Introduction
Since the first months of the beginning of the COVID-19 pandemic, the World Health Organization (WHO) provided a set of recommendations to control and reduce the spread of the SARS-CoV-2 virus1. Thus, following these recommendations, countries around the world restricted movement and social interactions in groups, and recommended social distancing, constant hand washing and the use of face masks2. Regarding face masks, it has been indicated that their use reduces the amount of virus inhaled by the individual, which would decrease the transmission of SARS-CoV-2 and the resulting COVID-19 load3,4). Simulation studies indicated that the presence of low percentages of people wearing masks would result in widespread COVID-19 infection in the absence of other strategies to mitigate disease5. In Peru, a simulation study indicated that the implementation of preventive measures such as the use of masks, together with the use of alcohol and social distancing, generated a slower evolution of the pandemic6. The same previous study concluded that the probability of becoming infected with COVID-19 reached 90% when an infected person and another susceptible person were not wearing a mask; the probability drops to 0.5% when both people wore a mask and a face shield, the use of only a mask makes the probability of contagion reach 1.5%; and finally, when the infected person wears a mask and another susceptible person does not, the probability reaches 5%.
However, the use of facemasks during the outbreak differed according to the time of the pandemic and the location7. For example, the use of facemasks became ubiquitous in different Asian countries at the beginning of the pandemic8; whereas, in the United States some authorities discouraged the purchase of facemasks for use by healthy persons and other states of the country left the use of facemasks to individual choice9. Moreover, a study conducted in 38 countries indicated that the use of facemasks varied over time. Thus, a group of countries showed a higher and constant use of masks (more than 75 %) from April to October 2020 (this was the case of some Latin American countries such as Chile, Argentina and Colombia, etc.); other countries showed a relatively low use in April, but it increased and remained at high levels in Brazil, Portugal, Canada, etc.; whereas, a consistently low use (less than 25 %) was observed in European countries such as Denmark, Sweden and Norway10. Another study, using a photoepidemiology method, indicated that the rate of facemask usage in closed environments, such as international airports, during the first months of the pandemic was highest in Asia, followed by South America and very low in the USA11. Thus, the use of face masks has been one of the most controversial and debated public health preventive behavior during the pandemic12.
One of the main topics in debate is oriented towards mask usage after acquiring an adequate level of vaccination coverage against COVID-19. A recent study indicated that the mask use must be maintained even if optimal vaccination coverage was achieved and even if herd immunity levels were exceeded, because virus transmission does not stop when high levels of coverage are achieved; furthermore, the use of masks would prevent additional cases of COVID-192. In Peru, a high proportion of fully immunized people against COVID-19 (84.76%)13 has mitigated the severity of the disease. Thus, under the recommendation of experts, the Peruvian government issued Supreme Decree 118-2022-PCM, which indicated that the use of masks is optional in open spaces and ventilated enclosed spaces as of October 1, 2022. This decision was based on the decrease in cases, hospitalizations, and death in the weeks prior to the publication of the decree. Although many people stopped wearing masks as stipulated in the regulation, a group of people continued to wear them in open and in closed ventilated spaces.
The reasons for wearing or not a mask are diverse and can be personal, social, cultural, psychological and even economic. It has been suggested that not wearing of masks is related to physical discomfort, annoyance, interference in daily interactions and some beliefs14,15. Likewise, the presence of anti-mask and anti-vaccine attitudes, political ideologies and perceptions of their ineffectiveness are related to refusal to wear masks16. On the other hand, greater trust in science and perceived greater efficacy of the mask to reduce contagion15 and fear17 are factors that favor mask-wearing behavior. From the fear-impulse theory18, fear can generate changes, which decrease if the fear is excessive, since behaviors will focus on fear and not on facing the risk. On the other hand, the same situation or information does not have the same effect on all people, because some comply with the recommendations, others do not; while another group complies with the measures in a given place and time, but not in another.
From the health belief model19, it is suggested that beliefs about disease threats and the effectiveness of measures can predict health behaviors. The latter is important, because if the reason for wearing masks was compliance with imposed norms, when the obligation disappeared, people would stop wearing them. However, along with the norms, beliefs and habits have appeared, which would cause behavioral change to persist, even in the absence of external laws. As mentioned, this has been observed recently in Peru, where it was still common to find people walking in open places wearing masks, even though it was not mandatory to do so in outdoor environments. In view of this situation, the objective of the present study was to find out the reasons why people continued to wear masks despite the fact that it was not mandatory in outdoor environments. This would allow governments and public health institutions to have scientific information to make rational recommendations on the use of masks despite not being mandatory, after achieving an adequate level of vaccination coverage against COVID-19.
Methods
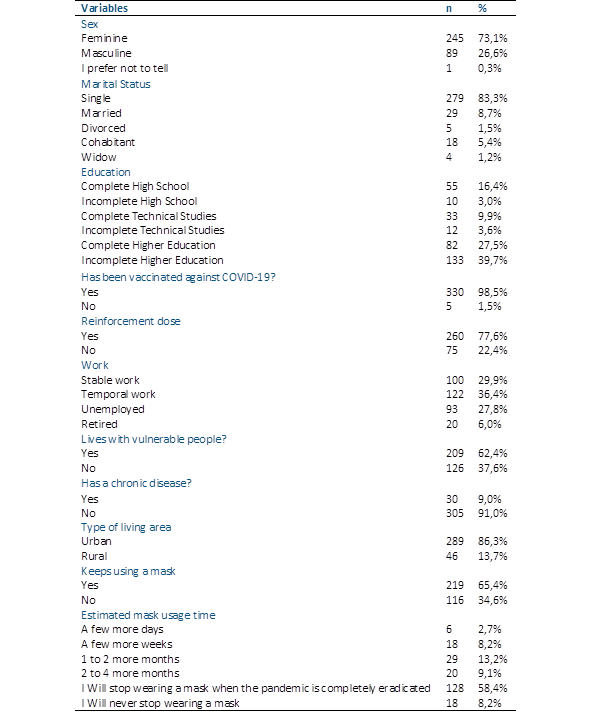
Participants: A total of 335 people with an average age of 26.11 years (SD= 10.02), selected by non-probabilistic sampling, participated in the study. Inclusion criteria were: 1) to be residents of Peru; 2) to be over 18 years of age; and 3) to give informed consent. Most participants were women (73.1%). In addition, most participants reported being single (83.3%) and having completed or incomplete university studies (67.2%). 98.5% indicated having been vaccinated against COVID-19 and 77.6% were vaccinated with their booster doses. 62.4% live with vulnerable people and 91.0% do not suffer from chronic diseases. Regarding the work environment, 29.9% indicated having a permanent job and 36.4% a temporary job. Regarding the use of masks, the majority (65.4%) continue to wear masks in open and closed places with ventilation, even though this was no longer obligatory at the time of the study. Finally, more than 50% of the participants (58.4%) indicated that they will stop wearing masks when the pandemic is totally eradicated. Table 1 reports in more detail the sociodemographic and health characteristics of the sample.
Instruments
A data collection form was prepared with two sections. In the first section, sociodemographic and health information on the participants was requested, such as age, sex, marital status, educational level, vaccination against COVID-19, booster vaccine dose, work, living with vulnerable people, diagnosis of chronic disease, type of area where they live, use of mask and estimated time of mask use. A second section included the following question: "Why do you continue to wear the mask even though it is optional in open and closed ventilated spaces?" and a space of four lines to write a response. Participants were invited to write their answer on these lines and were told that it would not be a problem if they did not complete all the lines.
Procedures and ethics
The study protocol was evaluated and approved by the Institutional Committee for the Protection of Human Subjects in Research (CIPSHI) of the University of Puerto Rico (No. 2223-006). Data was collected during October 3 and 10, 2022, through an online survey built in Google Forms that was distributed via social networks (Instagram, Twitter and Facebook) and email. In the online survey, the objective of the study, anonymity warrant, confidentiality, and consent were first presented. Participants were required to read and accept the informed consent before continuing to the other questions. There was no time limit for answering the survey; however, it lasted an average of 5 minutes.
Data Analysis
Data obtained from the last open-ended question of the instrument was analyzed using a Discursive Textual Analysis (DTA) and an exploratory analysis through IRAMUTEQ (Interface de R pour les Analyses Multidimensionnelles de Textes et de Questionnaires) version 0.7 Alpha220. This program speeds up the retrieval of text and word segments, identifying their association and enabling the grouping of statistically significant words based on their co-occurrence in the whole corpus21. The analysis was conducted by the following steps. First, raw data was reviewed, corrected, and organized into a monothematic corpus of analysis. Each response was separated by a command line and related to four variables that were considered relevant for further classification: Sex, vaccination status, chronic disease and if the respondent lives with a vulnerable person (e.g. **** *sexo_F *Vac_SI *Vul_Si *Cron_No Es necesario protegerme a mí y a mi familia de un potencial contagio de esta u otra infección viral respiratoria.). This process was carried out by using LibreOffice Calc and LibreOffice Writer. The file was saved as a text document using UTF-8 standard encoding (Unicode Transformation Format 8 bit codeunits). The total number of text segments included in the analysis was 217. Next, a basic lexicography was applied to lemmatize the whole corpus and establish the word frequency. Then, a Similarity Analysis was carried out to find the relations between text segments throughout the whole corpus, since the Descending Hierarchical Classification (DHC) pilot trial resulted only in a retention of 61.75%, which is less than the 75% recommended by Camargo y Justo22. So, the similarity analysis helped to further establish the connections between words based on their proximity and frequency in the corpus, helping researchers to articulate meaning based on visually presented connections. When carrying out the similarity analysis using the variables, no relevant differences were found between groups. So, a general similarity analysis was used to articulate the main motives that participants refer to have in relation to mask usage.
Results
Exploratory Statistical Analysis
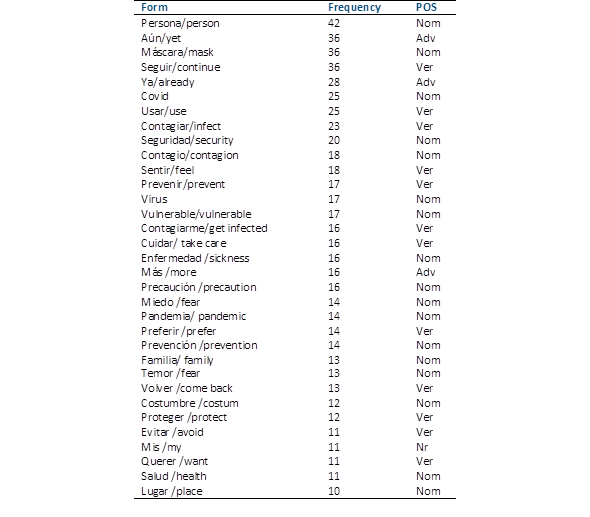
After the lemmatization, the analysis of the 217 text segments resulted in a total of 108 active forms (adjectives, names, and verbs). The following table shows the first 33, with a frequency of ≥10 which show semantic relevance related to the monothematic corpus (Table 2).
Similarity Analysis
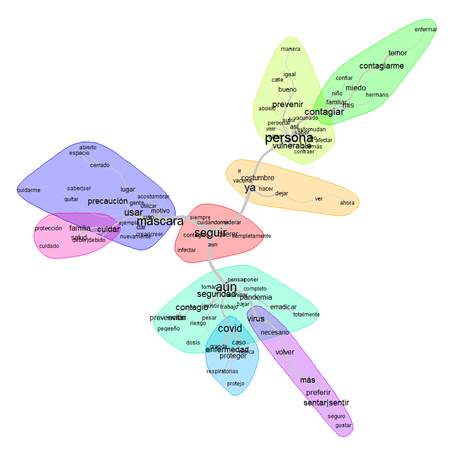
A similarity analysis was conducted with the whole list of active forms. Communities and Halo options were selected to represent the most related words. Figure 1 shows the similarity tree that organizes the active forms in three main branches which represent the reasons and motives for the continuation on the use of masks. The size of the words illustrates their frequency, while the thickness of the lines represents the strength of the relation based on proximity, as it is shown in Figure 1.
As a general finding, the center of the tree aggregates terms such as ‘seguir’(continue), ‘cuidándome’ (take care of myself), ‘contagios’ (infections), which show the intention of continuing to wear a mask, even if the restrictions are lifted, to avoid contagion, not only of COVID-19, but of other respiratory diseases such as tuberculosis and the Flu: “Debido a que es un gran recurso para evitar contagios no solo del Covid- 19, sino también de la gripe, por ejemplo” (Because it is a great resource to avoid contagion not only of COVID-19, but also the flu, for example).
The two communities to the right of figure 1 relate terms such as ‘máscara’ (mask), ‘precaución’ (precaution) and ‘cuidar’ (take care). In a general sense, tese communities specify the need to wear a mask as a precautionary measure in open and closed spaces. Also, it describes the need to take care of one’s own family, preventing the infection of loved ones: “Porque prefiero seguir guardando cierta precaución y además porque aún no me hago costumbre a no usarla, debo volverme a adaptar más al hecho de ya no llevarla” (Because I still prefer to be cautious and also because I am not yet used to not wearing it, I have to get used to the fact of not wearing it anymore).
The following three communities, orange, yellow and green represent, first, in close relation to the previous group of communities, the use of the mask is shown to be a custom integrated into the habits of the participants. Nevertheless, yellow and green communities reveal a strong connection between the terms ‘persona’ (person), ‘vulnerable’ (vulnerable), ‘prevenir’ (prevent), ‘contagiar’ (infect), ‘contagiarme’ (get infected), ‘miedo’ (fear) and ‘temor’ (dread).
These terms illustrate a motive related to the prevention of both infecting vulnerable people (being children, older adults or family members) and being infected. Both possible situations generate emotions such as fear and dread towards infection with COVID-19: “Siento temor que en cualquier momento pueda contagiarme y contagiar a los mios” (I feel fear that in any moment I could get infected and infect my loved ones).
The next related communities, highlighted by light blue, light green and purple in the bottom of the tree, relate terms such as ‘aún’(yet), ‘seguridad’ (security), ‘contagio’ (infection), ‘covid’, ‘virus’, ‘enfermedad’ (desease), ‘prevención’ (prevention). These further develops the general reason to wear a mask, specifying the psychological need of security in relation to the prevalence of the pandemic, which has not yet been completely eradicated. In this context, participants recognize the need to further prevent a possible infection and transmission of the virus: “porque considero que la enfermedad aún no está erradicada del todo, por precaución, mi salud y la de los demás prefiero seguir usando mascarilla” (Because I consider that the disease is not yet completely eradicated, for precaution, my health and the health of others I prefer to continue wearing a mask.
As a general finding, the center of the tree aggregates terms such as ‘seguir’(continue), ‘cuidándome’ (take care of myself), ‘contagios’ (infections), which show the intention of continuing to wear a mask, even if the restrictions are lifted, to avoid contagion, not only of COVID-19, but of other respiratory diseases such as tuberculosis and the Flu: “Debido a que es un gran recurso para evitar contagios no solo del Covid- 19, sino también de la gripe, por ejemplo” (Because it is a great resource to avoid contagion not only of COVID-19, but also the flu, for example).
The two communities to the right of figure 1 relate terms such as ‘máscara’ (mask), ‘precaución’ (precaution) and ‘cuidar’ (take care). In a general sense, tese communities specify the need to wear a mask as a precautionary measure in open and closed spaces. Also, it describes the need to take care of one’s own family, preventing the infection of loved ones: “Porque prefiero seguir guardando cierta precaución y además porque aún no me hago costumbre a no usarla, debo volverme a adaptar más al hecho de ya no llevarla” (Because I still prefer to be cautious and also because I am not yet used to not wearing it, I have to get used to the fact of not wearing it anymore).
The following three communities, orange, yellow and green represent, first, in close relation to the previous group of communities, the use of the mask is shown to be a custom integrated into the habits of the participants. Nevertheless, yellow and green communities reveal a strong connection between the terms ‘persona’ (person), ‘vulnerable’ (vulnerable), ‘prevenir’ (prevent), ‘contagiar’ (infect), ‘contagiarme’ (get infected), ‘miedo’ (fear) and ‘temor’ (dread). These terms illustrate a motive related to the prevention of both infecting vulnerable people (being children, older adults or family members) and being infected. Both possible situations generate emotions such as fear and dread towards infection with COVID-19: “Siento temor que en cualquier momento pueda contagiarme y contagiar a los mios” (I feel fear that in any moment I could get infected and infect my loved ones).
The next related communities, highlighted by light blue, light green and purple in the bottom of the tree, relate terms such as ‘aún’(yet), ‘seguridad’ (security), ‘contagio’ (infection), ‘covid’, ‘virus’, ‘enfermedad’ (desease), ‘prevención’ (prevention). These further develops the general reason to wear a mask, specifying the psychological need of security in relation to the prevalence of the pandemic, which has not yet been completely eradicated. In this context, participants recognize the need to further prevent a possible infection and transmission of the virus: “porque considero que la enfermedad aún no está erradicada del todo, por precaución, mi salud y la de los demás prefiero seguir usando mascarilla” (Because I consider that the disease is not yet completely eradicated, for precaution, my health and the health of others I prefer to continue wearing a mask).
Discussion
The use of masks has been reported to be a protective barrier that reduced the risk of COVID-19 transmission among the population23. As of October 1, it was no longer mandatory in Peru to wear masks in open spaces. Even so, after this regulation came into effect, people were observed walking in open spaces wearing masks. In view of this situation, the objective of the present study was to find out the reasons why people continued to wear masks even though it was not mandatory in outdoor environments.
A first and central finding indicated that people continued to wear masks, despite the lifting of restrictions, to avoid contagion, not only of COVID-19, but also of other respiratory diseases. In addition, the prevention of possible infection and transmission of the virus is also focused on family and vulnerable people. This agrees with the idea that people would wear masks to obtain a personal benefit by avoiding getting infected with the virus or to benefit others by not transmitting the virus24. In this sense, although obtaining benefits for oneself is one of the strongest factors for the use of masks, the findings demonstrate that people are social beings who are willing and able to cooperate with others25,26. This could promote attitudes and behaviors related to the restriction of daily activities, such as not wearing masks when it is no longer mandatory, to protect risk groups from COVID-1927. Thus, the use of a mask would indicate a level of care and respect towards others28. Similarly, this could imply the presence of a collectivist variable, characterized by the perception of an interdependent self that cares about the needs of the group29) as a predictor of mask use. It has previously been suggested that more collectivistic societies tend to wear facemasks more as a preventive measure to cope with the pandemic than members of more individualistic societies30. As the presence of the collectivist variable was not assessed in this study, this remains a working hypothesis for future studies.
Similarly, the findings can be explained from the theory of planned behavior (TPB)31, where the perception of the risk of contagion to oneself and others has a positive impact on prevention practices during epidemics. This would have generated a greater awareness of Peruvians about the severity of COVID-19, susceptibility, and mortality of the disease to develop positive beliefs about how masks would help overcome the pandemic32. In this regard, a relevant variable, and one that is also present in the health belief model (EHBM)33, is fear. This is clearly observed in the strong relationships found between the terms: person, vulnerable, prevent, infect, infect me, and fear. Fear has been one of the most important emotions during the COVID-19 pandemic, as it is an expected response to threatening situations34. This fear generates coping responses that seek to manage threats and lead to adopting and maintaining preventive health behaviors35.
The findings have theoretical and practical implications. The results allow a better understanding of why some people wear masks in public even though it is not mandatory at the time of data collection. In addition, people wearing masks for personal benefit or to benefit others by not transmitting the virus suggests the presence of underlying unobservable cultural phenomena that may contribute to mask use. This could function as an argument for the design of policies related to the use or non-use of masks, which should consider pre-existing social norms and experiences related to their use10.
Despite the important results, the study has several limitations. First, because the sample was selected through non-random sampling, there is the possibility of selection bias and problems in generalizing the findings, since the participants are not representative of the general population of Peru. The selection bias caused the sample of the current study to be mostly female, single and with university studies in progress or completed. Second, the use of an online survey meant that the response rate was likely to be comparatively lower in lower socioeconomic groups and those living in rural areas that do not have full access to the Internet. Third, the study was of a cross-sectional nature where data were collected in a single time period immediately after the Peruvian government indicated that mask use is optional in open spaces and ventilated enclosed spaces. However, it would be interesting to be able to conduct a longitudinal study where this behavior in Peruvian citizens could be followed up. Fourth, the use of self-report questions could generate the presence of social desirability. However, their use was important since the reasons for mask use are based on personal feelings and had to be further elaborated by participants.
In conclusion, people continued to wear masks, despite the lifting of restrictions, to prevent the spread of COVID-19 and other respiratory diseases. In addition, this prevention of possible infection and transmission of the virus is also focused on the family and vulnerable people. Therefore, it could be indicated that the practice of wearing masks may be influenced by individual perceptions of risk and interpretations of responsibility and solidarity towards others. It should be considered that the non-obligatory use of masks should be part of a safer preventive health approach. Despite the non-obligatory use of masks, public health messages should be addressed to people who decide to continue wearing them, such as the proper wearing of masks, the use of clear, simple, and evidence-based information on protection against the transmission of respiratory diseases and being transparent about the benefits and precautions regarding mask usage. This will help Peruvians form more realistic expectations about the pros and cons of wearing or not wearing masks. In this way, more informed decisions could be made about preventive health practices. This is even more important because at the time of writing the manuscript (December 6, 2022), Peru was in the fifth wave of the COVID-19 pandemic.