Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Cirugía paraguaya
versión On-line ISSN 2307-0420
Cir. parag. vol.48 no.1 Asunción abr. 2024
https://doi.org/10.18004/sopaci.2024.abril.9
Original Article
Video-assisted retroperitoneal necrosectomy on acute pancreatitis. Itauguá National Hospital, period 2015-2021
1Ministerio de Salud Pública y Bienestar Social, Centro Médico Nacional, Hospital Nacional. Departamento de Cirugía General. Servicio de Cirugía General. Itauguá, Paraguay
INTRODUCTION: Acute pancreatitis on its necrotic form presents an estimated mortality of 50% in cases with surgery and up to 100% without surgery. MATERIALS: Observational, descriptive, retrospective, transversal study of patients with a complicated acute pancreatitis diagnosis who had a video-assisted necrosectomy performed through retroperitoneal approach on the Itauguá National Hospital, years 2015 to 2021. RESULTS: 35 patients with an average age of 57 years old, 60% were women, 57.1% were admitted with a severe pancreatitis diagnosis, and 42.9% with moderated pancreatitis. The percutaneous drainage was placed first in 29 cases, the patients were directly intervened with a video-assisted necrosectomy in 6 cases. The time between performing the draining and the debridement was 65.5% between the first and third subsequent week. Two thirds of the patients needed an additional surgical procedure, such as a second video-assisted debridement, cholecystectomy or open necrosectomy. A mortality of 11.4% was observed. CONCLUSION: Necrotizing pancreatitis’ treatment has now averted from open surgical debridement to a more conservative treatment and minimally invasive approaches. The video-assisted retroperitoneal debridement yielded relatively good results as a previous step to open surgery, hence avoiding complications befitting of a laparotomy.
Key words: acute pancreatitis; retroperitoneal debridement; necrosectomy.
INTRODUCCION: La pancreatitis aguda en su forma necrótica presenta una mortalidad estimada en 50% de los casos con cirugía y hasta 100% sin cirugía. MATERIALES: Estudio observacional, descriptivo, retrospectivo, transversal de pacientes con diagnóstico de pancreatitis aguda complicada en quienes se realizó necrosectomía videoasistida por vía retroperitoneal en el Hospital Nacional de Itauguá, periodo 2015 a 2021. RESULTADOS: 35 pacientes con una edad promedio e de 57 años, 60% fueron mujeres, 57,1% fue admitido con el diagnóstico de pancreatitis grave y 42,9% pancreatitis moderada. En 29 casos se realizó la colocación de drenaje percutáneo en primer lugar, en 6 casos los pacientes fueron intervenidos directamente con necrosectomía videoasistida. El tiempo entre la realización del drenaje y el debridamiento fue 65,5% entre la primera y tercera semana posterior. Dos tercios de los pacienter necesitaron un procedimiento quirúrgico adicional, como un segundo debridamiento videoasistido, colecistectomía o necrosectomía abierta. Se observó una mortalidad de 11,4%. CONCLUSION: El tratamiento de la pancreatitis necrotizante se ha alejado ahora del desbridamiento quirúrgico abierto a un tratamiento más conservador y enfoques mínimamente invasivos. El debridamiento retroperitoneal videoasistido arrojo relativos buenos resultados como escalón previo a la cirugía abierta, evitando así las complicaciones propias de una laparotomía.
Palabras claves: Pancreatitis aguda; debridamiento retroperitoneal; necrosectomía
INTRODUCTION
One of the most frequent pancreatic diseases in the world is acute pancreatitis (AP). It has an incidence from 5 to 80 cases for every 100,000 people, which variates according to different geographical regions, depending on alcohol consumption and the prevalence of gallstones1). AP is characterized by the activation of pancreatic enzymes and release of cytokines. The 20% of them evolves to become more severe, bringing forth complications such as pancreatic necrosis and sepsis, and finally multi-organ failure2.
Currently, the necrosis-infected AP is handled in a minimally invasive manner through the “step-up approach”. This methodology consists in the percutaneous or endoscopic drainage with antibiotics, followed by retroperitoneal debridement in case of the former’s failure, leaving open surgical drainage as the last resort3.
In AP, the main cause of death is infection of the necrotic tissue, which is associated with an improper diagnosis: mortality is approximately up 30 to 39% in those with infected necrosis (which occurs at some point during the clinical process in approximately a third of the necrosis patients). An intervention in the case of an infected pancreatic necrosis is generally required and, with less frequency, in patients with sterile necrosis that are symptomatic (especially in the case of biliary obstruction or gastric or duodenal outlet). Additional treatment has been open surgical necrosectomy: provides ample access to the infected necrosis, but it’s highly invasive and associated with reported morbidity rates of 34% to 95% and mortality rate of 11% to 39%, due to the physiological stress of the laparotomic debridement4.
The present study is dedicated to evaluating the characteristics of the procedure known as VARD (video-assisted retroperitoneal debridement) on the Itauguá National Hospital during the years 2015 to 2021.
MATERIALS AND METHODS
An observational, descriptive, retrospective, crosscut study was performed.
The sample were patients with a complicated AP diagnosis with infected necrosis intervened through VARD in the Itauguá National Hospital during the years 2015 to 2021.
As for the inclusion criteria, patients intervened through the VARD technique, that have had or not a previous drainage (percutaneous or endoscopic) were selected. As for exclusion criteria, patients intervened through other methods were not selected.
For the case selection, the surgical procedures’ register book of the General Surgery Services was accessed, to classify the AP patients on which VARD was performed, requesting clinical files to the Itauguá National Hospital’s statistical service afterwards for the recollection of variables of interest.
RESULTS
35 AP and infected necrosis patients were included, on which a VARD was performed. The average age was 57 years old, with a minimal age of 24 and a maximum of 78 years old. The 60% were of the feminine sex, while the 40% were masculine.
Regarding comorbidities, 77.1% reported high blood pressure, 45% obesity and Mellitus diabetes (see Table 1).
Table 1. Acute pancreatitis patients’ comorbidities intervened through VARD.
| Comorbidity | n | % |
|---|---|---|
| HBP | 27 | 77.1% |
| Obesity | 16 | 45.7% |
| Mellitus diabetes | 16 | 45.7% |
| COPD | 4 | 11.4% |
| CKD | 1 | 2.8% |
*VARD: video-assisted retroperitoneal debridement; HBP: high blood pressure; COPD: chronic obstructive pulmonary disease; CRK: chronic kidney disease
Regarding the admission diagnosis, 57.1% were severe AP and 42.9% moderate AP. As for etiology, 31 patients were of lithiasis cause, 2 alcoholic, and 2 hyperlipidemic.
Of the cited 35 patients on which a VARD was performed, 29 of them (82.9%) followed a “step-up approach” scheme with first a percutaneous drainage placement, and in 6 cases (17.1%) the patients were directly intervened through VARD (see Graphic 1).
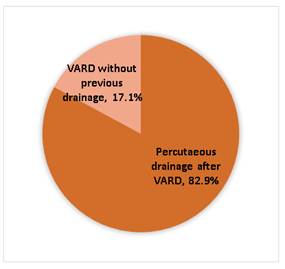
Graphic 1. Handling considering the “step-up approach” on patients with complicated acute pancreatitis with pancreatic necrosis. n=35. Itauguá National Hospital.
Time within the drainage’s placement and the VARD’s execution was 65.5% between the first and third post drainage weeks, 27.5% between the fourth and sixth weeks, and 7% between the seventh and nine weeks. (see Table 2).
Table 2. Time between the percutaneous drainage’s placement and the VARD’s execution.
| Time between percutaneous drainage and VARD | n | % |
|---|---|---|
| 1 to 3 weeks | 19 | 65.5% |
| 4 to 6 weeks | 8 | 27.5% |
| 7 to 9 weeks | 2 | 7.0% |
| Total | 29 | 100% |
After the first intervention through VARD, another surgical intervention was performed on 24 of the 35 patients (68.6%): second VARD on 12 patients (50%), cholecystectomy on 7 (29.1%), and open necrosectomy on 5 (20.8%) (see Table 3).
DISCUSSION
AP yet constitutes a severe problem for current-day surgery, despite registered advances in its proper clinical identification, causes, production mechanisms, imagery diagnosis elements, and treatment guidelines. According to statistics, 80% of the total patients will present a tame form of the disease, associated to an interstitial edematous pancreatic tissue or around the gland, and generally resolved in a week of medical treatment. However, the necrotizing variant of the condition, present on the resulting 20%, constitutes the most severe outcome, being characterized by pancreatic or peri-pancreatic necrosis, and becoming infected in a third of the cases, associating as well to sepsis statuses, severe sepsis, or simple or multiple organ failure, assessing an estimated mortality of 50% of the operated patient total and almost 100% of the non-operated ones5.
On the Itauguá National Hospital between January 2015 and November 2021, 35 patients with infected necrosis AP were intervened through the VARD technique. The average age was 57 years old, with a female predominance of 60%. These findings coincide with the study performed by Bang et al. where a female predominance of 75% was found. The cited study reports an age predominance between 18 to 35 years old reaching the 50%. This age range differs from the range found in our study, in which the patients presented an older age average6.
This study is based on patients who received VARD as treatment. The van Santvoort at al. study of the year 2010 showed that close to 35% of “step-up approach” patients did not require a subsequent necrosectomy7. The minimally invasive handling looks to reduce the surgical stress and associated complications to conventional interventions. Video-assisted handling of pancreatic necrosis improved the morbidity rates of patients submitted to surgical necrosectomy8.
It is crucial to find a proper window for performing a VARD. The point of entry must be comfortable for the patient, the trajectory must be as direct as possible and not compromise any organs or vital structures9.
Open necrosectomy is associated to a high mortality (approx. 40%) and morbidity (more than 95%) including bleeding, gastrointestinal fistulas, and pancreatic insufficiency. In the Wrońsky et al. study, the “step-up approach”, including the VARD was the superior approach in terms of results when compared to open necrosectomy. The number of patients with complications was significantly greater in patients submitted to a laparotomy compared to those who received VARD10.
The dilemma with the percutaneous approach is to define the moment in which the method fails and if the patient requires a necrosectomy, whether video-assisted or through conventional surgery. Early surgery, without a doubt has a higher morbimortality, but a great delay in the surgical indication is also accompanied by an important mortality. Exclusive percutaneous drainage treatment doesn’t always achieve a sepsis control on these patients, making the video-assisted surgical handling through retroperitoneal way necessary11.
CONCLUSION
The average age of AP patients in this work was 57 years old, predominately of the female sex. In 88.5% of cases the etiology was lithiasic.
In this study, 82.9% of patients followed the “step-up approach” scheme, percutaneous drainage and then VARD. Inn 17.1% a VARD was performed as a first procedure. The time between the percutaneous drainage’ performance and the VARD’s was of 1-3 weeks (65.5%).
Approximately two thirds of the patients (68.6%) submitted to VARD required an additional surgical procedure: 50% of patients needed a second debridement (VARD) and 20.8% an open necrosectomy. Mortality was of 11.4%.
REFERENCES
1. Baron TH, DiMaio CJ, Wang AY, Morgan KA. American Gastroenterological Association Clinical Practice Update: Management of Pancreatic Necrosis. Gastroenterology. 2020; 158(1): 67-75.e1. [ Links ]
2. Cao F, Duan N, Gao C, Li A, Li F. One-Step verse Step-Up Laparoscopic-Assisted Necrosectomy for Infected Pancreatic Necrosis. Dig Surg. 2020; 37(3): 211-219. [ Links ]
3. Calcaterra, Emilio & Obeid, Jorge & Brosutti, Oscar & Garcia Calcaterra, Emilio & Cian, María & García, Maximiliano. (2023). Necrosis pancreática infectada: tratamiento solo con antibióticos. ¿sería el primer paso del step-up approach?. 83. 394 - 401. [ Links ]
4. Bugiantella W, Rondelli F, Boni M, Stella P, Polistena A, Sanguinetti A, et al. Necrotizing pancreatitis: A review of the interventions. Int J Surg. 2016;28 Suppl 1: S163-71. [ Links ]
5. Garg PK, Meena D, Babu D, Padhan RK, Dhingra R, Krishna A, et al. Endoscopic versus laparoscopic drainage of pseudocyst and walled-off necrosis following acute pancreatitis: a randomized trial. Surg Endosc. 2020;34 (3): 1157-1166. [ Links ]
6. Cao F, Li A, Wang X, Gao C, Li J, Li F. Laparoscopic transgastric necrosectomy in treatment of walled-off pancreatic necrosis with sinistral portal hypertension. BMC Surg. 2021; 21(1): 362. [ Links ]
7. Bang JY, Arnoletti JP, Holt BA, Sutton B, Hasan MK, Navaneethan U, et al. An Endoscopic Transluminal Approach, Compared with Minimally Invasive Surgery, Reduces Complications and Costs for Patients With Necrotizing Pancreatitis. Gastroenterology. 2019; 156(4): 1027-1040.e3. [ Links ]
8. Nguyen AK, Song AJ, Swopes T, Ko A, Lim BS. Percutaneous Endoscopic Necrosectomy of Complex Walled-Off Lateral Necrosis of the Pancreas with the Aid of Laparoscopic Babcock Forceps: A Case Report of an Endoscopic and Radiologic Team Approach. Perm J. 2019; 23: 18-230. [ Links ]
9. Dua MM, Jensen CW, Friedland S, Worth PJ, Poultsides GA, Norton JA, et al.Isolated pancreatic tail remnants after transgastric necrosectomy can be observed J Surg Res. 2018; 231: 109-115. [ Links ]
10. Wronski M, Cebulski W, Witkowski B, Jankowski M, Klucinski A, Krasnodebski I, et al. Comparison between minimally invasive and open surgical treatment in necrotizing pancreatitis. J Surg Res. 2017; 210: 22-31. [ Links ]
11. Bendersky V, Mallipeddi M, Perez A, Pappas N. Necrotizing pancreatitis: challenges and solutions. Clin ExpGastroenterol. 2016; 9: 345-350. [ Links ]
Responsible editor: Helmut A. Segovia Lohse. https://orcid.org/0000-0003-3255-5345. Universidad Nacional de Asunción. Facultad de Ciencias Médicas. San Lorenzo, Paraguay. Ministerio de Salud Pública y Bienestar Social. Hospital General de Lambaré. Paraguay
Conflict of interest
Author’s contribution
All authors participated on the information search, data recollection, draft’s redaction, critical revision of the manuscript and final approval of it.
Funding
Ethical considerations
Received: May 18, 2023; Accepted: March 15, 2024











 texto en
texto en 



