Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Cirugía paraguaya
On-line version ISSN 2307-0420
Cir. parag. vol.47 no.2 Asunción Aug. 2023
https://doi.org/10.18004/sopaci.2023.agosto.42
Case report
Left renal vein transposition
1Hospital Central del Instituto de Previsión Social. Asunción, Paraguay
Nutcracker syndrome caused by aorto-mesenteric compression of the left renal vein can be treated with surgical transposition. A review of this treatment was carried out at the Instituto de Previsión Social. Two women aged fifteen and twenty-six, who had low back pain and hematuria, were identified. They were discharged on the fourth and fifth postoperative day. The patients showed no symptoms after five and nine months of follow-up.
Keywords: Nutcracker Syndrome; Left renal vein transposition.
El Síndrome de Nutcracker producido por compresión aorto-mesenterica de la vena renal izquierda puede tratarse con transposición quirúrgica. Se realizó revisión de dicho tratamiento realizado en el Instituto de Previsión Social. Se identificaron dos mujeres de 15 y 26 años, que presentaron dolor lumbar y hematuria. Egresaron al cuarto y quinto día de postoperatorio. Las pacientes no presentaron síntomas a los cinco y nueve meses de seguimiento.
Palabras claves: Síndrome de Nutcracker; Transposición de vena renal izquierda.
INTRODUCTION
The compression of the left renal vein by the aorto-mesenteric angle (aorta and superior mesenteric artery) was first described by Grant in 1937, who drew an analogy with a nutcracker1. The first clinical report of a patient with left renal vein compression syndrome, also known as nutcracker syndrome (NS), was made in 1950. The syndrome was described in a thin-built patient with little retroperitoneal fat, resulting in left renal ptosis with subsequent compression of the left renal vein2.
The pathophysiology of NS involves venous hypertension proximal to the site of compression of the left renal vein, leading to the development of varices in the renal pelvis that cause hematuria and left lumbar pain. Hematuria occurs due to the rupture of veins into the urinary collecting system. Other symptoms secondary to venous hypertension include varicocele in males, pelvic congestion syndrome in females, and orthostatic proteinuria3-5.
Numerous therapeutic procedures exist for treating these patients. Open surgical procedures include nephropexy, gonadal venous bypass, renal decapsulation, mesoaortic transposition, renal autotransplantation, and left renal vein transposition. Endovascular procedures used for treatment include transluminal angioplasty and stent placement in the left renal vein6-8.
The purpose of this study is to report the outcomes of patients with severe NS symptoms refractory to medical treatment who were treated in a Vascular Surgery Department.
CLINICAL CASE PRESENTATION
Data were collected from patients diagnosed with NS and treated in the Vascular Surgery Department of the Central Hospital of the Instituto de Previsión Social (HC-IPS) during the period from January 1st to December 31st, 2022. The HC-IPS electronic system (SIH) was used to collect data, including sex, age, laboratory tests, imaging studies (ultrasound, angioCT), urological studies (cystoscopy and ureteroscopy), surgical procedure performed (operative time, intraoperative bleeding, surgical technique, renal vein clamping time, length of hospital stay, and complications). Follow-up was conducted through reviewing patient records in the electronic system and telephone calls.
Patients underwent clinical evaluation, complemented with abdominal ultrasound in cases of abdominal pain, followed by abdominal angiotomography using a 64-slice multidetector CT scanner and Maximum Intensity Projection (MIP) reconstruction with arterial and venous phases for better identification of renal veins. Hematuria was assessed using cystoscopy and ureteroscopy.
The surgical procedure used was left renal vein transposition (Figure 1). General anesthesia was administered for the procedure. A midline laparotomy incision was made, and access to the inferior vena cava (IVC) and left renal vein was obtained transperitoneally by incising the retroperitoneum to the left of the root of the mesentery. Systemic heparinization with unfractionated heparin at a dose of 100 IU per kilogram of the patient's weight was administered before renal vein clamping. Clamping of the left renal vein and partial clamping of the IVC were performed. The IVC was sutured with 6/0 polypropylene. To mobilize the left renal vein, the left suprarenal vein was ligated, and the left gonadal vein was ligated only if necessary. The anastomosis of the left renal vein was performed 3 cm below its ostium.
Two patients with left renal vein compression syndrome or NS were identified between January 1st and December 31st, 2022.
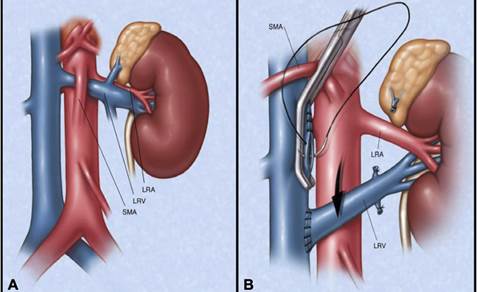
Figure 1. Aorto-mesenteric compression. Panel A: Compression of the left renal vein by the superior mesenteric artery. Panel B: Surgical schema of left renal vein transposition. LRA: Left renal artery, LRV: Left renal vein, SMA: Superior mesenteric artery. Reprint with permission from J Vasc Surg 2009;49: 386-94.
Case 1 involved a 15-year-old female patient with a prior clinical history of severe abdominal pain. The patient was referred to HC-IPS with a probable diagnosis of left kidney stones, where abdominal ultrasound was performed after clinical evaluation. The ultrasound ruled out kidney stones as the cause of the pain and showed Doppler signs of possible compression of the left renal vein. Abdominal angiotomography (Figure 2) was performed, confirming compression of the left renal vein by the aorto-mesenteric angle during the venous phase. Left renal vein transposition (LRVT) was performed without complications (Figure 3). Surgical time: 130 minutes, left renal vein clamping time: 25 minutes. The patient was discharged on the fifth postoperative day without abdominal pain. Abdominal Doppler was performed on the ninth postoperative day, confirming a patent left renal vein with normal flow (Figure 4). The patient remained symptom-free at 9 months of follow-up.
Case 2 involved a 26-year-old female patient who presented to HC-IPS with severe hematuria without hemodynamic impact, but requiring transfusion of 4 units of packed red blood cells. Studies were conducted to determine the cause of the hematuria. Cystoscopy revealed abundant clots without identifying the cause. Ureteroscopy did not reveal the source of bleeding. Ultrasound revealed a staghorn calculus in the left kidney. Given the suspicion of NS, abdominal angiotomography was performed, confirming left renal vein compression by the aorto-mesenteric angle (Figure 5). The patient underwent LRVT, with a surgical time of 140 minutes and a left renal vein clamping time of 28 minutes (Figure 6). No postoperative hematuria was observed. The patient was discharged on the fourth postoperative day without complications. Follow-up revealed no recurrence of hematuria, and renal function was preserved at 6 months.
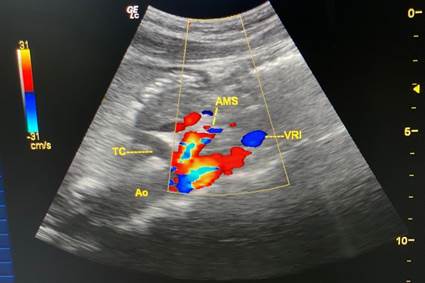
Figure 4. Abdominal Doppler. Patent left renal vein. LRV: Left renal vein, SMA: Superior mesenteric artery, Ao: Aorta.
DISCUSSION
The diagnosis of NS is challenging due to the lack of absolute criteria. Patient evaluation should be comprehensive and multidisciplinary. The most common reasons for consultation are left lumbar pain, hematuria, and varicocele. NS typically presents in patients with a thin constitution and low body mass index (less than 25). Diagnosis is based on clinical findings, confirmed by ultrasound showing left renal vein compression, and further supported by abdominal angiotomography with arterial and venous phases and Maximum Intensity Projection reconstruction.9-12
Medical treatment is applied in cases with mild to moderate symptoms. Surgical treatment is indicated for severe cases unresponsive to medical therapy. According to the Argentine Intersociety Consensus on Pelvic Syndrome, medical treatment is recommended for at least twenty-four months in individuals under 18 years old and six months in those over 18 years, focusing on increasing body mass index.13-14
Endovascular treatment options include angioplasty and stent placement in the left renal vein, with reported technical success rates of up to 95%.13-14
Among the surgical options, left renal vein transposition (LRVT) is considered the best choice as it ensures renal function with a direct anastomosis to the inferior vena cava, ensuring a high patency rate. Reviewed literature indicates the best results in cases of hematuria and abdominal pain, with higher recurrence rates observed in cases of varicocele. Renal autotransplantation is a more complex surgery compared to LRVT.
REFERENCES
1. Reed Nr, Kalra M, Bower TC, Vrtiska TJ, et al. Left renal vein transposition for nutcracker syndrome. J Vasc Surg 2009;49: 386-94. [ Links ]
2. Boileau Grant JC. A method of anatomy, descriptive and deductive. 3ra ed. Baltimore: The Williams and Wilkins Company; 1944. [ Links ]
3. El-Sadr AR, Mina E. Anatomical and surgical aspects in the operative management of varicocele. Urol Cutaneous Rev. May 1950; 54:257-62. [ Links ]
4. Chait A MK, Fabian CE, Mellins HZ. Vascular impressions on the ureters. Am J Roentgen Rad Ther 1971; 3:729-49. [ Links ]
5. Stavros AT, Sickler KJ, Menter RR. Color duplex sonography of the nutcracker syndrome (aortomesenteric left renal vein compression). J Ultrasound Med 1994; 13:569-74. [ Links ]
6. Taylor HC. Vascular congestion and hyperemia; their effects on structure and function in the female reproductive system. Am J Obstet Gynecol 1949; 57:637-53. [ Links ]
7. Paolini JE. Síndrome congestivo pélvico: tratamiento quirúrgico. En: Ulloa JH, Simkin C, Segura J, et al (eds). Guías latinoamericanas de terapeútica para la patología venosa. Buenos Aires: Edit. Nayarit; 2016. p.299-303. ISBN 978-987-28471. [ Links ]
8. Kornberg AM, Turek MA, Sanchez F, Eiselle G. Diagnóstico y tratamiento de venopatías pélvicas. Síndrome de congestión pélvica. Várices vulvares. Rev Forum de Flebología y Linfología. mayo 2006;8(1):1 [ Links ]
9. Almeida EC, Nogueira AA, Candido dos Reis FJ, Rosa e Silva JC. Cesarean section as a cause of chronic pelvic pain. Int J Gynaecol Obstet 2002;79(2):101-4. [ Links ]
10. Hebbar S, Chawla C. Role of laparoscopy in evaluation of chronic pelvic pain. J Minim Access Surg 2005;1(3):116-2. [ Links ]
11. Howard FM. The role of laparoscopy in chronic pelvic pain: promise and pitfalls. Obstet Gynecol Surv1993;48(6):357-87. [ Links ]
12. Marsh P, Holdstock J, Harrison C, Smith C, Price BA, Whiteley MS. Pelvic vein reflux in female patients with varicose veins: comparison of incidence between a specialist private vein clinic and the vascular department of a National Health Service District General Hospital. Phlebology 2009;24(3):108-13. [ Links ]
13. Eisele G et al. Intersocietary Argentine pelvic congestion syndrome consensus. Part 1. Rev Argent de Cardioangiologia Intervencionista 2020;11(4):162-193. https://doi.org/10.30567/RACI/202004/0162 [ Links ]
14. Amore M, et al. Intersocietary Argentine pelvic congestion syndrome consensus. Part 2. Rev Argent de Cardioangiologia Intervencionista 2021;12(1): 14-43. https://doi.org/10.30567/RACI/202101/0014 [ Links ]
9Ethical Considerations: This research complies with the principles of the Nuremberg Code and the Declaration of Helsinki.
Received: April 04, 2023; Accepted: July 20, 2023











 text in
text in