Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Cirugía paraguaya
versión On-line ISSN 2307-0420
Cir. parag. vol.47 no.3 Asunción dic. 2023
https://doi.org/10.18004/sopaci.2023.diciembre.15
ORIGINAL ARTICLE
Management of patients with appendicular mass, in the general surgery service at the Hospital Nacional de Itauguá in the period 2011-2021
1Hospital Nacional de Itauguá. Itauguá, Paraguay
Introduction: this study seeks to determine the characteristics and management of patients with appendiceal mass at the General Surgery Service at the Hospital Nacional de Itauguá, an infrequent pathology manifested as an inflammatory tumor consisting of the inflamed appen- dix, adjacent viscera and greater omentum when the organism manages to partially control appendicitis, thus avoiding peritonitis. Methods: retrospective, descriptive study, being variables: reason for consultation, days of illness and hospitalization, treatment, etc. Results: of the total of 50 samples, 88% consulted for pain, the average number of days of illness is 9 days and hospitalization 11 days, on physical examination 82% presented a tumor in the right iliac fossa. 56% required surgery: 16 were cavity lavage plus drainage, 1 case right colectomy and 2 cases percutaneous drainage. Conclusion: According to the bibliographies, in recent years a conservative attitude is spreading. In our work, however, immediate surgery was performed in 56% of the cases, we did not verify the use of delayed surgery, probably due to lack of follow-up. Most come with symptoms of approximately 9 days, already as a ruptured abscess in the cavity, so the most used technique was lavage + cavity drainage.
Keywords: aappendiceal mass; acute appendicitis; appendectomy; conservative treatment
Introducción: el plastrón apendicular es una patología infrecuente ma- nifestada como una tumoración inflamatoria constituida por el apén- dice, vísceras adyacentes y epiplón mayor cuando el organismo logra controlar parcialmente la apendicitis, evitando así una peritonitis. Este trabajo busca determinar características y manejo de pacientes con plas- trón apendicular del Servicio de Cirugía general del Hospital Nacional de Itauguá. Métodos: estudio retrospectivo, descriptivo de corte trans- verso. Resultados: del total de 50 pacientes, 88% consultó por dolor, el promedio de días de enfermedad previo de 9 días y una internación pro- medio de 11 días. Al examen físico 82% presentaba tumoración en fosa iliaca derecha. El 56 % requirió cirugía: 16 fueron lavado de cavidad más drenaje (por plastrón roto y abscedado a cavidad), 1 caso colectomía derecha y 2 casos drenajes percutáneos. Conclusión: Probablemente debido al retraso al acceso del sistema de salud, los pacientes al acudir ya presentan complicaciones del plastrón apendicular que requieren un tratamiento quirúrgico en más de la mitad de los casos.
Palabras clave: plastrón apendicular; apendicitis aguda; apendicectomía; tratamiento conservador
INTRODUCTION
Appendiceal mass, infrequent pathology that appears as an acute appendicitis complication: it consist of an inflammatory myo fibroblastic tumor constituted by the swollen appendix, which is generally already punctured, adjacent viscera and greater omentum. It may or may not contain pus (abscess/phlegmon). It occurs when the organism can partially control this process, hence avoiding a peritonitis. Additionally, the infectious process increments morbidity, as well as prolonging the treatment, hospitalization or resting time, tests, etc(1,2).
There are advantages and disadvantages between the choice of medical (conservative) or surgical (whether immediate or de ferred) treatment. Deferred surgical treatment consists of initial conservative treatment followed by a scheduled appendectomy: it entails minimal complications, given that it’s performed in a stable patient, with solved inflammatory symptoms. Further- more, it prevents recurring appendiceal episodes, which are present more frequently between the 6 to 24 following months, also preventing diseases such as Meckel diverticulum, Crohn’s disease or appendiceal neoplasms, and if some of these are al- ready in progress, early detection allows better prognosis hence avoiding the use of more aggressive therapies(2,3).
On immediate surgical treatment a simple drainage (if the appendix is digested), appendectomy, or even a right hemi- colectomy can be performed. A Colombian research of 2,175 acute appendicitis cases reported that a right hemicolectomy was necessary in 1.7% of cases (half of them due to an unspecific inflammatory mass or plastron), with primary anastomosis and a morbidity of 69%. (4) Another surgical option is ileocolic resection, a procedure associated with low morbi-mortality, compared to the right hemicolectomy. (5) Malignant tumors of the appendix, cecum and ascending colon are the main cause of concern when a surgeon finds these inflammatory masses; in these cases a right hemicolectomy with lymph node dissection and primary anastomosis is recommended. (4) The advantages of immediate surgery, although high mass recurrency chance (71%), and high malignant tumor incidence, show a lessened hospitality stay and, therefore lower use of resources, however it presents multiple complications such as other viscera’s injuries, surgical wound’s infection, pelvic abscess and the need of surgical reintervention. Henceforth, this option is not of the first considerations of professionals, choosing the conservative approach to avoid the aforementioned adverse situations. (6,7)
Those who propose the conservative approach only predicate based on the number of patients that develop a subsequent appendicitis and/or appendiceal cancer to be minimum (0.2- 0.5% of the total of gastrointestinal tumors), considering it’s an intervention that increases hospitalizations and unnecessary use of resources. However, it also presents complications as failure, uncomplete drainage or the need of additional drain- ages, infections, fistula, laparotomy for abscess drainage and recurrent appendicitis. (6) Nowadays the use of minimally invasive therapy with percutaneous drainage for the resolution of abdominal build-up and abscessed appendiceal mass is also recommended. Its use will depend on the personnel’s experience and the existence of this resource in the institution, how- ever it also presents limitations as to not being able to achieve an anatomopathological study, therefore being unable to discard malignant pathology(8).
The relevance of this work rests on the lack of national publications about the subject and above all else the fact that nowadays there are many diverse stances on a pathology’s treatment that could eventually present low morbidity and be fatal in cases in which diagnosis nor proper treatment were achieved. The present retrospective research seeks to determine the appendiceal mass patient’s characteristics and handle, within the Adult General Surgery Services in the Hospital Nacional de Itauguá, during 2011 through 2021.
METHODS
50 completed clinical forms were found in the Hospital Nacional de Itauguá, from which we solely focused on the ones that presented an appendiceal mass diagnosis, excluding uncomplete forms. A retrospective, descriptive and observational study was performed, with a cross-sectional non-probability sampling. Our job consists of literary search through virtual libraries about the topic in question, as well as reading, analysis, comprehension, and synthesis of the found literature, and subsequent recollection of data from the forms, respecting the right of privacy and confidentiality of the identity of the patients. Likewise, corresponding authorization was solicited to the information access service’s personnel, and the protocol was accepted by the ethical committee. The studied variables are: age, gender, consultation’s reason, days of hospital stay and sickness, antibiotic therapy, treatment, and complications. For the variable’s study the data was transferred to a Microsoft Office Excel 2007®-type virtual spreadsheet and submitted to statistical observations.
RESULTS
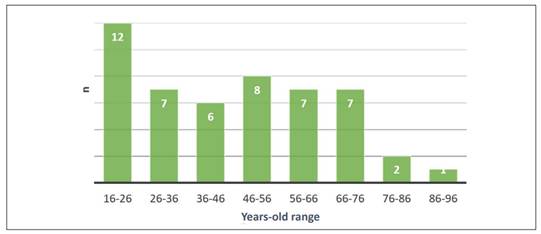
Regarding the sample total (50 patients), 54% of cases were of the female gender and the prevalent age range were between 16 to 26 years old (Graphic 1). 88% of patients consulted because of pain, while the rest did so because of tumors, with an average formation rate of 9.27 days before consultation.
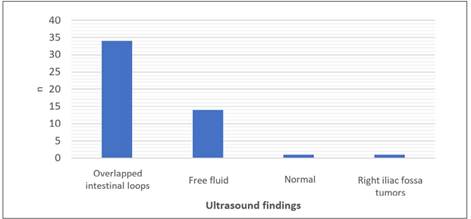
Upon performing the physical exam, it was reported that 82% of patients presented tangible tumors on the right iliac fossa and 64% presented Delbet’s sign during abdominal palpation. Between the most frequent ultrasound findings are the over lapped intestinal loops (68%), free fluid (28%) (See Graphic 2).
Those whom required surgical treatment during hospital stay were 56% of patients, in whom surgical techniques inform that 16 cases had cavity cleaning and draining, with most of them having a generalized postoperative peritonitis diagnosis by broken-cavity abscessed mass, from which a successful appendectomy was only achieved in 8 cases, right colectomy was performed in one case and only an ileostomy plus drainage was performed in one case, minimally invasive was performed in 2 of the cases (percutaneous drainage) (See Table 1). 80% did not present any complications, among mentioned postoperative complications are surgical site infection as first place (14%), and evisceration, fecal fistula in less cases. There was only one de- ceased, caused by sepsis on a senior patient.
The remaining patients received the conservative handle (antibiotic therapy), being ciproflozacin/metronidazole the combination utilized in 98% of cases.
The general average of hospital stay days was 11.
Table 1: Patient classification by treatment: surgical/conservative.
| Treatment Surgical | n | % |
|---|---|---|
| Cleaning plus drainage | 16 | 32% |
| Appendectomy | 8 | 16% |
| Percutaneous drainage | 2 | 4% |
| Ileostomy | 1 | 2% |
| Right colectomy | 1 | 2% |
| TOTAL SURGICAL TREATMENT | 28 | 56% |
| Conservative Treatment | ||
| Antibiotic Therapy | 22 | 44% |
| TOTAL CONSERVATIVE TREATMENT | 22 | 44% |
DISCUSSION
According to the references, a conservative attitude towards appendiceal mass has been extending for the past few years. The presence of a pericecal inflammatory mass of infectious etiology has reached a variable frequency of 2-10% of the appendiceal procedures(9,10).
Nowadays the appendiceal mass treatment options are the deferred surgical alternative, versus the conservative or medical handle, as the most idoneous treatment. On the other hand, the no-less-important immediate surgery option is also presented. There is no consensus regarding which would be the correct option, the resolution is greatly related to the surgeon’s experience, resource availability and the patient’s state. In the last few years a conservative attitude has been extending in non-complicated ways through hydration, broad-spectrum antibiotic therapy and clinical observation, based on the development of imagery techniques with better diagnostic precision, increasing therapeutic efficiency and the concept that a non-complicated appendicitis will not always evolve towards perforation, regardless of showing a near 20% global recurrency of appendicitis symptoms and a small impact on the necessity of a subsequent appendectomy due to therapeutic failure(3,11,12,13).
According to studies, appendectomy have much simple results when performed in between 3-6 months(14). In our research, however, immediate surgical treatment was performed in 56% of cases, without considering deferred surgical use, most likely due to lack of proper follow-up of the patients after discharge, which represents a bias. The vast majority of patients were young, who attended the emergency room reporting 9-month evolutive symptoms, and unlike other researches, the most frequently used surgical technique in our casuistry was abdominal cavity cleaning and drainage. Only 20% presented postoperative complications. The consultation reason and performed surgery is most likely due to most patients already arriving with pre- operative acute abdomen diagnosis and whose intraoperative findings were acute generalized peritonitis by broken-cavity abscessed appendiceal mass, which also explains the fact that one of the most frequent postoperative complications was surgical site infection. We will continue to perform follow-ups to dis- charged patients without surgery, and investigate further about the handling to reach an unanimous and effective conclusion regarding therapeutics.
CONCLUSION
In our research immediate surgery was performed in 56% of cases. We did not consider to the use of deferred surgery, most likely due to lack of patient follow-ups. Most of them report with 9-days symptoms, them being broken-cavity abscess in most cases, therefore cavity cleaning and draining was the most utilized surgical technique. This study is of outmost relevance due to the fact that there is practically no recent national publications about the subject, and as we described during the study, this pathology can be of high impact to the working capability and quality of life of the patient, especially due to handling being mostly conservative, reason why it’s very important to avoid subsequent complications.
REFERENCES
1. Humes DJ, Simpson J. Acute appendicitis. BMJ. 2006 Sep 9; 333(7567): 530-4. doi: 10.1136/bmj.38940.664363.AE. PMID: 16960208; PMCID: PMC1562475. [ Links ]
2. Brainsky A, Salamanca E, Bonilla E, Varón C, Roa JL, Díaz D. Controversias En El Manejo Del plastrón Y El Absceso Apendicular: Reporte De Un Caso. Rev Colomb Cir 2004; 19 : 190-194. [ Links ]
3. Simillis C, Symeonides P, Shorthouse AJ, Tekkis PP. A meta-analysis comparing conservative treatment versus acute appendectomy for complicated appendicitis (abscess or phlegmon). Surgery. 2010 Jun;147(6):818-29. doi: 10.1016/j.surg.2009.11.013. Epub 2010 Feb 10. PMID: 20149402. [ Links ]
4. Beltrán A. Hemicolectomía derecha en pacientes operados por apendicitis: de la incisión de McBurney y apendicectomía, a la laparotomía media y hemicolectomía.. Rev Colomb Cir. 2012; (27): 129-138 [ Links ]
5. Hildebrand P, Kropp M, Stellmacher F, Roblick UJ, Bruch HP, Schwandner O. Surgery for right-sided colonic diverticulitis: results of a 10-year- observation period. Langenbecks Arch Surg. 2007 Mar; 392(2): 143-7. doi: 10.1007/s00423-006-0109-6. Epub 2006 Oct 28. PMID: 17072664 [ Links ]
6. Santos M, Torres V, Poblete A, Guelfand M, Rodríguez J. Tratamiento de los plastrones apendiculares en pediatría. Conservador v/s quirúrgico ¿cuál es la mejor alternativa? Rev. Ped. Elec. [en línea] 2010;7(2):2-7. ISSN 0718-0918 Disponible en: https://www.revistapediatria.cl/volumenes/2010/vol7num2/pdf/PLASTRON.pdf [ Links ]
7. Deelder JD, Richir MC, Schoorl T, Schreurs WH. How to treat an appen- diceal inflammatory mass: operatively or nonoperatively? J Gastrointest Surg. 2014 Apr;18(4):641-5. doi: 10.1007/s11605-014-2460-1. Epub 2014 Feb 4. PMID: 24493295. [ Links ]
8. Escudero Sepúlveda AF, Roccuzzo, Medina Pereira JP, Vicente Rodrí- guez AN, Fonseca Consuegra AS. Manejo percutáneo de la apendicitis aguda complicada. Reporte de caso y revisión de la literatura. SACD Rev [internet]. 2020;1(3):e1507:016 Disponible en: http://revista.sacd.org.ar/manejo-percutaneo-de-la-apendicitis-aguda-complicada-reporte-de- caso-y-revision-de-la-literatura/ [ Links ]
9. Meshikhes AW. Management of appendiceal mass: controversial issues revisited. J Gastrointest Surg. 2008 Apr;12(4):767-75. doi: 10.1007/ s11605-007-0399-1. Epub 2007 Nov 13. PMID: 17999120. [ Links ]
10. Cheng Y, Xiong X, Lu J, Wu S, Zhou R, Cheng N. Early versus delayed appendicectomy for appendiceal phlegmon or abscess. Cochrane Database Syst Rev. 2017 Jun 2;6(6):CD011670. doi: 10.1002/14651858. CD011670.pub2. PMID: 28574593; PMCID: PMC6481778. [ Links ]
11. Allievi N, Harbi A, Ceresoli M, Montori G, Poiasina E, Coccolini F, Pisano M, Ansaloni L. Acute Appendicitis: Still a Surgical Disease? Results from a Propensity Score-Based Outcome Analysis of Conservative Versus Surgical Management from a Prospective Database. World J Surg. 2017 Nov; 41 (11): 2697-2705. doi: 10.1007/s00268-017-4094-4. PMID: 28623597 [ Links ]
12. Helling TS, Soltys DF, Seals S. Operative versus non-operative management in the care of patients with complicated appendicitis. Am J Surg. 2017 Dec;214(6):1195-1200. doi: 10.1016/j.amjsurg.2017.07.039. Epub 2017 Sep 18. PMID: 28941724. [ Links ]
13. Rollins KE, Varadhan KK, Neal KR, Lobo DN. Antibiotics Versus Appendicectomy for the Treatment of Uncomplicated Acute Appendicitis: An Updated Meta-Analysis of Randomised Controlled Trials. World Journal of urgery. 2016 Oct;40(10):2305-2318. DOI: 10.1007/s00268- 016-3561-7. PMID: 27199000. [ Links ]
14. Villalón F, Villanueva A, Suñol MA, Garay J, Arana J, Jimênez J, Sainz de la Maza M, Eizaguirre I. Tratamiento y seguimiento del plastrón apendi- cular. Cir Pediatr. 2013 Oct; 26 (4): 164-6. PMID: 24645240. [ Links ]
Author’s contributions:
All authors have contributed to the development of the manuscript, literary, referential and statistical search, writing of the article and final approval.
Conflict of interest:
Funding:
Ethical considerations:
Received: March 15, 2023; Accepted: November 19, 2023











 texto en
texto en