Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Cirugía paraguaya
On-line version ISSN 2307-0420
Cir. parag. vol.47 no.2 Asunción Aug. 2023
https://doi.org/10.18004/sopaci.2023.agosto.28
Review article
Health care-associated infections after surgical procedures in adult patients: scoping review
1Universidad Surcolombiana, Neiva, Colombia.
2Hospital Universitario Hernando Moncaleano Perdomo, Neiva, Colombia.
Objective: To establish the infections associated with health care in surgically treated patients, without considering operative site (ISO) infections. Materials and methods: A search of the literature was performed in MEDLINE, CENTRAL, LILACS databases in addition to unpublished literature, identifying studies related to infections associated with health care in adult patients who underwent surgery. Results: In the search performed, 25 articles were selected, from which the results were extracted. The most frequent IAAS in the studies reviewed were: ventilator-associated pneumonia (36%), pneumonia associated with health care (32%), urinary tract infections by urinary catheter (48%), infections associated with venous catheter (8 %). Conclusion: Infections associated with health care in patients brought to surgical procedures, most frequently found are ventilator-associated pneumonia, pneumonia associated with health care, urinary tract infection by catheter and venous catheter-associated infections. However, they continue to generate questions, since ISO is the most documented, suggesting more studies and research.
Key words: Infection associated with health care; nosocomial infection; postoperative infections; surgical procedures
Objetivo: Establecer las infecciones asociadas a la atención de la salud en pacientes intervenidos quirúrgicamente, sin tener en cuenta las infecciones del sitio operatorio (ISO). Materiales y métodos: Se realizó una búsqueda de la literatura en las bases de datos de MEDLINE, CENTRAL, LILACS además de la literatura gris, para identificar estudios relacionados con infecciones asociadas a la atención de la salud en pacientes adultos que fueron intervenidos quirúrgicamente. Resultados: En la búsqueda realizada se seleccionaron 25 artículos de los cuales se extrajeron los resultados. Las IAAS más frecuentes en los estudios revisados fueron: neumonía asociada al ventilador (36%), neumonía asociada al cuidado de la salud (32%), infecciones de tracto urinario por catéter urinario (48%), infecciones asociadas a catéter venoso (8%). Conclusión: Las infecciones asociadas a la atención de la salud frecuentemente encontradas en pacientes llevados a procedimientos quirúrgicos son la neumonía asociada al ventilador, neumonía asociada al cuidado de la salud, la infección del tracto urinario por catéter y las infecciones asociadas a catéter venoso, sin embargo, las infecciones de sitio operatorio (ISO) son las más documentadas, situación que requiere mayor atención y abordaje a través de otros estudios de investigación.
Palabras clave: Infección asociada a la atención en salud; Infección nosocomial; infecciones posquirúrgicas; procedimientos quirúrgicos.
INTRODUCTION
Healthcare-associated infection (HAI), previously known as nosocomial or intrahospital infection, is defined as an infection that arises from the process of medical or surgical care not inherent to the reason for admission to the hospital, without prior symptoms or during the incubation period of the disease1-6.
HAIs are a global public health problem, as indicated by the World Health Organization (WHO) in 2002, which published a study involving 55 hospitals from 14 countries, reporting an average of 8.7% HAIs in hospitalized patients, corresponding to over 1.4 million individuals (3.5). This is reinforced by data from the Centers for Disease Control and Prevention (CDC) in the US, which documents approximately 1.7 million people with HAIs and an annual mortality rate of around 99,000 individuals3; it also estimates that the cost of HAIs in the year 2000 was $6 billion (6.7). In a study in the United Kingdom (UK), a general HAI rate of 7.8% was found in 4,000 patients, leading to an 11-day extension in hospital stay, with costs 2.8 times higher than those of comparable non-infected patients. Additionally, the mortality rate of the infected group was 13%, compared to 2% in the non-infected group (1.8).
In 2010, The Lancet compiled 220 publications from 1995 to 2008, including studies from the Americas (22%), Europe (20%), Southeast Asia (16%), Eastern Mediterranean (8%), Africa (5%), and other regions (29%). The study revealed that the prevalence of HAIs in developing countries was 15.5 per 100 patients, which could increase to 34.2 per 1,000 patient-days in ICU patients, tripling the rates reported in the US9.
In Colombia, the National Epidemiological Surveillance Group of Intensive Care Units (GRUVECO) reported a ventilator-associated pneumonia (VAP) rate of 7.37 per 1,000 ventilator days, a catheter-associated bloodstream infection (CAB) rate of 1.77 per 1,000 catheter days, and a urinary tract infection associated with urinary catheterization (UTIAC) rate of 3.04 per 1,000 urinary catheter days4. In 2012, surveillance of HAIs was implemented, prioritizing information on Device-Associated Infections (DAI). In Bogotá, a total of 13,762 cases of HAIs were reported in hospital and outpatient services1,2,4.
Regarding the classification of HAIs, there are four types associated with invasive and surgical procedures: urinary tract infection associated with urinary catheter, aspiration pneumonia, catheter-associated bloodstream infection, and surgical site infections (SSIs). Some studies have identified risk factors for HAIs related to the host (prematurity, age > 65, immunodeficiency, nutritional status), the agent (predominantly gram-negative bacilli and gram-positive cocci, bacterial resistance), and the hospital environment of the patient (more common in ICUs and operating rooms)3,5.
Given the existing literature on HAIs in surgical patients, there is greater emphasis on SSIs, with limited information regarding other types of HAIs in this population. Hence, the importance of conducting a review focused on healthcare-associated infections other than SSIs, such as urinary tract infection associated with urinary catheterization, catheter-associated bloodstream infection, and healthcare-associated pneumonia. These infections increase the risk of functional disability, prolong hospital stays, reduce the quality of life, and in some cases increase patient mortality, leading to an exaggerated increase in healthcare costs1,2,5,6,8.
The objective of this review is to identify healthcare-associated infections in patients who have undergone surgical procedures, excluding SSIs.
MATERIALS AND METHODS
Search Strategy
The search was conducted by three researchers using the following databases: MEDLINE, CENTRAL, and LILACS, with language restriction (English and Spanish) and without time restrictions. A combination of MeSH terms and free-text terms was used for the search, including:
MEDLINE: Infectious Disease Transmission, Professional-to-Patient"[Mesh] OR "Cross Infection"[Mesh]) AND "surgery"[Subheading] NOT "Surgical Wound Infection"[Mesh] con filtro: Humanos; idioma inglés - spanish
CENTRAL: #1 Infectious Disease Transmission, Professional-to-Patient [Mesh] OR #2 Cross Infection [Mesh] AND #3 surgery NOT #4 Surgical Wound Infection [Mesh]
LILACS: (tw:(infección hospitalaria)) AND (tw:(procedimientos quirúrgicos operativos)) NOT (tw:(infección de la herida quirúrgica)) AND (instance:"regional") AND ( db:("LILACS") AND la:("es"))
DECS: Infección Hospitalaria, Procedimientos Quirúrgicos Operativos; Infección Herida Quirúrgica.
Selection Criteria
According to the design, cohort studies, case series, cross-sectional studies, and systematic reviews that determined cases of HAIs in post-surgical patients were included. Editorials, letters to the editor, comments, studies with samples of fewer than 10 infected patients, studies in pediatric populations, outpatient surgeries, and studies where differentiation between infection and colonization was not achieved were excluded.
To include all relevant research, references from the included studies and a search of the INICC database were reviewed, resulting in 208 publications, of which 3 articles were reviewed. For the identified abstracts, the corresponding authors were contacted to inquire whether the final work had been published in a scientific journal. Additionally, the data obtained from the search in "Infection Control & Hospital Epidemiology" yielded 774 files, from which 11 were chosen based on their titles, but the total was excluded due to being letters to the editor and comments.
The principal investigator (MFE) along with LCH and DMA independently reviewed the titles and abstracts to assess eligibility criteria (N=1287). Once the titles were reviewed, the inter-rater agreement was 87.5%; differences in articles were resolved through discussion and consensus among the three reviewers.
After reviewing titles and abstracts, full-text articles (n=145) were reviewed to assess eligibility criteria. This review was conducted by MFE.
Study Selection
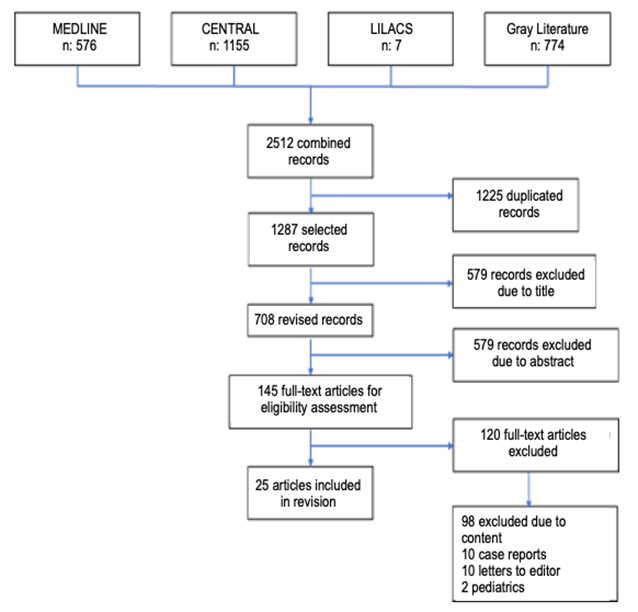
The database search yielded 1287 publications. After removing duplicates, 579 publications were excluded based on their titles. A total of 708 were selected for review of their titles and abstracts. Among these, 563 were excluded based on abstracts, resulting in 145 studies for full-text review. Finally, 25 articles met the eligibility criteria for the review (Figure 1).
Data Extraction
Information from the articles was extracted by three reviewers (MFE, LCH, DMA) using an established format that included the following variables: primary author, year of publication, geographic location, study type, number of participants, type of surgical procedures, and primary outcome.
RESULTS
The search yielded 1287 records, after eliminating duplicates. Among these, 579 records were excluded based on titles, resulting in 708 studies that were reviewed based on abstracts. Among these, 563 were further excluded, resulting in a final pool of 145 studies for full-text review. Out of these, 120 articles were eliminated for not meeting the selection criteria, including being letters to the editor, case reports, studies in pediatric populations, or having content not aligned with the study's objective.
Out of the total studies identified, 25 focused on healthcare-associated infections in post-surgical patients10-34. Specifically, 8 studies examined infections secondary to orthopedic and traumatology procedures(13, 14, 19, 21, 28, 29, 32, 33), 5 focused on cardiovascular surgery11,16,26,31,34, 5 on procedures in oncology patients10,15,18,20,30, 5 on gastrointestinal surgery17,22,23,25,27, and 2 on neurosurgical procedures12,24.
The studies were published between 1996 and 2017 and were conducted in various countries, including the United States(11-15, 17, 18, 21, 22, 24, 27, 29, 33), Canada(25), the United Kingdom(28,30), the Netherlands(10), Switzerland(16), Sweden(19), Spain26,32,34, Israel(20), Mexico(23), and Slovenia(31). All the studies were written in English. The characteristics of the included studies are presented in Table 1.
Table 1. Characteristics of Included Studies in the Review
| Author, year (country) | Study type | # of participants | Type of surgical procedure | Principal outcome |
|---|---|---|---|---|
| Pieter C. van der Sluis(10), 2014 (Netherlands) | Retro-prospective cohort | 185 | Esophagectomy due to cancer | 70 (37.8%) hospitalization related pneumonia - total |
| 9 (4.9%) ICU inmediate postoperative pneumonia | ||||
| 67 (36.2%) pneumonia during hospital stay | ||||
| Raymond J. Strobel(11), 2016 (USA) | Retrospective | 16084 | Coronary bypass graft | 531 (3,3%) pneumonia |
| Branko Skovrlj(12), 2014 (USA) | Retrospective | 2569043 | Spnial surgery | 20867 (0.11%) C. Difficile infection |
| Michael Mackowski(13), 2014 (USA) | Retrospective | 25 | Damage control surgery (thoracotomy/sternotomy) | 12 (48%) VAP |
| 1 (4%) urinary tract infection due to urinary catheter | ||||
| Shu-Chen Kung(14), 2017 (USA) | Retrospective | 93 | Major trauma | 15 (16.1%) had VAP |
| 1 (1.07%) presented urinary tract infection due to urinary catheter | ||||
| Jesse Sammon(15), 2013 (USA) | Retrospective | 2502686 | Oncological Surgery: Colectomy, Cystectomy, Esophagogastrectom, Gastrectomy, Hysterectomy, Pneumonectomy, Pancreatectomy, Prostatectomy | 4.2% urinary tract infection due to urinary catheter |
| 3.5% VAP | ||||
| Philipp Kohler(16), 2015 (Switzerland) | Retrospective | 3706 | Open heart surgery | 10 (0.26%) M. Chimaera infection |
| Christopher T. Aquina(17), 2016 (USA) | Retrospective cohort | 150878 | Segmental colectomy, proctectomy | 3323 (2.2%) C. difficile infection |
| Amit Kochhar(18), 2013 (USA) | Cross-sectional study | 123662 | Oncologic surgery of the oral, laryngeal, hypopharyngeal, or oropharyngeal cavity | 852 presented complications associated with surgery |
| Pneumonia 27.1% | ||||
| Urinary tract infection 12.7% | ||||
| Marie Stenlund(19), 2017 (Sweden) | Retrospective | 4961 | Emergency abdominal surgery / trauma | 90 healthcare-associated pneumonia |
| Evgeni Brotfain(20), 2017 (Israel) | Retrospective | 149 | Oncologic surgery of the upper gastrointestinal tract | 49 patients had postoperative intra-abdominal infection, of which 10 had fungal invasion |
| Robert D. Becher(21), 2011 (USA) | Retrospective | 116 | 72 patients in trauma ICU (TICU) | TICU: VAP 83.3%, healthcare-associated pneumonia 16.7% |
| 44 patients in general surgery ICU (SICU) | SICU: VAP 70.5%, healthcare-associated pneumonia 29.5% | |||
| John G. Armstrong(22), 2017 (USA) | Retrospective | 10108 | Colectomy 7615 | Colectomy: urinary tract infection 107 (1.4%), pneumonia 171 (2.24%) |
| Abdominal perineal resection (APR) 2493 | APR: urinary tract infection 88 (3.6%), pneumonia 60 (2.4%) | |||
| Gerardo Evaristo-Méndez(23), 2016 (Mexico) | Cross-sectional analytical | 942 | 700 general surgery 242 oncologic surgery | General surgery: 9.2% of patients developed pneumonia Oncologic surgery: 10.7% of patients developed pneumonia |
| K. Nosova(24), 2013 (USA) | Retrospective | 46344 | Craniotomy for meningioma | Men: 553 (3.9%) with urinary tract infection |
| Women: 2024 (6.3%) with urinary tract infection | ||||
| Torchia MG(25), 2000 (Canada) | Retrospective | 154 | Colorectal surgery | The overall rate of HAI was 17%, which was higher in patients receiving any type of transfusion, primarily pneumonia |
| M. Henar Rebollo(26), 1996 (Spain) | Case-control study | 970 | Cardiovascular surgery | Nosocomial infection occurred in 89 (9.2%) patients: |
| SSI was the most common (5.6%) | ||||
| Pneumonia (3.2%) | ||||
| Urinary tract infection (1.8%) | ||||
| Deep SSI (0.9%) | ||||
| Bacteremia (0.7%). | ||||
| Courtney Balentine(27), 2009 (USA) | Retrospective | 88 | Major abdominal surgery | VAP 30% Urinary tract infection 20% |
| P. Sharma(28), 2003 (UK) | Prospective observational | 239 | Hip fracture surgery | 17 patients presented diarrhea associated with Clostridium difficile infection |
| Heidi Wald(29), 2005 (USA) | Retrospective cohort | 111330 | Hip fracture surgery | 15.9% of the patients presented urinary tract infection |
| David J. Bowrey(30), 2007 (UK) | Prospective observational | 98 | Esophagectomy due to cancer | 1 out of 5 patients presented MRSA* infection, with a higher risk in those who received neoadjuvant chemotherapy |
| Bojana Beovic(31), 2003 (Slovenia) | Prospective cohort | 2458 | Vascular surgery | Lower respiratory tract infection: 228 pts Urinary tract infection: 48 pts Central nervous system infection: 47 pts Infection from vascular catheter: 19 pts |
| Mónica Izuel Rami(32), 2008 (Spain) | Prospective observational | 286 | Hip fracture surgery | 25.9% presented nosocomial Infections: 36 patients with urinary tract infection 12 patients with respiratory infection 4 patients with urinary tract infection + nosocomial infection 2 patients with urinary tract infection + respiratory infection |
| Hosam K. Kamel(33), 2005 (USA) | Retrospective observational | 138 | Hip fracture surgery | Urinary tract infection in patients older than 65 years was 16% Urinary tract infection in patients younger than 65 years was 4% |
| Emilio Bouza(34), 2003 (Spain) | Prospective observational | 356 | Cardiac surgery | VAP 7.87% |
*SARM: Staphylococcus aureus resistente a la meticilina, VAP: ventilator associated pneumonia, SSI: surgical site infection, ICU: intensive care unit.
Regarding the study design, one-third of these studies were retrospective, with the majority being observational. Only one of the reviewed articles included a case-control design, and two studies were cohort studies. In terms of the surgical procedures performed, one-third of the studies were related to major orthopedic and trauma surgeries, followed by cardiovascular surgeries and gastrointestinal procedures.
The HAIs identified based on the results are as follows: VAP was reported in 6 studies (24%) 13-15,21,27,34, Healthcare-associated pneumonia in 11 studies (44%) 10,11,18,19,21-23,25,26,31,32, Urinary tract infections due to urinary catheter use in 12 studies (48%) (13-15,18,22,24,26,27,29,31-33), Infections associated with venous catheters in four studies (16%) 16,26,30,31, Clostridium difficile infection in three studies (12%) (12,17,28), Intra-abdominal fungal infections in one study (4%) (20) and Infections caused by MRSA were examined in one study (4%) (30).
DISCUSSION
Given that HAIs are one of the main patient safety issues and are considered preventable adverse events, they can be considered some of the best indicators of the quality of care. They are significant due to their frequency, associated morbidity and mortality, increased costs, and reflection of healthcare team actions that can be modified according to current standards35.
In contrast to the literature, which often emphasizes urinary tract infections associated with urinary catheter use as the most common HAIs, the results of this review revealed that healthcare-associated infections in patients undergoing surgical procedures (excluding SSIs, the most documented HAI) are predominantly lower respiratory tract infections, specifically VAP13-15,21,27,34. These are followed by urinary tract infections secondary to the use of urinary catheters13-15,18,22,24,26,27,29,31-33, infections associated with venous catheters16,26,30,31, and less frequently other types of infections [Clostridium difficile12,17,28, fungal infections(20), MRSA infections(30)].
Literature findings indicate that urinary tract infections are the most common HAIs. It is estimated that 80% of these infections are caused by the use of indwelling urinary catheters35. While urinary tract infections cause less morbidity than other HAIs, they can still lead to bacteremia and death. It is estimated that after the second day of catheterization, the risk of bacteriuria increases by 5-10% per day. In many cases, bacteriuria is asymptomatic, and catheter removal is more effective for control than antibiotic administration35.
On the other hand, VAP not only leads to higher morbidity and mortality but also contributes to inappropriate antibiotic use, which in turn contributes to bacterial resistance, increased toxicity, and higher healthcare costs35. According to the results of the reviewed articles, VAP occurrence is dependent on patient-related factors, often seen in patients undergoing oncological procedures with multiple comorbidities, immunocompromised status, and major surgeries such as polytrauma cases, damage control procedures, and significant bleeding, requiring prolonged endotracheal intubation.
Regarding bacteremia, the primary risk factors for its development are catheterization duration, aseptic insertion practices, and ongoing catheter care35. In comparison with the findings of this review, it appears that the occurrence of bacteremia is primarily dependent on operator-related factors and direct transmission.
Of the studies selected for this review based on the inclusion and exclusion criteria, the majority were conducted in North America (52%)11-15,17,18,21,22,24,25,27,29,33, followed by European countries (36%)10,16,19,26,28,30-32,34, with only one study from Asia20 and one from Central America23. It is noteworthy that no studies from South America were found, limiting the extrapolation of findings to this part of the continent. The lack of data likely limits the scope of the analysis.
Reflecting on the implications of these results, it is clear that more studies are needed, with a focus on HAIs, particularly in developing countries like those in Latin America. The absence of such studies in certain regions might be attributed to underreporting due to legal implications of HAIs in those countries, as these can have significant implications for their healthcare systems. This emphasizes the need for further research to identify gaps and needs.
HAIs in patients undergoing surgical procedures continue to raise questions, particularly those that are not SSIs. More research is required, especially in developing countries, to anticipate and recognize the complications that can arise from these infections. These complications include prolonged hospital stays, increased healthcare costs, and increased morbidity and mortality.
REFERENCES
1. Ministerio de Salud. Detectar, prevenir y reducir infecciones asociadas con la atención en salud [Internet]. Disponible en: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/DE/CA/Detectar-Infecciones.pdf [ Links ]
2. SUPERSALUD. CIRCULAR 45 DE 2012 [Internet]. 2012. Disponible en: https://docs.supersalud.gov.co/PortalWeb/Juridica/OtraNormativa/C_MSPS_0045_2012.pdf [ Links ]
3. Unahalekhaka A. Conceptos básicos de control de infecciones. Epidemiología de las infecciones asociadas a la atención en salud. 29-44. [Internet] Disponible en: https://www.theific.org/wp-content/uploads/2014/08/Spanish_ch3_PRESS.pdf [ Links ]
4. Molina F, Fonseca N, Jaramillo C, Mejía S, Arango J, Benitez F, et al. Epidemiología de las infecciones nosocomiales asociadas a dispositivos en 35 unidades de cuidados intensivos de Colombia (2007-2008). Acta Colomb Cuid Intensivo. 2009;9:923-. [ Links ]
5. Girard R, Perraud M, Herriot HE, Prüss A, Savey A, Tikhomirov E, et al. Prevención de las infecciones nosocomiales. Guía Práctica. Organización Mundial de la Salud (2003). [Internet] Disponible en: http://apps.who.int/iris/bitstream/handle/10665/67877/WHO_CDS_CSR_EPH_2002.12_spa.pdf;jsessionid=88B1174085CE6F9B9B4CE39A98FA7171?sequence=1 . [ Links ]
6. Rodríguez-Acelas AL, de Abreu Almeida M, Engelman B, Cañon-Montañez W. Risk factors for health care-associated infection in hospitalized adults: Systematic review and meta-analysis. Am J Infect Control. diciembre de 2017;45(12):e149-56. [ Links ]
7. Cecchini E, Gonzalez S.. Infectologia y enfermedades infecciosas [Internet]. 1.a ed. Ediciones Journal; 2008. Disponible en: http://www.inicc.org/media/docs/Cecchini-Infectologiayenfermedadesinfecciosas.pdf [ Links ]
8. Stone PW, Braccia D, Larson E. Systematic review of economic analyses of health care-associated infections. Am J Infect Control. noviembre de 2005;33(9):501-9. [ Links ]
9. Rosenthal VD. Health-care-associated infections in developing countries. The Lancet. enero de 2011;377(9761):186-8. [ Links ]
10. van der Sluis PC, Verhage RJJ, van der Horst S, van der Wal WM, Ruurda JP, van Hillegersberg R. A new clinical scoring system to define pneumonia following esophagectomy for cancer. Dig Surg. 2014;31(2):108-16. [ Links ]
11. Strobel RJ, Liang Q, Zhang M, Wu X, Rogers MAM, Theurer PF, et al. A Preoperative Risk Model for Postoperative Pneumonia After Coronary Artery Bypass Grafting. Ann Thorac Surg. octubre de 2016;102(4):1213-9. [ Links ]
12. Skovrlj B, Guzman JZ, Silvestre J, Al Maaieh M, Qureshi SA. Clostridium difficile colitis in patients undergoing lumbar spine surgery. Spine. 1 de septiembre de 2014;39(19):E1167-1173. [ Links ]
13. Mackowski MJ, Barnett RE, Harbrecht BG, Miller KR, Franklin GA, Smith JW, et al. Damage control for thoracic trauma. Am Surg. septiembre de 2014;80(9):910-3. [ Links ]
14. Kung S-C, Lin W-T, Tsai T-C, Lin M-H, Chang C-H, Lai C-C, et al. Epidemiologic characteristics and outcomes of major trauma patients requiring prolonged mechanical ventilation. Medicine (Baltimore). diciembre de 2017;96(52):e9487. [ Links ]
15. Sammon J, Trinh VQ, Ravi P, Sukumar S, Gervais M-K, Shariat SF, et al. Health care-associated infections after major cancer surgery: temporal trends, patterns of care, and effect on mortality. Cancer. 15 de junio de 2013;119(12):2317-24. [ Links ]
16. Kohler P, Kuster SP, Bloemberg G, Schulthess B, Frank M, Tanner FC, et al. Healthcare-associated prosthetic heart valve, aortic vascular graft, and disseminated Mycobacterium chimaera infections subsequent to open heart surgery. Eur Heart J. 21 de octubre de 2015;36(40):2745-53. [ Links ]
17. Aquina CT, Probst CP, Becerra AZ, Hensley BJ, Iannuzzi JC, Noyes K, et al. High Variability in Nosocomial Clostridium difficile Infection Rates Across Hospitals After Colorectal Resection. Dis Colon Rectum. abril de 2016;59(4):323-31. [ Links ]
18. Kochhar A, Pronovost PJ, Gourin CG. Hospital-acquired conditions in head and neck cancer surgery. The Laryngoscope. julio de 2013;123(7):1660-9. [ Links ]
19. Stenlund M, Sjodahl R, Pia Yngman-Uhlin RN. Incidence and potential risk factors for hospital-acquired pneumonia in an emergency department of surgery. Int J Qual Health Care J Int Soc Qual Health Care. 1 de abril de 2017;29(2):290-4. [ Links ]
20. Brotfain E, Sebbag G, Friger M, Kirshtein B, Borer A, Koyfman L, et al. Invasive Candida Infection after Upper Gastrointestinal Tract Surgery for GastricCancer. Int J Surg Oncol. 2017;2017:6058567. [ Links ]
21. Becher RD, Hoth JJ, Neff LP, Rebo JJ, Martin RS, Miller PR. Multidrug-resistant pathogens and pneumonia: comparing the trauma and surgical intensive care units. Surg Infect. agosto de 2011;12(4):267-72. [ Links ]
22. Armstrong JG, Li C-H, Liao J, Byrn JC. Right Colectomy and Abdominal Perineal Resection for Cancer : Do Urinary Tract Infections Impact Outcomes? Surg Infect . julio de 2017;18(5):570-6. [ Links ]
23. Evaristo-Mendez G, Rocha-Calderon CH. [Risk factors for nosocomial pneumonia in patients with abdominal surgery]. Cir Cir. febrero de 2016;84(1):21-7. [ Links ]
24. Nosova K, Nuno M, Mukherjee D, Lad SP, Boakye M, Black KL, et al. Urinary tract infections in meningioma patients: analysis of risk factors and outcomes. J Hosp Infect. febrero de 2013;83(2):132-9. [ Links ]
25. Torchia MG, Danzinger RG. Perioperative blood transfusion and albumin administration are independent risk factors for the development of postoperative infections after colorectal surgery. Can J Surg J Can Chir. junio de 2000;43(3):212-6. [ Links ]
26. Rebollo MH, Bernal JM, Llorca J, Rabasa JM, Revuelta JM. Nosocomial infections in patients having cardiovascular operations: a multivariate analysis of risk factors. J Thorac Cardiovasc Surg. octubre de 1996;112(4):908-13. [ Links ]
27. Balentine C, Subramanian A, Palacio CH, Sansgiry S, Berger DH, Awad SS. AVAS Best Clinical Resident Award (Tied): management and outcomes of the open abdomen in nontrauma patients. Am J Surg. noviembre de 2009;198(5):588-92. [ Links ]
28. Sharma P, Bomireddy R, Phillips S. Clostridium difficile-associated diarrhoea after internal fixation of intertrochanteric femoral fractures. Eur J Clin Microbiol Infect Dis Off Publ Eur Soc Clin Microbiol. octubre de 2003;22(10):615-8. [ Links ]
29. Wald H, Epstein A, Kramer A. Extended use of indwelling urinary catheters in postoperative hip fracture patients. Med Care. octubre de 2005;43(10):1009-17. [ Links ]
30. Bowrey DJ, Evans MD, Clark GWB. Impact of methicillin-resistant Staphylococcus aureus infection on outcome after esophagectomy. World J Surg. febrero de 2007;31(2):326-31. [ Links ]
31. Beovic B, Matos B, Bosnjak R, Seme K, Mueller-Premru M, Hergouth-Krizan V, et al. Prevention of nosocomial lower respiratory tract infections in patients after intracranial artery aneurysm surgery with a short course of antimicrobials. Int J Antimicrob Agents. julio de 2003;22(1):60-6. [ Links ]
32. Izuel Rami M, Garcia Erce JA, Gomez-Barrera M, Cuenca Espierrez J, Abad Sazatornil R, Rabanaque Hernandez MJ. [Relationship between allogeneic blood transfusion, iron deficiency and nosocomial infection in patients with hip fracture]. Med Clin (Barc). 15 de noviembre de 2008;131(17):647-52. [ Links ]
33. Kamel HK. The frequency and factors linked to a urinary tract infection coding in patients undergoing hip fracture surgery. J Am Med Dir Assoc. octubre de 2005;6(5):316-20. [ Links ]
34. Bouza E, Perez A, Munoz P, Jesus Perez M, Rincon C, Sanchez C, et al. Ventilator-associated pneumonia after heart surgery: a prospective analysis and the value of surveillance. Crit Care Med. julio de 2003;31(7):1964-70. [ Links ]
35. Velásquez A. Infecciones asociadas a la atención en salud (intrahospitalarias) [Internet]. Disponible en: http://santamargarita.gov.co/intranet/pdf/Otros/MANUAL.pdf [ Links ]
6Conflict of Interest: The authors of this research declare no conflicts of interest in relation to the publication and preparation of this manuscript.
7Author Contributions: All authors declare to have reviewed and validated the content of the manuscript, including tables, figures, and text, and thereby take responsibility for its content.
Received: February 09, 2023; Accepted: June 13, 2023











 text in
text in