Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Cirugía paraguaya
On-line version ISSN 2307-0420
Cir. parag. vol.47 no.1 Asunción Apr. 2023
https://doi.org/10.18004/sopaci.2023.abril.36
Case report
Appendiceal tumor in young adult
1Hospital Clínica Panamericana. Servicio de Medicina Interna. Guayaquil, Ecuador.
2Hospital Clínica Panamericana. Servicio de Gastroenterología. Guayaquil, Ecuador.
3Hospital Clínica Panamericana. Servicio de Cirugía General. Guayaquil, Ecuador.
4Universidad de Especialidades Espíritu Santo. Facultad de Medicina. Samborondón, Ecuador.
The appendiceal tumor is a rare entity; it is usually discovered during appendectomy. This is the case of a 21-year-old man admitted due to abdominal pain accompanied by vomiting, high fever, and weight loss. Paraclinical lab test results: hematocrit, 30.7%; hemoglobin, 10.1g/dl. He is examined by the General Surgery unit, and underwent surgery due to clinical signs of acute appendicitis. The surgical findings are granulomatous lesions, and congestive appendix with tumor. The biopsy performed reveals the presence of malignant epithelial neoplasm consistent with adenocarcinoma. He is eventually discharged from the hospital with good prognosis.
Keywords: tumor; appendix; abdominal pain; weight loss
El tumor apendicular es raro, normalmente se descubre durante una apendicectomía. Este es el caso de un varón de 21 años que ingresa por dolor abdominal, acompañado de vómitos, alza térmica y pérdida de peso. En paraclínicos hematocrito: 30,7%, hemoglobina: 10,1g/dl. Evaluado por Cirugía General, intervienen por cuadro de apendicitis aguda; los hallazgos quirúrgicos son lesiones granulomatosas, apéndice congestivo con tumoración. Se toma biopsia que revela neoplasia epitelial maligna consistente con adenocarcinoma. El paciente es dado de alta con buen pronóstico.
Palabres clave: tumor; apéndice; dolor abdominal; pérdida de peso
INTRODUCTION
Appendiceal mucinous neoplasms (AMN) are rare tumors that account for less than 1% of all cancers reported. In their early stage, they are diagnosed incidentally in resection due to suspected appendicitis. In its advanced stage, the disease occurs with distended abdomen related to the mucin accumulated in the peritoneal space. Appendiceal mucinous neoplasms are present in 0.2% to 0.3% of all appendicectomy specimens1.
Preoperative diagnosis is difficult due to lack of pathognomonic signs or symptoms and the fact that over 70% of these patients show clinical symptoms typical of clinical signs of acute appendicitis. Back in 2016, an article published by Xin Xie reported on the case reports of 1.404 patients with appendix adenocarcinoma in the database of the Surveillance, Epidemiology and End Results (SEER) Program in China from 2004 through 2013. Out of these cases, 48.7% were positive mucinous adenocarcinomas while 51.3% were non-mucinous colon adenocarcinomas2.
Other studies reveal that 0.9% to 1.4% of all appendectomies performed to treat acute appendicitis are of neoplastic origin and that 2% and 6% of the patients diagnosed with acute appendicitis show the presence of an appendiceal mass often described as an inflammatory phlegmon or abscess.(3
Imaging reports play an important role in diagnosis. Computed tomography scan often shows simple or retention mucoceles in the appendix looking like cystic structures with a smooth wall. An appendix of more than 15 mm in diameter, soft tissue mass, thickening or irregularity of the wall leads to suspected mucinous neoplasm4.
Appendiceal tumors are a rare condition that accounts for 1% of the overall number of appendectomies performed. According to the wide variety of appendiceal tumors included in the database «Surveillance, Epidemiology, and End Results» (SEER) from the United States National Cancer Institute from 1973 through 2007 the most common histological type is mucinous adenocarcinoma followed by intestinal adenocarcinoma. Appendiceal adenocarcinomas (AA) represent less than 0.2% of all appendectomies performed according to the international medical literature available5.
The classification of appendiceal mucinous neoplasms (AMN) is controversial when they lack aspects of malignancy. However, they are associated with peritoneal dissemination of mucin. Low-grade tumors limited to the appendix are clinically benign while those that have already spread to the peritoneum can have a very different clinical progression. On the other hand, tumors with appendiceal wall invasion or high-degree tumors of atypia can progress aggressively, and are considered adenocarcinomas. According to the Pai and Longacre classification, AMN can be categorized into: mucinous cystadenoma (MC), mucinous neoplasm of uncertain malignant potential (NUMP), mucinous neoplasm of low malignant potential (NLMP), and mucinous adenocarcinoma (MA). Mucinous ascites known as pseudomyxoma peritonei (PP) is present in more than 50% of these patients and its presence is indicative of a more advanced stage and worse prognosis. It can also occur as low- (diffuse peritoneal adenomucinosis) or high-grade (diffuse peritoneal carcinomatosis)1).
The objective of this case report is to look into the symptomatology of appendiceal signs more deeply without ruling out any suspicion of greater complications like appendiceal cancer.
A case study is conducted since its early management was that of a classic acute appendicitis, without any apparent suspicion of other conditions. Lesions indicative of neoplasm are seen during surgery. Therefore, a decision is made to study tumor markers and histopathology.
Since we are dealing with an uncommon pathology, and there is not such a thing as a clear diagnosis and management protocol, more concise approaches for cases like this are expected in the future.
CASE REPORT
This is the case of a 21-year-old man without a relevant past medical history. He presents to the emergency department at Hospital Clínica Panamericana, Guayaquil, Ecuador, with clinical signs with a 12-hour history of colic-like intense abdominal pain in the right hemiabdomen. Pain grows with breathing followed by nausea that results in bilious vomiting on 4 occasions. In addition, over the past 4 hours fever goes up. The patient has a 1-month history of progressive weight loss and abdominal pain. This calls our attention, which is why tumor markers are requested.
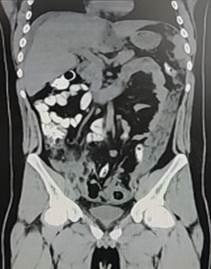
Lab test results: microcytic hypochromic anemia; hematocrit, 30.7%; hemoglobin, 10.1g/dL. The abdominal computed tomography scan performed reveals the presence of a large amount of fluid in the abdominal cavity of peri-hepatic and perisplenic predominance (Figure 1).
After consultation with the General Surgery unit due to persistent abdominal pain and imaging data, the patient is assessed for abdominal pain consistent with appendiceal clinical signs based on the lab test results and imaging data, indicate of a diagnosis suggestive of acute appendicitis. Therefore, it is decided to perform laparoscopic appendectomy.
The findings during the surgery revealed the presence of granulomatous lesions in the entire abdominal cavity, granulomatous omentum, and congestive cecal appendix with tumor in its tip with mesoappendix infiltration, peritoneal fluid. Biopsy is performed at this point (Figures 2 and 3). Results of peritoneal fluid and tumor markers: lymphocytes in peritoneal fluid >70% = 98%; leukocytes > 500 cells = 501; proteins > 3g = 5.25; fat < 1.1= 0.9 murky yellow in color. Carcinoembryonic antigen (CEA): 14.22 ng/mL; CA 19.9: 5.63 u/mL; alpha fetoprotein (AFP), 1.15 u/mL,

Figure 2: 8 cm x 1 cm cecal appendix, smooth serosa, grey in color, with several tumor elevations at middle and distal third level, white in color, irregular and semisoft measuring 2 cm in its major axis.
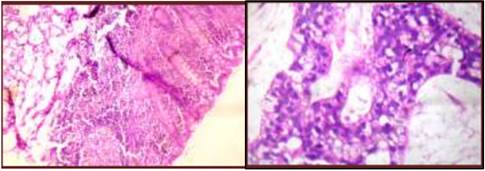
Figure 3: cecal appendix; with mucosa covered by columnar epithelium, with infiltration of epithelial neoplasm of mucinous pattern consisting of pleomorphic and hyperchromatic irregular nuclei cells with extensive mucinous content.
The result of the appendix biopsy is consistent with infiltrating mucinous adenocarcinoma in the cecal appendix with spread to the periappendiceal adipose tissue. Following this finding, it is requested that the case be assessed by the gastroenterology unit to perform endoscopic and biopsy studies (Figure 4) to see the actual spread of the adenocarcinoma.
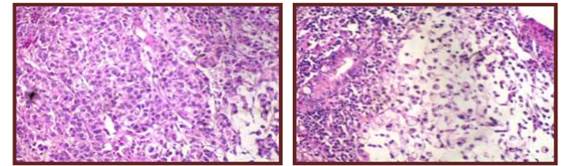
Figure 4: Transverse Colon Mucosa, malignant epithelial neoplasm of glandular pattern consisting of enlarged pleomorphic, irregular, hyperchromatic nuclei cells with wide eosinophilic cytoplasm and.
The endoscopic colon mucosa biopsy is performed. It confirms adenocarcinoma spread to the transverse colon where high columnar epithelium is observed infiltrated by a malignant epithelial neoplasm of glandular pattern consisting of enlarged, hyperchromatic, irregular, pleomorphic nuclei cells wide eosinophilic cytoplasm, atypical signet ring cells with intracellular and extracellular mucin lakes. Biopsy results are consistent with an infiltrating mucinous appendix adenocarcinoma.
Patient with favorable postoperative period. He is discharged within 2 weeks due to the biopsy result times prior to starting treatment with follow-up outpatient visits with chemotherapy treatment. The patient is administered 12 cycles of folfox 14 chemotherapy, oxaliplatin 95 mg/m2 (136 mg IV on days 1 #3 amp); leucovorin 400 mg/m2 (640 mg IV on days 1 #13 amp); 5 fluorouracil 400 mg/m2 (640 mg IV on days 1 #2 amp); and 5 fluorouracil 600 mg/m2 (1940 mg in 48 hours ic # 4amp).
DISCUSSION
Malignant neoplasms of the appendix are rare. In its database of Surveillance, Epidemiology and End Results (SEER), the United States National Cancer Institute reports that appendiceal cancer accounts for 0.4% of all gastrointestinal tumors. Due to the fact that appendix carcinomas can cause appendicitis or appendix rupture, the most common symptoms of primary carcinomas of the appendix occur in a similar way to acute appendicitis1). The patient of this study had intense abdominal pain followed by nausea and vomiting, which is typical of acute appendiceal clinical signs.
In the case report presented here, the patient reported a 1-month history of progressive weight loss and abdominal pain.
According to the United States National Cancer Institute, appendiceal adenocarcinomas account for 0.4% of all malignant gastrointestinal tumors. The mean age at diagnosis is 50 years predominantly in women6). In contrast with the current study reported, no relationship was seen between sex and age. The patient was 21 years old and he is a man. Pathology test result was an infiltrating mucinous adenocarcinoma.
In a case studied, it was reported that 37.2% of the patients showed signs and symptoms of acute abdomen, which is suggestive of acute appendicitis. In 23%, the appendiceal lesion was discovered incidentally during another surgical procedure. In 77.8% of cases, cardiovascular comorbidities (53.3%) and diabetes mellitus (15.5%) were reported in patients with appendiceal mucinous adenocarcinoma7). The case reported here presented as a classic appendiceal case without a relevant past medical history whatsoever.
A study of the findings made during the surgeries performed that showed appendiceal perforation, free appendiceal fluid, and peritoneal pseudomyxoma was conducted8). In the case presented here free peritoneal fluid was confirmed and it was murky and sallow (3000cc). There were granulomatous lesions all over the abdominal cavity.
Once diagnosis was confirmed, depending on how compromise the primary tumor was, there is indication of right hemicolectomy plus lymph nodal dissection, a procedure that allows suitable tumor staging. This course of action differs from the management of other histologic types of primary tumors of the appendix. The prognosis of adenocarcinomas is worse than that of other appendiceal tumors, with survival rates of 40% to 50% at 5 years in the best series reported5). In the case report shown here, laparoscopic appendectomy was performed with adjuvant chemotherapy, and follow-up outpatient visits.
The conclusion is that, although appendiceal tumor is extremely rare, it is important not to rule out this type of conditions in the presence of appendiceal clinical signs. Therefore, the macroscopic finding is important to suspect this type of neoplasm while keeping in mind that the ultimate diagnosis will need to histopathological. In our case, our 21-year-old male patient had no relevant past medical history, which is not consistent with the statistics coming from the medical literature available on appendiceal neoplasms. However, the accompanying symptomatology the patient complained of like diffuse abdominal pain, and progressive weight loss without any apparent explanation led us to suspect neoplasm.
REFERENCES
1. Shaib WL, Assi R, Shamseddine A, Alese OB, Staley C, Memis B, et al. Appendiceal Mucinous Neoplasms: Diagnosis and Management. The Oncologist [Internet]. septiembre de 2017 [citado 5 de febrero de 2023];22(9):1107-16. Disponible en: Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5599200/ [ Links ]
2. Stein S, Raymond B, Stein S, D.o BR. Appendiceal Adenocarcinoma Presenting As Perforated Appendicitis. Cureus J Med Sci [Internet]. 26 de febrero de 2021 [citado 5 de febrero de 2023]; 13(2). Disponible en: Disponible en: https://www.cureus.com/articles/53500-appendiceal-adenocarcinoma-presenting-as-perforated-appendicitis [ Links ]
3. Teixeira FJR, Couto Netto SD, Akaishi EH, Utiyama EM, Menegozzo CAM, Rocha MC. Acute appendicitis, inflammatory appendiceal mass and the risk of a hidden malignant tumor: a systematic review of the literature. World J Emerg Surg WJES [Internet]. 9 de marzo de 2017 [citado 5 de febrero de 2023]; 12: 12. Disponible en: Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5343298/ [ Links ]
4. Tirumani SH, Fraser-Hill M, Auer R, Shabana W, Walsh C, Lee F, et al. Mucinous neoplasms of the appendix: a current comprehensive clinicopathologic and imaging review. Cancer Imaging [Internet]. 22 de febrero de 2013 [citado 5 de febrero de 2023];13(1):14-25. Disponible en: Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3582328/ [ Links ]
5. Fulle C A, Castillo R R, Moreno L P, Orellana G M, Cabreras S M, Briones N P, et al. Análisis de casos de adenocarcinoma apendicular y su manejo en una serie de 10 años en el Hospital Doctor Sótero del Río. Rev Chil Cir [Internet]. agosto de 2017 [citado 5 de febrero de 2023]; 69(4): 297-301. Disponible en: Disponible en: http://www.scielo.cl/scielo.php?script=sci_abstract&pid=S0718-40262017000400006&lng=es&nrm=iso&tlng=es [ Links ]
6. Nutu OA, Marcacuzco Quinto AA, Manrique Municio A, Justo Alonso I, Calvo Pulido J, García-Conde M, et al. Tumores mucinosos del apéndice: incidencia, diagnóstico y tratamiento quirúrgico. Cir Esp [Internet]. 1 de junio de 2017 [citado 5 de febrero de 2023]; 95(6): 321-7. Disponible en: Disponible en: https://www.elsevier.es/es-revista-cirugia-espanola-36-articulo-tumores-mucinosos-del-apendice-incidencia-S0009739X17301380 [ Links ]
7. Benedix F, Reimer A, Gastinger I, Mroczkowski P, Lippert H, Kube R, et al. Primary appendiceal carcinoma--epidemiology, surgery and survival: results of a German multi-center study. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol. agosto de 2010; 36(8): 763-71. [ Links ]
8. Xie X, Zhou Z, Song Y, Li W, Diao D, Dang C, et al. The Management and Prognostic Prediction of Adenocarcinoma of Appendix. Sci Rep [Internet]. 16 de diciembre de 2016 [citado 5 de febrero de 2023]; 6: 39027. Disponible en: Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5159879/ [ Links ]
Authors’ contribution: All the authors contributed drafting this manuscript, and giving their approval for publication purposes.
Received: November 15, 2022; Accepted: February 06, 2023











 text in
text in