Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Cirugía paraguaya
On-line version ISSN 2307-0420
Cir. parag. vol.47 no.2 Asunción Aug. 2023
https://doi.org/10.18004/sopaci.2023.agosto.24
Original article
Percutaneous surgery, 5 years experience in a medium complexity hospital
1Ministerio de Salud Pública y Bienestar Social, Hospital Regional de Encarnación. Departamento de Cirugía. Encarnación, Paraguay.
Introducción: El drenaje percutáneo es una terapéutica eficaz para las colecciones y otras patologías. Las guía imagenológicas utilizadas suelen ser la ecografía y la tomografía.
Método: Estudio descriptivo, retrospectivo de corte transversal. Se analizaron las historias clínicas de los pacientes sometidos a drenaje percutáneo en el Hospital Regional de Encarnación en un periodo de 5 años.
Resultados: Se incluyeron 81 pacientes (53% varones, 47% mujeres), edad promedio 50 años. Las indicaciones fueron: 21% absceso hepático, 11% colecciones postoperatorias, 10% drenaje biliar, el 9% nefrostomías; 7% gastrostomías. El 56% de los procedimientos fueron ecoguiados. La técnica de Seldinger se utilizó mayormente; el catéter multipropósito tipo pigtail se utilizó en el 65% de los casos y el de vía venosa central en el 23%. El promedio de permanencia del catéter fue 15 días; con 4% de complicaciones. La tasa de éxito fue del 98,5%.
Conclusiones: La cirugía percutánea es eficaz y segura. La utilización de catéteres sin medios de fijación interna (via venosa central) son útiles en situaciones de urgencia, no representando mayor riesgo.
Palabras clave: Drenaje percutáneo; colecciones; guía ecográfica; catéteres venosos centrales
Introduction: Percutaneous drainage is an effective therapy for collections and other pathologies. The commonly used imaging guides are ultrasound and tomography. Methods: Descriptive, retrospective cross-sectional study, review of medical records of patients who underwent percutaneous drainage at the Hospital Regional de Encarnación over a 5-year period were analyzed. Results: 81 patients were included (53% males, 47% females), with an average age of 50 years. Indications were as follows: 21% hepatic abscess, 11% postoperative collections, 10% biliary drainage, 9% nephrostomies, and 7% gastrostomies. 56% of procedures were guided by ultrasound. The Seldinger technique was predominantly used, with the multipurpose pigtail catheter employed in 65% of cases, and the central venous catheter in 23%. The average catheter duration was 15 days, with a 4% complication rate. The success rate was 98.5%. Conclusions: Percutaneous surgery is effective and safe. The use of catheters without internal fixation (central venous catheters) is valuable in emergency situations, posing no significant risk.
Key words: Percutaneous drainage; collection; ultrasound guidance; central venous catheters.
INTRODUCTION
Intra-abdominal abscesses can occur in various regions of the abdomen and may arise following surgical procedures, trauma, or as a result of infections or abdominal inflammation. If left untreated, abscesses can spread to adjacent structures, leading to complications1.
In a case series study, ultrasound-guided percutaneous drainage (PD) was curative in 82.6%, palliative in 8.7%, and failed in 8.7% of cases, establishing it as a safe alternative to surgery2. Another study reported a 99% success rate for PD3. Among the various applications of PD, biliary drainage can be used as a treatment option for obstructive jaundice when endoscopic retrograde cholangiopancreatography (ERCP) is unsuccessful, with a low frequency of complications4.
For hepatic abscesses, PD has become the treatment of choice. A single puncture and aspiration suffice for abscesses under 5 cm in diameter, while larger abscesses require image-guided PD with the placement of a multipurpose pigtail catheter5,6. Additionally, PD can be used for psoas muscle abscesses7,8.
PD is also indicated for complications of pancreatitis, such as pancreatic pseudocysts, infected collections, or necrotizing pancreatitis, to evacuate contents and avoid open necrosectomy9,10.
The multipurpose pigtail catheter is the most commonly used, with the catheter diameter determined by the material being drained, thicker tubes preferred for more viscous material. In our setting, administrative issues sometimes necessitate the use of alternative catheters, such as narrower central venous catheters.
This study aims to present the experience with percutaneous procedures performed in the Surgery Department of the Regional Hospital of Encarnación from 2017 to 2021.
MATERIALS AND METHODS
This is an observational, descriptive, cross-sectional, retrospective study. A non-probabilistic sampling of consecutive cases was conducted, involving a review of medical records of patients who underwent percutaneous procedures at the Regional Hospital of Encarnación, Paraguay, between January 2017 and December 2021.
Inclusion criteria: Complete medical records of patients who underwent percutaneous procedures for therapeutic, bridge-to-definitive, or diagnostic purposes were included.
Exclusion criteria: Incomplete medical records or records of patients undergoing surgical drainage were excluded.
Variables studied included age, sex, diagnosis, imaging guide used for diagnosis and the procedure, anesthesia, catheter type and caliber, catheter dwell time, success rate, and complications.
RESULTS
The study included 81 patients who underwent percutaneous procedures during the specified time frame. Of these, 53% (43 patients) were male and 47% (38 patients) were female, with an average age of 50 years (range 15-87, standard deviation 17).
Regarding the indications for the procedure, hepatic abscesses accounted for the main indication at 21% (17 patients), followed by postoperative collections at 15% (12 cases), biliary drainage for neoplastic-related jaundice at 10% (8 cases), nephrostomies for severe hydronephrosis due to oncological pathologies at 9% (7 cases), gastrostomies for nutritional support at 7% (6 cases), and renal and perirenal abscesses at 6% (5 cases). Other less frequent cases are detailed in Table 1.
Table 1. Distribution according to diagnosis of patients undergoing percutaneous drainage. n=81
| Diagnosis | n | % |
|---|---|---|
| Hepatic abscess | 17 | 21 % |
| Postoperative collection | 12 | 15 % |
| Biliary drainage | 8 | 10 % |
| Nephrostomy | 7 | 9 % |
| Gastrostomy | 6 | 7 % |
| Renal-perirenal abscess | 5 | 6 % |
| Complicated hepatic cyst | 4 | 5 % |
| Pancreatic pseudocyst | 4 | 5 % |
| Pancreatic abscess | 4 | 5 % |
| Psoas abscess | 3 | 4 % |
| Retroperitoneal abscess | 2 | 2 % |
| Colonic diverticulitis | 2 | 2 % |
| Infected rectus sheath hematoma | 2 | 2 % |
| Others * | 5 | 6 % |
| Total | 81 | 100 % |
* Splenic cyst 1 case, mesenteric cyst 1, post-traumatic hepatic bilioma 1, wall abscess 1, prevesical abscess 1.
The auxiliary imaging methods used for diagnosing the conditions that led to perform a percutaneous drainage was computed tomography (CT) in 67% (54) of cases, and ultrasound in 33% (27).
Regarding the imaging method used for the guidance of puncture, ultrasound was used in 56% (45) of procedures. A combination of ultrasound and fluoroscopy (transparietohepatic drainages) was used in 22% (18) of cases. CT was employed in 15% (12) of cases, and fluoroscopy alone was used in 7% (6) of cases, which corresponded to percutaneous gastrostomies (Graph 1).
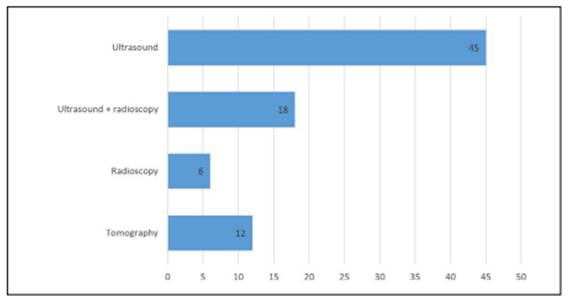
Graph 1. Distribution according to the imaging method used for the procedure’s puncture guidance. n=81.
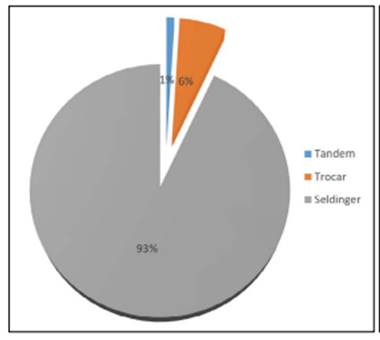
When evaluating the PD technique, it was identified that the Seldinger technique was used in 93% (75) of cases, trocar technique in 6% (5), and tandem technique in 1% (1). (Graph 2 ).
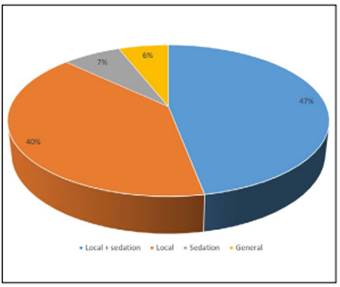
Regarding the type of anesthesia used, sedation with local anesthesia was found in 47%, corresponding to 38 cases (2% lidocaine at a dose of 5mg/kg and propofol at 1mg/kg). Sedation alone was used in 7% (6) of cases, local anesthesia alone in 40% (32), and general anesthesia in 6% (5), as shown in Graph 3
The principal catheter udes for PD was the multipurpose pigtail catheter in 64% (52) of cases, followed by the central venous catheter in 23.5% (19) of cases. The catheter with an inflatable balloon (gastrostomy set) was used in 7.5% (6) of cases, and the Malecot type was used in 5% (4) of cases. The use of central venous catheters was due to the lack of availability of multipurpose catheters in the hospital.
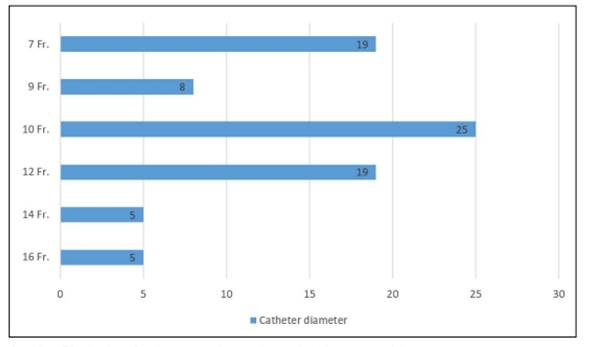
The most used catheter sizes were 10Fr. (31%), 12Fr. (23.5%), and 7Fr. (23.5%) (Graph 4).
The average catheter dwell time was 15 days, with a range of 1 to 65 days and a standard deviation of 10 days. Patients who were discharged with the catheter still in place were excluded from this determination.
Complications occurred in 4% (3) of cases: 1 case of pericatheter infection, 1 case of accidental catheter removal, and 1 case of catheter obstruction that was resolved by exchanging the catheter.
Follow-up could not be conducted for 10 patients due to various reasons. The success rate among patients who could be followed was 70 out of 71, representing a 98.5% success rate. One failure was observed in a patient with a drained hepatic abscess that recurred a few weeks after catheter removal, requiring a new drainage procedure.
DISCUSSION
About gender distribution, our findings differ from the literature, where a slight predominance of women was reported (55%). In our sample, male patients were more common, accounting for 53%.
The literature mentions indications for PD such as hepatic abscesses, acute cholecystitis, biliomas, biliary obstruction, pseudocysts, and pancreatic abscesses, among others1, which aligns with the drainage indications observed in our evaluated population.
In most cases, clinical suspicion prompts the need for imaging confirmation, with CT being the preferred method7. In our study, CT was used in 67% of cases for diagnosing the conditions that necessitated various percutaneous drainages.
Existing literature cites that ultrasound-guided PD is effective for managing abdominal collections2. In our sample, ultrasound was the most commonly used method in 56% of cases, often combined with fluoroscopy in 22% of cases.
Carlos Priarone's publication regarding puncture techniques mentions that the majority of interventions (86.6%) are performed using the Seldinger technique3, which is similar to our study, where the Seldinger technique was used in 93% of cases.
Regarding the type of catheter used, literature does not commonly discuss the use of a 7Fr central venous catheter for drainage purposes. In our sample, we utilized this type of catheter in 24% of cases with positive outcomes and no complications.
Existing literature reports percutaneous drainage success rates ranging from 80% to 100% depending on the location11. In our study, the success rate was 98.5%.
CONCLUSION
In our case series, the majority of patients undergoing drainage procedures were male. The primary indication for drainage was hepatic abscesses, followed by postoperative collections. The Seldinger technique under ultrasound guidance was the most commonly used method for catheter placement, and the multipurpose pigtail catheter was the most frequently employed. The average catheter dwell time was 15 days, and the procedure's success rate was 98.5%.
The use of catheters without internal fixation mechanisms, such as central venous catheters in our case, proves useful in emergency situations and does not present a higher risk in our experience.
REFERENCES
1. Cerón Pérez DT, Báez Quiñónez DF, Álvarez Pérez LC, Zambrano Palma DM. Utilidad de ecografía en drenaje percutáneo. RECIAMUC [Internet]. 2020;4(3):208-15. Disponible en: https://reciamuc.com/index.php/RECIAMUC/article/view/514/773 [ Links ]
2. López Fernández M, Castro Revollo M. Drenaje percutáneo de colecciones abdominales guiados por ecografía. Rev. Méd. La Paz [Internet]. 2011;17(1):26-30. Disponible en: http://www.scielo.org.bo/scielo.php?script=sci_arttext&pid=S1726-89582011000100005&lng=es [ Links ]
3. Ramírez J, Arroyave Y, Quilindo C, Romero T, Priarone C. Manejo del drenaje percutáneo guiado por imágenes en un hospital de tercer nivel. Rev. colomb. cir. [Internet]. 2019; 34(2):163-170. Disponible en: http://www.scielo.org.co/scielo.php?script=sci_arttext&pid=S2011-75822019000200163&lng=en [ Links ]
4. Santillán Morales R, Ríos L. Experiencia de drenaje biliar percutáneo en pacientes del Hospital Ángeles Mocel. Acta Médica Grupo Ángeles [Internet]. 2021;19(1):15-20. Disponible en: https://www.medigraphic.com/cgi-bin/new/resumen.cgi?IDARTICULO=98564 [ Links ]
5. Campuzano Rizzo BL, Paredes JN, Novillo Flores M del C, Cárdenas Chávez AB. Drenaje de abscesos hepáticos guiados por tomografía. Recimundo [Internet]. 2022;6(2):338-45. Disponible en: https://www.reciamuc.com/~recimund/index.php/es/article/view/1577/2034 [ Links ]
6. Bazán Portocarrero S, Pinto Sánchez J, Godoy Martínez D, Campos Torres R, Asmat Garaycochea P, Arias Schreiber M. Drenaje Percutáneo de absceso piógeno hepático: eficacia del manejo. Rev. gastroenterol. Perú [Internet]. 2003; 23(1): 17-21. Disponible en: http://www.scielo.org.pe/scielo.php?script=sci_arttext&pid=S1022-51292003000100002&lng=es [ Links ]
7. González-Rivas M, Ramirez-Preciado I, Serrano-Gómez D. Absceso de Psoas. Resolución percutánea. Actual Med. 2021; 106(812): 78-80. Disponible en: https://digibug.ugr.es/bitstream/handle/10481/71061/am-812-cc01.pdf?sequence=1&isAllowed=y [ Links ]
8. Iida K, Yoshikane K, Tono O, Tarukado K, Harimaya K. The effectiveness of a percutaneous endoscopic approach in a patient with psoas and epidural abscess accompanied by pyogenic spondylitis: a case report. Journal of Medical Case Reports [Internet]. 2019;13(1). Available from: https://jmedicalcasereports.biomedcentral.com/articles/10.1186/s13256-019-2193-6 [ Links ]
9. Pereira FA, Salazar F, Venales Y. Drenaje endoscópico y percutáneo del pseudoquiste pancreático infectado. Reporte de casos. Revista GEN [Internet]. 2018;72(2):52-6. Disponible en: http://genrevista.org/index.php/GEN/article/view/394 [ Links ]
10. Agüero-Milanés A, Hernández-Castro J, Larrondo-Muguercia H. Drenaje percutáneo de colección necrótica encapsulada en pancreatitis necrotizante, guiado por ultrasonografía. Acta Médica [revista en Internet]. 2020; 21 (1) Disponible en: http://www.revactamedica.sld.cu/index.php/act/article/view/43 [ Links ]
11. Latorre-Tomey R, Lesta-Colmenero M, Sainz-Sanchez. percutáneo de abscesos posquirúrgicos. Intervencionismo. [revista en Internet]. 2019;19(2):60-66. Disponible en: http://revistaintervencionismo.com/wp-content/uploads/2019_02_original2.pdf [ Links ]
Received: May 12, 2023; Accepted: August 24, 2023











 text in
text in