Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Cirugía paraguaya
versão On-line ISSN 2307-0420
Cir. parag. vol.47 no.3 Asunción dez. 2023
https://doi.org/10.18004/sopaci.2023.diciembre.19
ORIGINAL ARTICLE
Experience in the videolaparoscopic surgical management of achalasia at the Hospital Nacional de Itauguá, period 2017-2021
1Hospital Nacional. Itauguá, Paraguay
Introduction: achalasia is a motility disorder of the distal esophagus of unknown etiology, manometrically characterized by loss of esophageal peristalsis and lack of lower esophageal sphincter relaxation; radiograph- ically by aperistalsis, esophageal dilatation, with minimum opening of the lower esophageal sphincter, and endoscopically by dilated esophagus. Objective: prove the experience of the videolaparoscopic treatment of esophageal achalasia in the Hospital Nacional de Itauguá. Methods: Observational, descriptive, cross-sectional, retrospective study. Results: A total of 31 patients were evaluated; 15 were men and 16 were women; average age was 54.19 years old. Dysphagia was the predominant consultation motive, followed by regurgitation, vomiting and sternal pain. Most of the patients presented a Grade II esophageal dilatation through esophagram. Upper endoscopy was used in 100% of the patients as a diagnosis method, esophagram was used in 74%, and manometry was used in 32%. The most frequently used surgical technique was laparoscopic Heller’s cardiomyotomy with Dor fundoplication (71%). No mortality rate was registered. Conclusion: Dysphagia is the main reason for consultation and laparoscopic Heller’s cardiomyotomy with Dor fundo- plication is the most frequently used surgery for esophageal achalasia.
Keywords: achalasia; esophagus; dysphagia; manometry; Heller- myotomy
Introducción: La acalasia es un trastorno motor esofágico primario de etiología desconocida caracterizada manométricamente por pérdida del peristaltismo esofágico y relajación insuficiente del esfínter esofágico inferior; radiográficamente por aperistalsis, dilatación esofágica, con mínima apertura del esfínter esofágico inferior, y endoscópicamente por esófago dilatado. Objetivo: demostrar la experiencia del tratamiento videolaparoscópico de la acalasia esofágica en el Hospital Nacional de Itauguá. Métodos: Estudio observacional descriptivo, retrospectivo de corte transversal. Resultados: Se evaluaron un total de 31 pacientes; 15 fueron hombres y 16 mujeres; la edad promedio fue de 54,19 años. La disfagia fue el motivo de consulta predominante seguido de regurgitación, vómitos y dolor retroesternal. La mayoría de los pacientes presentaron una dilatación esofágica Grado ll por esofagograma. Como métodos diagnósticos se utilizaron la EDA en el 100% de los pacientes, el esofagograma en un 74% y la manometría en 32%. La técnica quirúrgica mayor frecuencia fue la cardiomiotomía laparoscópica de Heller con funduplicatura de Dor (71%). No se registraron tasas de mortalidad. Conclusión: La disfagia esel principal motivo de consulta y la cirugía más frecuentemente realizada para la acalasia esofágica en la cardiomiotomía laparoscópica de Heller con funduplicatura de Dor.
Palabras Claves: acalasia; esófago; disfagia; manometría; miotomía de Heller
INTRODUCTION
Achalasia is a motility disorder of the distal esophagus of un- known etiology manometrically characterized by loss of esophageal peristalsis and lack of lower esophageal sphincter (LES) relaxation; with radioscopical proof of aperistalsis, esophageal dilatation with minimum opening of the LES and bird-beak appearance, improper emptying contrast; and endoscopically by dilated esophagus with retained saliva, liquid, and non-digested food in absence of mucous membrane’s stenosis or tumor1.
Achalasia occurs equally between men and women with an incidence of 1 in 100,000 individuals annually, without racial predilection. The incidence peak presents itself between 30 to 60 years old2.
It is of autoimmune, viral, or neurodegenerative etiology; the secondary most frequent cause is Chagas disease, produced by endogenous protozoan Trypanosoma cruzi from South and Central America; this parasite causes long-term autonomic dysfunction of the esophagus’ (and other organs’) intramural neurons, which induce achalasia symptoms2.
The main clinical manifestations are: dysphagia in 95% of cases; regurgitation in 75%, chest pain, pyrosis, weight loss and nighttime cough3.
Regarding the diagnosis methods, the ones used are esophageal manometry, dynamic esophagography and upper gas- trointestinal endoscopy (UGE). Esophageal manometry is considered the golden pattern for achalasia diagnosis given the peculiarity of being able to confirm and distinguish be- tween three types of different manometric patterns (Chicago Classification). Type 1 is characterized by minimal esophageal pressurization, type 2 presents panesophageal pressurization, and type 3 is distinguished by secondary spasms to the spastic contractions. In the esophagram, the diagnosis is backed by findings such as esophageal dilation, a gastroesophageal tight junction with bird-beak appearance, aperistalsis and improper emptying contrast. As for upper gastrointestinal endoscopy, the main function is to discard a mechanical obstruction or a pseudoachalasia, given that they can emulate clinical as well as manometrical achalasia4.
Achalasia treatment continues to be palliative and is aimed towards functional and symptomatic relief through the slit of the lower esophageal sphincter5.
Amongst the therapeutic options, the laparoscopic approach has proven to be a safe, replicable, and effective technique that achieves control over the symptoms with minimal morbility6.
The objective of the present study is to prove the experience in the videolaparoscopic handling of the esophageal achalasia in the Hospital Nacional de Itauguá.
METHODS
Observational, descriptive, cross-sectional, retrospective study on patients who attended the general surgery service of the Hospital Nacional de Itauguá during the period between March 2017 and March 2021 (4 years). Adult patients (18 years old and above) from both genders with completed forms were included, with an esophageal achalasia diagnosis through at least one of these three methods: esophagram, esophageal endoscopy and/ or manometry, and those who were submitted to videolaparoscopic surgical treatment during the study’s duration. Patients with an achalasia diagnosis who received medical or endoscopic pneumatic dilation treatment; or an open approach surgical treatment were excluded. For the recollection of data, a data instrument was designed where all variables were included, and the data was obtained through the studied patients’ medical forms. The data was anonymously registered within the Micro- soft Office Excel 2010® program and summarized according to the nature of the variables.
RESULTS
31 patients were included, from which 15 were men (48,39%) and 16 were women (51,61%). The average age was 54,19 years old, with a 22 to 85 years-old range.
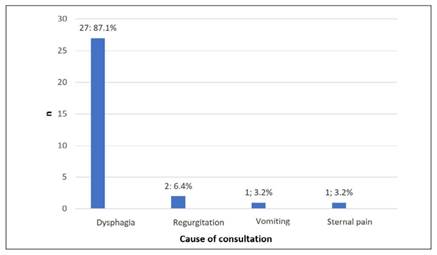
The main cause of consultation was dysphagia in 87,1% of patients, followed by regurgitation in 6,4%; vomiting in 3,2%, and sternal pain in 3,2% (See Graphic 1).
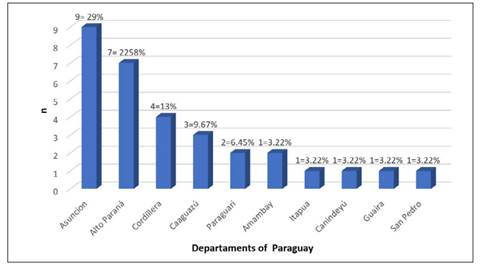
The city of origin of the patients was of 29% from Asunción, 22.58% from Alto Paraná, 13% from Cordillera, 9.67% from Caaguazú, among others (See Graphic 2).
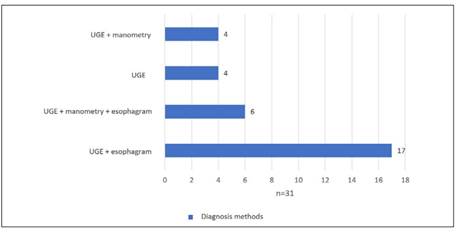
Esophageal achalasia diagnosis was performed most fre- quently through upper gastrointestinal endoscopy with an esophagram (n=17), followed by a least frequent upper gastrointestinal endoscopy, esophagram, and manometry (n=6). Esoph- ageal manometry was only able to be performed in 10 patients (See Graphic 3).
Of the 23 patients with an esophagram, grade II esophageal dilation was recorded in 16 of them (69.5%), grade III esopha- geal dilation in 6 of them (26%), and grade IV in one of them.
As for the surgical technique, the laparoscopic Heller’s car- diomyotomy was performed, and the Dor fundoplication asso- ciated antireflux procedure was done on 22 patients (71%), the Toupet one on 6 (19.3%), and the Nissen one on 3 (9.7%).
The average hospitalization days for each surgical interven- tion before discharge was of 5.22 days, with a range between 2 to 22 days, most of them being dedicated to finishing diagnosis studies. No mortality was registered.
DISCUSSION
Achalasia is a motility disorder of the distal esophagus, whose main symptom is dysphagia. It occurs equally between men and women. There is no racial predilection. The incidence peak presents itself between 30 to 60 years old.
There were no significative differences in regards to gender in the present study, whereas the average age was of 54.19 years old. In a study performed in our country in 2014, Cabral et at observed that the average age was of 57±10 years old, figure slightly higher than the one found in this study7.
The main cause of consultation was dysphagia followed by regurgitation, and vomiting and sternal pain in lesser occasions, data that matches a published work by Méndez-Sánchez from Mexico in 2018, where the most common clinical manifestation was dysphagia for solids followed by the one for liquids2.
More than half of the patients were from Asunción y Alto Paraná, although patients from almost every department of the western region were present.
The diagnosis of said pathology was more frequently per- formed by UGE and esophagram. UGE was performed in all patients (100%), esophagram in 23 (74.2%), and manometry in 10 (32.3%). In a Paraguayan study published in 2016, the main diagnosis methods were chest x-ray and esophagram in 100% of patients, and UGE in less quantity8.
This reflects the current systematic use of UGE and the pro- gressive increase of esophageal manometry as a diagnosis meth- od, although performed in less than a third of the patients. Being manometry the gold standard, this figure represents a limitation of the present study.
An esophageal dilation by esophagram was recorded in all patients, with grade II having the most frequency (69.5%). In their thesis, González Paredes showed that the greater percentage of patients were diagnosed in late-stage achalasia according to the esophagram: Grade II in 33%, Grade III in 5%, and Grade IV in 24% which matches with the findings of the present work.9 The surgical technique performed was laparoscopic Heller’s cardiomyotomy, plus the Dor antireflux procedure on 22 pa- tients (71%) which matches with a published work in our country done by the Instituto de Previsión Social on 2022, where the same technique was performed on 61% of patients10.
The average hospitalization days for said surgical interventions before discharge were of 5.22 days. In the work done by Ramírez Sotomayor published in 2016, the hospitalization days were of 8.82±6.06 days on average8.
The hospitalization days remain very high, due mainly to the delay of diagnosis studies.
As bias of the present study, due partially to the low esophageal manometry usage rate, are the systematic lack of Chagas’ tests in an endemic country such as Paraguay, even though they were performed, it wasn’t studied in every case. It would be interesting to develop protocols to define the necessary diagnosis methods for esophageal achalasia. Another limitation of the study was the lack of long-term follow-ups, most likely due to the patients being from very distant areas to the Hospital Nacional de Itauguá.
CONCLUSION
In the present study a clear gender predilection was not found. The average age was of 54.19 years old.
The main cause of consultation was dysphagia in 87.1% of patients followed by regurgitation, vomiting and sternal pain.
The city of origin of the patients were nearly all the oriental region’s departments of Paraguay.
As diagnosis studies, UGE was performed on 100% of the patients, esophagram in 74.2% (mostly grade II), and manome- try in only 32.2%.
The performed surgical technique was laparoscopic Heller’s cardiomyotomy, most frequently done alongside Dor fundoplication (71%). Toupet and Nissen fundoplication were also per- formed.
The preoperative hospitalization average was high due to de- lays on diagnosis studies. No mortality recorded.
REFERENCES
1. Ferradindo Carvallo F, Umaña Brenes AA. Acalasia como trastorno de la motilidad esofágica. Rev. Legal Costa Rica 2016;33(1):1 Disponible en: https://www.scielo.sa.cr/pdf/mlcr/v33n1/2215-5287-ml-cr-33-01-00269.pdf [ Links ]
2. Mendez Sánchez R. Acalasia esofágica. Rev. Med. Sinergia. 2018;3(10):3-6 Disponible en: https://www.medigraphic.com/pdfs/sinergia/rms-2018/rms1810a.pdf [ Links ]
3. Beck WC, Sharp KW. Achalasia. Surg Clin North Am. 2011 Oct;91(5):1031-7. doi: 10.1016/j.suc.2011.06.005. PMID: 21889028. [ Links ]
4. Forero-Vázquez BN, Yopasa-Romero JJ. Diagnostico y manejo actual de la acalasia. Rev. Colomb. Cir. 2023;38(2):330-8. DOI: https://doi.org/10.30944/20117582.2187 [ Links ]
5. Marinello FG, Targarona EM, Balagué C, Monés J, Trías M. Tratamiento quirúrgico de la acalasia: ¿mejor que las dilataciones?. Rev. Med. Gastro. 2009;32(9):653-661 https://doi.org/10.1016/j.gastrohep.2009.02.013 Disponible en: https://www.elsevier.es/es-revista-gastroenterologia-hepatologia-14-articulo-tratamiento-quirurgico-acalasia-mejor-que-S0210570509004002 [ Links ]
6. Roque González R, Martínez Alfonso MA, Torres Peña R, Anido Escobar V, Naranjo Hernández D, Díaz Drake Z. Miotomía de Heller laparoscópica para el tratamiento de la acalasia esofágica en el adulto mayor. Rev Cubana Cir [Internet]. 2015;54(4):309-317 Disponible en: https://www.medigraphic.com/cgi-bin/new/resumen.cgi?IDARTICULO=63971 [ Links ]
7. Cabral D, Reyes R, Mosqueira N, Godoy M. Tratamiento de la acalasia en el Hospital Nacional de Itauguá. Rev Cir Parag 2014;38(2):1-12. Disponible en: http://scielo.iics.una.py/scielo.php?script=sci_arttext&pid=S2307-04202014000200004 [ Links ]
8. Benítez García FD, Ramírez Sotomayor J. Morbimortalidad de la acalasia en el Hospital Nacional de Itauguá en el año 2.013-2.016. Rev. Cir. Parag. [Internet]. 2018;42(3):8-11 https://doi.org/10.18004/sopa-ci.2018.diciembre.8-11 Disponible en: http://scielo.iics.una.py/scielo.php?script=sci_arttext&pid=S2307-04202018000300008 [ Links ]
9. González Paredes GM. Acalasia esofágica: correlación entre la clínica, radiología y estudios fisiológicos [tesis de grado]. España: Departamento de cirugía. Hospital de Mataró Servicio de Cirugía General. Universidad Autónoma de Barcelona; 2011 [ Links ]
10. Montiel-Roa AJ, Rojas-Franco BM, Dragoto-Galvan A, Mora-Garbini SD. manejo quirúrgico de la acalasia esofágica en el Hospital central del IPS durante el periodo enero 2016 a diciembre 2018. Cir. Parag. 2020;44(1):16-18 https://doi.org/10.18004/sopaci.2020.abril.16-18 . Disponible en: http://scielo.iics.una.py/scielo.php?script=sci_arttext&pid=S2307-04202020000100016 [ Links ]
Author’s contribution:
FP: conceptualization, data processing, formal analysis, investigation, methodology, project and resource administration, validation, visualization, writing, revision and editing of the original draft. JFC and TE: conceptualization, methodology, supervision, validation, visualization, writing, revision, and editing. Authors are aware of the final con- tent and authorize its publication.
Conflict of Interest:
Funding:
Ethical considerations:
Received: March 29, 2023; Accepted: November 27, 2023











 texto em
texto em