections can be performed through malignant or benign pathologies, with anastomosis or ostomy confection. The anastomosis types include the term-terminal, term-lateral, or lateral-lateral type, with mechanical (staple) or manual suture. The surgical options include ileus-colic resection, right, transverse, or left colectomies, sigmoidectomy, and protocolectomy, among others. Conventional or minimally invasive handlings can be used, and in the latter group the manually or robotically assisted laparoscopic handling are included1.
The colorectal carcinoma is the most common neoplasia of the digestive tube, and its treatment has surgical, curative or palliative indication, even with the existence of metastasis2), because it decreases the tumoral load and prevents possible complications3). Among the most important risk factors ageing is included, given that 90% of patients who suffer from it are older than 50 years old, however, it’s also prevalent in patients younger than 50 years old hence a colonoscopy is key for diagnosing4). The surgery’s individualization in elderly patients looks to reduce complications. Minimally invasive surgery, even ambulatory, is studied for better results5). Postsurgical complications can be evaluated according to the Clavien-Dindo classification6.
In the present article, morbidity and colorectal surgeries with primary anastomosis’ characteristics were compared in patients older than 65 years old, according to the handling way, in the Institute of Social Prevision’s Central Hospital (December 2019 - August 2020).
MATERIALS Y METHODS
An observational, descriptive, and retrospective study was performed. The data was collected through the selection of clinical files and procurement of a database. The inclusion criteria were colorectal cancer patients of 65 or more years of age, submitted to colorectal surgery with programmed primary anastomosis, admitted to General Surgery Services of the Institute of Social Prevision’s Central Hospital, during the December 2019 to August 2020 period. Among the exclusion criteria are patients whose initial surgery was performed in a different facility and patients with an incomplete clinical history or medical file.
The surgical handling method was determined and compared to the anastomosis’ configuration, technique, drainage utilization, morbimortality according to the Clavien-Dindo classification, anastomosis leak and inpatient stay. Once the information was compiled, a database processed through an Excel® sheet was designed.
RESULTS
26 patients of 65 years old or older submitted to colorectal surgeries with primary anastomosis were evaluated, of which 30.7% were performed by laparoscopic way, and 69.2% by conventional way.
Base pathologies were found present on all patients operated through laparoscopic way (8/8), and in 72.2% (13/18) of those operated by conventional way.
Within the group submitted to laparoscopic-way surgery, 62.5% were right colectomies, 25% left colectomies, and 12.5% sigmoidectomies. As for the group submitted to conventional-way surgery, 61.1% were right colectomies, 16.6% sigmoidectomies, 11.1% lower anterior resections, 5.5% left colectomies, and 5.5% transversectomies.
Anastomotic configuration in the group submitted to laparoscopic-way surgery was 37.5% term-terminal, 37.5% lateral-lateral, and 25% term-lateral. Through conventional way 38.8% were lateral-lateral, 33.3% were term-lateral, and 27.7% were term-terminal. Manual suturing was used in 12.5% of laparoscopic approaches and in 44.4% of conventional-way approaches. Mechanical suturing was used in 87.5% of laparoscopic approaches and in 55.5% of conventional approaches. (see Table 1)
Regarding anastomosis’ complications, 12.5% presented anastomosis leak through laparoscopic way and 27.7% through conventional way. 87.5% of patients operated through laparoscopic way had a tubular drainage placement, and 88.8% through conventional way did so as well. (see Table 1)
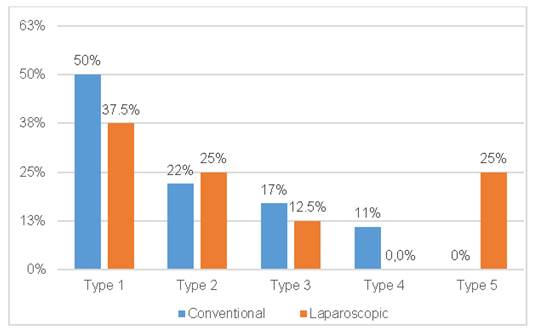
According to the Clavien-Dindo classification, the most frequent complication amongst both groups was type 1. (see Table 1, Graphic 1)
Tabla 1. Characteristics of patients over 65 years of age with colorectal surgery and primary anastomosis.
| Conventional (open) | Laparoscopic | ji2 | p value | |||||
| n | % | n | % | |||||
| Anastomosis configuration | Termino-terminal | 5 | 27.8 | 3 | 37.5 | |||
| Termino-lateral | 6 | 33.3 | 2 | 25.0 | 0.2979 | 0.8616 | ||
| Latero-lateral | 7 | 38.9 | 3 | 37.5 | ||||
| Anastomosis technique | Mechanical | 10 | 55.6 | 7 | 87.5 | 2.4971 | 0.1141 | |
| Manual | 8 | 44.4 | 1 | 12.5 | ||||
| Dreainage | With drainage | 16 | 88.9 | 7 | 87.5 | 0.0105 | 0.9185 | |
| Without drainage | 2 | 11.1 | 1 | 12.5 | ||||
| Complication (Clavien-DIndo) | Type 1 | 9 | 50.0 | 3 | 37.5 | __ | __ | |
| Type 2 | 4 | 22.2 | 2 | 25.0 | ||||
| Type 3 | 3 | 16.7 | 1 | 12.5 | ||||
| Type 4 | 2 | 11.1 | 0 | 0.0 | ||||
| Type 5 | 0 | 0.0 | 2 | 25.0 | ||||
| Anastomosis leakage | Present | 5 | 27.8 | 1 | 12.5 | 0.7282 | 0.3935 | |
| Absent | 13 | 72.2 | 7 | 87.5 | ||||
The average inpatient stay of patients operated through laparoscopic way was 6.75 days, and 9.2 days through conventional way.
DISCUSSION
A revision of 26 colorectal cancer patients who were submitted to colorectal surgeries with primary anastomosis was performed. The most common surgical approach was conventional-way and although it was the most frequent, laparoscopic-way has been the protagonist in our hospital center. In our current day, the laparoscopic way has become the standard method for colon surgeries7), the use of laparoscopic surgery on geriatric patients with colorectal cancer should increase due to the better long-term results8.
No significative difference between the different anastomosis configurations was observed, noting a similar frequency among term-terminal, lateral-lateral, and term-lateral anastomosis for both approach ways. This is also subjected to the patient’s localization and anatomy, the ileocolic anastomosis configuration’s impact that might have in the intestinal transit’s restitution after a right hemicolectomy. It’s necessary to perform a randomized essay comparing isoperistaltic and antiperistaltic modalities9), ileocolic, isoperistaltic, and antiperistaltic presented similar results in terms of performance, security, and functionality10.
Regarding the anastomosis technique, the use of mechanical stapler for anastomosis was predominant in both groups. It’s worth mentioning that the use of stapler with manual suture backup after the rectum cancer’s laparoscopic radical resection is convenient and effective11, making the standardized use of laparoscopic way and stapler for rectum cancer evident. A group of collaborators from the European Coloproctology Society informed increased use of the stapler technique rather than the manual one, alike our study, however, the most used surgical approach was laparoscopic way, which does not match the data of our study12.
Anastomosis leak was mostly present with conventional way and in an increased rate. Luglio and Corcione informed lesser anastomosis leak with the stapler’s use, however, they did not report the surgical approach way and specifically studied ileocolonic anastomosis13. Nordholom et al however reports a times two risk of anastomosis leak with the stapler’s use for ileocolic anastomosis, although it does not specify the surgical approach14. The collaborators’ group from the European Coloproctology Society studied the predictive factors of anastomosis leak in right colon cancer, where the surgery’s duration, conventional approach and stapler’s use was associated with a higher risk of anastomosis leakage12. There are studies that report that anastomosis leak us related to the deteriorated general survival and high local recurrency15,16.
In our study, abdominal drainage was left in almost every case, regardless of surgical approach. Some authors are not in favor of the rutinary use of drainages after colon and rectal anastomosis, voicing that it’s associated with an increase in injury’s infection rate which can be up to a 25%17.
For the morbimortality assessment the Clavien-Dindo classification was used. We observed that the most frequent complication was type 1, for laparoscopic approach as much as for conventional, although no type 5 complications were observed for the conventional-way submitted group, which were present in 25% of the laparoscopic-way submitted patients. The fact that most patients presented type 1 complications is encouraging given that studies report that the complications’ gravity is related to the general survivability18,19.
The shorter inpatient stay was for laparoscopic way, which matches with other studies with similar results20.
This article may be biased due to the low quantity of studied patients and the fact that the study was performed in a specialized hospital.
CONCLUSION
Of the patient total (26), most (69.2%) was submitted to conventional surgery. The most common resection type was right colectomy. Anastomosis configuration and the use of stapler did not show variations amongst the conventional and laparoscopic surgery groups. Anastomosis leaks were registered in both groups, with a higher rate in the conventional surgery group (27.7%). Complications are categorized according to the Clavien-Dindo classification, without significant discrepancies.
REFERENCES
1. Brunicardi FC, Andersen DK, Billiar TR, Dunn DL, Hunter JG, editores. Schwartz's principles of surgery. Tenth edition. New York: McGraw-Hill Education; 2014. [ Links ]
2. Buisman FE, Galjart B, Buettner S, Groot Koerkamp B, Grünhagen DJ, Verhoef C. Primary tumor location and the prognosis of patients after local treatment of colorectal liver metastases: a systematic review and meta-analysis. HPB. 2020; 22(3): 351-7. [ Links ]
3. Wang X-Y, Zhang R, Wang Z, Geng Y, Lin J, Ma K, et al. Meta-analysis of the association between primary tumour location and prognosis after surgical resection of colorectal liver metastases. Br J Surg. 2019; 106(13): 1747-60. [ Links ]
4. Millan M, Renau-Escrig AI. Minimizing the impact of colorectal surgery in the older patient: The role of enhanced recovery programs in older patients. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol. 2020; 46(3): 338-43. [ Links ]
5. Price BA, Bednarski BK, You YN, Manandhar M, Dean EM, Alawadi ZM, et al. Accelerated enhanced Recovery following Minimally Invasive colorectal cancer surgery (RecoverMI): a study protocol for a novel randomised controlled trial. BMJ Open. 20 de julio de 2017; 7(7): e015960. [ Links ]
6. Mitropoulos D, Artibani W, Biyani CS, Bjerggaard Jensen J, Rouprêt M, Truss M. Validation of the Clavien-Dindo Grading System in Urology by the European Association of Urology Guidelines Ad Hoc Panel. Eur Urol Focus. 2018; 4(4): 608-13. [ Links ]
7. Zhu D, Xu J. [Application of enhanced recovery after surgery in minimally invasive colorectal surgery]. Zhonghua Wei Chang Wai Ke Za Zhi Chin J Gastrointest Surg. marzo de 2016; 19(3): 256-9. [ Links ]
8. Fugang W, Zhaopeng Y, Meng Z, Maomin S. Long-term outcomes of laparoscopy vs. open surgery for colorectal cancer in elderly patients: A meta-analysis. Mol Clin Oncol. noviembre de 2017; 7(5): 771-6. [ Links ]
9. Ibañez N, Abrisqueta J, Luján J, Hernández Q, Parrilla P. Isoperistaltic versus antiperistaltic side-to-side anastomosis after right laparoscopic hemicolectomy for cancer (ISOVANTI) trial: study protocol for a randomised clinical trial. Int J Colorectal Dis. septiembre de 2017; 32(9): 1349-56. [ Links ]
10. Ibáñez N, Abrisqueta J, Luján J, Hernández Q, Rufete MD, Parrilla P. Isoperistaltic versus antiperistaltic ileocolic anastomosis. Does it really matter? Results from a randomised clinical trial (ISOVANTI). Surg Endosc. 2019; 33(9): 2850-7. [ Links ]
11. He Y, Zhu Z, Liu S, Liu L, Hu B, Wan X, et al. [Effect of anastomotic reinforcing sutures on the incidence of anastomotic leakage after laparoscopic radical resection of rectal cancer: a prospective randomized controlled trial]. Zhonghua Wei Chang Wai Ke Za Zhi ChinJ Gastrointest Surg . Apirl de 2018; 21(4): 431-6. [ Links ]
12. 2015 European Society of Coloproctology Collaborating Group. Predictors for Anastomotic Leak, Postoperative Complications, and Mortality After Right Colectomy for Cancer: Results From an International Snapshot Audit. Dis Colon Rectum. 2020; 63(5) :606-18. [ Links ]
13. Luglio G, Corcione F. Stapled versus handsewn methods for ileocolic anastomoses. Tech Coloproctology. noviembre de 2019; 23 (11): 1093-5. [ Links ]
14. A N-C, M SR, Pm K. Increased Leak Rates Following Stapled Versus Handsewn Ileocolic Anastomosis in Patients with Right-Sided Colon Cancer: A Nationwide Cohort Study [Internet]. Vol. 62, Diseases of the colon and rectum. Dis Colon Rectum; 2019 [citado 16 de noviembre de 2020]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/30489322/ [ Links ]
15. Bashir Mohamed K, Hansen CH, Krarup P-M, Fransgård T, Madsen MT, Gögenur I. The impact of anastomotic leakage on recurrence and long-term survival in patients with colonic cancer: A systematic review and meta-analysis. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol. 2020; 46(3): 439-47. [ Links ]
16. Wang S, Liu J, Wang S, Zhao H, Ge S, Wang W. Adverse Effects of Anastomotic Leakage on Local Recurrence and Survival After Curative Anterior Resection for Rectal Cancer: A Systematic Review and Meta-analysis. World J Surg. enero de 2017; 41(1): 277-84. [ Links ]
17. Podda M, Di Saverio S, Davies RJ, Atzeni J, Balestra F, Virdis F, et al. Prophylactic intra-abdominal drainage following colorectal anastomoses. A systematic review and meta-analysis of randomized controlled trials. Am J Surg. 2020; 219 (1): 164-74. [ Links ]
18. McSorley ST, Horgan PG, McMillan DC. The impact of the type and severity of postoperative complications on long-term outcomes following surgery for colorectal cancer: A systematic review and meta-analysis. Crit Rev Oncol Hematol. enero de 2016; 97: 168-77. [ Links ]
19. Lawler J, Choynowski M, Bailey K, Bucholc M, Johnston A, Sugrue M. Meta-analysis of the impact of postoperative infective complications on oncological outcomes in colorectal cancer surgery. BJS Open. 11 de junio de 2020. [ Links ]
20. Tan SJ, Jiang Y, Xi QL, Meng QY, Zhuang QL, Han YS, et al. [Meta-analysis of laparoscopic versus open surgery for palliative resection of the primary tumor in stage IV colorectal cancer]. Zhonghua Wei Chang Wai Ke Za Zhi Chin J Gastrointest Surg . 25 de junio de 2020;23 (6): 589-96. [ Links ]
Author data
Michelle Natascha Feltes Escurra. General Surgery Resident. Columbia University. Harlem Hospital Center, New York, USA.
Giulianna Benedetti. Health Sciences Faculty Intern. Universidad Católica Nuestra Señora de la Asunción. Asunción, Paraguay
Conflict of Interest
Author’s contribution
Dr. Pablo Schaerer, Dr. Marcelo Samudio, Dr. Michelle Feltes, Dr. Mónica Martínez, Dr. Monserrat Riquelme, Dr. Gabriela Sanabria, and Resident Giulianna Benedetti conceived the idea, elaborated the manuscript, bibliographic research, and final revision.
Ethical considerations
All principles of bioethics were upheld. Confidentiality of the results was kept under the use of a numeric code that identified each file, data only being known by the authors.
Funding
Received: September 25, 2023; Accepted: March 15, 2024











 texto en
texto en