Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Cirugía paraguaya
On-line version ISSN 2307-0420
Cir. parag. vol.47 no.3 Asunción Dec. 2023
https://doi.org/10.18004/sopaci.2023.diciembre.37
Case Report
Neuromuscular and vascular hamartoma of the small intestine: a case report
1Universidad Nacional de Asunción, Facultad de Ciencias Médicas, Hospital de Clínicas. San Lorenzo, Paraguay
Small bowel neoplasms are extremely rare (2%) and generally malfor- mative, neuromuscular and vascular hamartoma being even rarer with approximately 28 cases reported since 1982, when it was first described. As more common clinical manifestations, obstructive abdominal pain and occlusive pictures in the intestinal lumen are described, however, it can also mimic clinical features of inflammatory bowel disease and other reactive conditions. Imaging studies may show signs of stricture, intus- susception, or directly a polypoid mass. Surgical resection is curative and no recurrences have been reported.
Keywords: Hamartoma; neuromuscular and vascular hamartoma; small intestine
Las neoplasias de intestino delgado son extremadamente raras (2%) y generalmente malformativas, el hamartoma neuromuscular y vascular es aún más raro con aproximadamente 28 casos reportados desde 1982, cuando fue descrito por primera vez. Como manifestaciones clínicas más comunes, se describen el dolor abdominal obstructivo y cuadros oclusivos en la luz intestinal, sin embargo, también puede imitar características clínicas de enfermedad inflamatoria intestinal y otras afecciones reactivas. En los estudios de imagen, se pueden observar signos de estenosis, invaginación intestinal o directamente una masa polipoide. La resección quirúrgica es curativa y no se han registrado recurrencias
Palabras clave: Hamartoma; Hamartoma neuromuscular y vascular; intestino delgado
INTRODUCTION
Small bowel neoplasms are extremely rare (2%) and generally malformative, neuromuscular and vascular hamartoma being even rarer with approximately 28 cases reported since 1982, when it was first described1,2.
Many published cases even cast doubt on the existence of this pathology due to the clinical similarity and histology with reactive pathologies such as Crohn’s disease, ischemic enteritis, or radiation enteritis, which has been a cause for debating whether the injury really is a hamartoma or a “burned” phase of said pathologies.
This is a case report of a 67-year-old female patient with 2-month evolutive symptoms of black stool and cathartic habs’ alterations, imagery studies yielded signs of intestinal intussusception, therefore the patient was submitted to small bowel resection of the affected area and ileal-anal anastomosis with manual suture in a single plane. The patient reported a proper evolution after the procedure and was discharged.
CLINICAL CASE
67-year-old female patient with 2-month evolutive symptoms of black stools and presyncope, hence she attends a physician although no hemodynamic alterations are detected, therefore she is discharged. She reports a second episode approximately 1 month afterwards with a 5 g/dl hemoglobin drop which required a 2-volume concentrated red blood cells transfusion. Furthermore, she reports alternating episodes of diarrhea and constipation. Known high blood pressure patient in current treatment with telmisartan/amlodipine 40/5mg e/24hs and Type 2 mellitus diabetes in current treatment with metformin 850 mg e/24hs and glimepiride 4 mg e/24hs.
Abdominal ultrasound yielded a cross-section rounded formation in the hypogastrium and right iliac fossa, formed by hypo and hyperechoic concentric layers (cockade sign) of approximately 50 mm of diameter. Said formation continues with thin folds, which are not dilated, although of thickened walls (9mm of thickness) with proper color Doppler vascularity, lack of gastrointestinal peristalsis.
In the contrasted tomography, signs of intestinal intussusception of thin folds (ileal) can be seen close to the ileocecal junction in the hypogastrium region, the compromised thin folds show thickened walls of up to 7 mm of thickness with present parietal enhancement without signs of proximal intestinal obstruction (see Figure 1). Furthermore, an upper gastrointestinal endoscopy and colonoscopy are performed without relevant findings.
An exploratory laparotomy was performed where ileal-anal intussusception without transition zone nor occlusion signs was reported (see Figure 2). A resection of the affected area of approximately 25 cm long 90 cm away from the ileocecal valve with term-terminal ileo-anal anastomosis with manual suture in a single layer was performed.

Figure 1. Contrasted tomography where intestinal intussusception of thin folds (A) close to the ileocecal junction can be observed.
In the macroscopy, a brownish, heterogeneous, smooth external surface was observed, with a grayish beige internal sur- face with preserved intestinal folds and walls of up to 0.7 cm of thickness. An elongated polypoid formation of 11 cm long and 3 cm wide was observed, coated by grayish beige mucous of irregular aspect which stays 6 cm away from the closest resection margin.
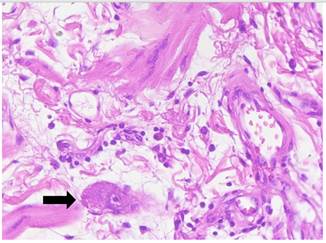
In the histology, said polypoid formation presented itself coated by benign small intestine mucous, without atypia and ulcerated on the distal portion. In its own slide, parallel to the crypts, smooth muscle bundles were observed. The muscularis mucosae was found disorganized and improperly constituted. In the center of the injury corresponding to the submucosa, nu- merous vessels of different calibers were observed, of abnormal appearance. The major vessels with hyalinization and eccentric myxoid changes to an intimate level; others presented them- selves with recent thrombosis, partially rechanneled, irregularectatic venous structures, and small vessels of walls with hyperplasia, as well as small and medium caliber vascular changes that partially extend to the mucous and intestinal villus. Fur- thermore, abundant disorganized smooth muscle tissue around said vessels was observed. (see Figures 3 and 4)
The macroscopic and histological findings are compatible with neuromuscular and vascular hamartoma of the small intes- tine (11 cm) of polypoid pattern.
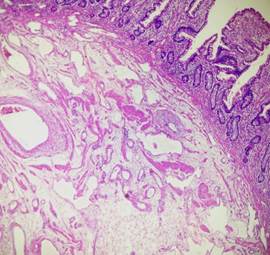
Figure 3. Jejunal submucosa, disorganized muscle fascicles, and numerous hemangiomatous blood vessels were observed.
DISCUSSION
Neuromuscular and vascular hamartoma of the small intestine is a rare condition first described in 1982. There are approximately 28 known published cases to this date, in which an aver- age age of 53 years old is observed as presentation age, generally at jejunal and ileum level, although there has been a reported case in the cecal appendix (1,3,5). In our case, the 67-yeard-old patient presents an ileal-level tumor at approximately 90 cm from the ileocecal valve.
As the most common clinical manifestations, it is described obstructive abdominal pain and occlusion at intestinal light, however, it can also mimic clinical characteristics of intestinal inflammatory disease and other reactive affections, hidden gas- trointestinal bleeding, and anemia by iron deficiency (1,2). In the case of our patient, both types of symptoms were present due to her presenting episodes of bleeding as well as cathartic habits’ alterations.
In the imagery studies, signs of stenosis, intestinal intussusception or directly a polypoid mass can be observed (3). In the presented case, the ultrasound yielded a cross-section round formation, formed by hypo and hyperechoic concentric layers (cockade sign) of approximately 50 mm of diameter, and in the tomography, signs of intestinal intussusception of thin folds (il- eal) close to the ileocecal junction in the hypogastrium region.
She presents with abnormal proliferation, no neoplasms of cellular elements which are generally part of the gastrointestinal mucous and submucosa. Neoplasm injuries of the small intestine, besides being extremely rare (2%), are generally malformative. Cases with single or multiple stenoses, or injuries of mass similar to simple polyps which can also be single or multiple were reported (2,3). Coincidently, our patient reported a single elongated polypoid injury, coated by grayish beige mucous of irregular aspect.
At histological level, disorganized elements of unmyelinated nerve fibers were observed, as well as ganglion cells, muscle fascicles, and hemagiomatous vascular channels which were found in the mucous and submucosa of the small intestine’s walls(1). In our patient’s case, abundant disorganized and improperly constituted smooth muscle tissue was observed, and in the submucosa, vessels of different calibers and of anomalous aspect were observed.
Surgical resection is healing, and no recurrences have been registered (1,2), in our patient’s case the surgery was successfully performed, and the patient was discharged 5 days afterwards with a favorable evolution and without recurrences up to this date.
REFERENCES
1. Dhruv S, Anwar S, Kashi M, Mukherjee I. Hamartoma neuromuscular y vascular: ¿punto de partida en la enfermedad de Crohn? J Med Casos. Agosto 2021;12(8):332-337. doi: 10.14740/jmc3727. Epub 2021 Jul 3. PMID: 34434482; PMCID: PMC8383593. [ Links ]
2. Caruso ML, Cavalcanti E, De Michele F, Ignazzi A, Carullo R, Mastronardi M. Small bowel capsule endoscopy revealing neuromuscular and vascular hamartoma of the jejunum: A case report. Medicine (Balti- more). 2018 Apr;97(15):e0196. doi: 10.1097/MD.0000000000010196. PMID: 29642143; PMCID: PMC5908559. [ Links ]
3. Elstner KE, Vickers CR, Gett RM, Qiu MR, Killen LV. Neuromuscular and vascular hamartoma as an unusual cause of small bowel obstruction. Int J Surg Case Rep. 2016;26:1-3. doi: 10.1016/j.ijscr.2016.06.042. Epub 2016 Jul 6. PMID: 27420120; PMCID: PMC4949502. [ Links ]
4. Scintu F, Capra F, Giordano M, Frau G, Mascia R, Comella D, Rais M, Casula G. L’amartoma neuromuscolare e vascolare dell’intestino tenue. Presentazione di un caso clinico e revisione della letteratura [Neuromuscular and vascular hamartoma of the small intestine. Report of a clinical case and review of the literature]. Chir Ital. 2001 May-Jun;53(3):393-8. Italian. PMID: 11452826. [ Links ]
5. Sasaki T, Furuhata T, Nishimura M, Ono T, Noda A, Koizumi H, Miyaji- ma N, Otsubo T. An extremely rare case of neuromuscular and vascular hamartoma of the appendix. Surg Case Rep. 2020 Aug 24;6(1):216. doi: 10.1186/s40792-020-00970-2. PMID: 32833104; PMCID: PMC7445220. [ Links ]
6. Ayyanar P, Purkait S, Mishra TS, Patra S, Mitra S. Histopathologic Spectrum of Neuromuscular and Vascular Hamartoma With Special Reference to the Vasculopathic Phenomenon. Int J Surg Pathol. 2020 Jun;28(4):382-392. doi: 10.1177/1066896919890129. Epub 2019 Nov 24. PMID: 31760840. [ Links ]
7. Crothers JW, Zenali M. Neuromuscular and Vascular Hamartoma of the Small Intestine: An Exuberant Reparative Process Secondary to Chronic Inflammation. Int J Surg Pathol. 2015 Dec;23(8):673-6. doi: 10.1177/1066896915600518. Epub 2015 Aug 14. PMID: 26275621. [ Links ]
Declaration of contribution of each author to the pres- ent work for publication: All three authors of the work have contributed to the writing of the draft and critical revision of its content, as well as the revision and approval of the final article.
Received: February 17, 2023; Accepted: December 10, 2023











 text in
text in