Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Cirugía paraguaya
On-line version ISSN 2307-0420
Cir. parag. vol.47 no.1 Asunción Apr. 2023
https://doi.org/10.18004/sopaci.2023.abril.27
Case report
Parathyroid carcinoma. A rare disease with difficult diagnosis. Case report
1Clínica Las Américas - AUNA, Hospital Pablo Tobón Uribe. Medellín, Colombia.
2Clínica Las Américas- AUNA, Instituto de Cancerología. Medellín, Colombia.
3Clínica Las Américas- AUNA. Medellín, Colombia.
4Universidad CES. Medellín, Colombia.
Parathyroid carcinoma is a rare tumor with occasional hormonal activity and symptoms of severe hypercalcemia. Diagnosis is achieved through pathology study and intraoperative findings. Surgery is often the treatment of choice. This is the case of a 61-year-old woman with a preoperative diagnosis of a 4 cm left thyroid nodule-follicular neoplasm (Bethesda category IV) treated with surgery, and with final diagnosis of parathyroid carcinoma. Surgical management and adjuvant therapy with radiotherapy were administered.
Keywords: Parathyroid carcinoma; surgery; diagnosis; treatment
El carcinoma de paratiroides es un tumor raro. Ocasionalmente presenta actividad hormonal y sintomatología sugestiva de hipercalcemia severa. Al diagnóstico se llega estudiando la patología y los hallazgos intraoperatorios, siendo la cirugía su principal forma de tratamiento. Presentamos una paciente de 61 años con diagnóstico preoperatorio de nódulo tiroideo izquierdo de 4 cm, Bethesda IV (neoplasia folicular) derivado a cirugía diagnosticándose finalmente carcinoma de paratiroides. Se realizó manejo quirúrgico y adyuvancia con radioterapia.
Palabras claves: carcinoma de paratiroides; cirugía; diagnóstico; tratamiento
INTRODUCTION
Parathyroid carcinoma is a rare malignant tumor. The levels of parathyroid hormones can be up to 10 times higher compared to normal values (10 pg/mL to 60 pg/mL). Symptom onset can be due to mass effect, muscular pain, headache, pathological fractures, etc.
This is the case of a parathyroid carcinoma found in a 61-year-old woman previously diagnosed with a 5 cm left thyroid nodule with preoperative disease of follicular neoplasm (Bethesda category IV).
CASE REPORT
This is the case of a 61-year-old woman with a 12-month history of left thyroid nodule of progressive growth. The physical examination and palpation conducted revealed the presence of a 5 cm attached, hard, moving nodule occupying most of the left thyroid lobe. The computed tomography scan of the neck revealed the presence of a 55 mm x 37.7 mm x 30 mm solid nodular lesion in the left thyroid lobe with a 29 mm x 18 mm x 20 mm “metastatic nodule” in the lower pole in contact with both the esophagus and trachea (see Figure 1).
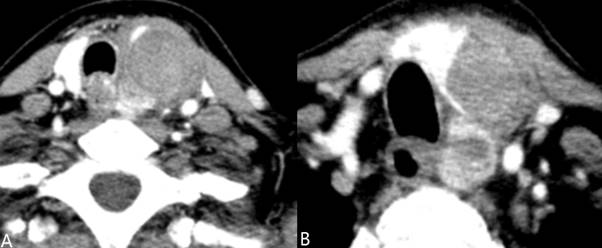
Figure 1. Contrast enhanced computed tomography scan of the neck. Axial view. A: middle third of the thyroid showing a 5 cm lesion partially replacing the left thyroid lobe suggestive of suspicious adenopathy. B: thyroid lower third-left thyroid lobe. The asterisk reveals the presence of a suspicious mediastinal metastasis.
Ultrasound-guided fine needle aspiration biopsy was performed that revealed findings of follicular neoplasm (Bethesda category IV). Thyroid function tests were normal. However, the levels of preoperative parathyroid hormone were 472 pg/mL, and therefore, suggestive of parathyroid adenoma.
Given the size of the lesion it was decided that the best thing to do was to rule out the presence of thyroid carcinoma. Therefore, the patient was prepared for surgery, a total thyroidectomy with mediastinal dissection (level VI) using Medtronic Nim 3 nerve monitoring system (Jacksonville, FL United States). Surgery revealed these findings: a mass occupying the entire left thyroid lobe attached to ipsilateral pre-thyroid muscles. En bloc resection was considered necessary at this point. The recurrent left laryngeal nerve was not compromised by the tumor and, therefore, spared. The left thyroid lower pole revealed the presence of a 3 cm parathyroid adenoma-like lesion that was en bloc resected together with the lobe. No suspicious peritumoral adenopathies were found in the mediastinal dissection. The patient was discharged 1 day after the surgery on 100 mcg of levothyroxine/day and 1500 mg of calcium citrate every 8 hours followed by 0.5 mcg of calcitriol every 12 h since the levels of parathyroid hormones and calcium after surgery were 7.9 pg/mL and 7.2 mg/dL, respectively. This reduced postoperative calcium levels went back to normal after 8 days. The final diagnosis of parathyroid carcinoma was achieved after conducting several studies of tumor markers and discussing the case with the treating group in association with intraoperative findings. The patient was referred for radiotherapy and received 6000 Gray (Cy). Eighteen months after treatment, the patient shows no signs of tumor relapse and her parathyroid hormones and calcium levels remain stable at 13.6 pg/mL and 9.1mg/d, respectively. The patient was, then, referred to the endocrinology unit to discard other systemic alterations the same way other alterations had been discarded before.
DISCUSSION
Parathyroid carcinoma is one of the rarest malignant conditions of the human body. It represents 1% of all cases of primary hyperparathyroidism. It often starts in people between 40 and 50 years old and affects men and women alike1,3,4
Pathogenesis is still unknown, and it can start sporadically or be associated with genetic syndromes like multiple endocrine neoplasm type 1, 2 (MEN 1, MEN 2), familial hyperparathyroidism. Non genetic factors associated with the disease are previous neck radiation, primary hyper-parathyroidism or thyroid cancer1,2.
The main symptom in the disease early stages is a lesion of progressive growth. This, however, in the context of a mass that seems to come from the thyroid leads to ruling out-as it was the case with our patient-the presence of a type of aggressive thyroid carcinoma without considering the possibility of a parathyroid malignant lesion. The presence of preoperative parathyroid hormone levels of 476 pg/mL is suggestive of parathyroid adenoma and not of a malignant lesion of the thyroid gland (in this case parathyroid hormone levels skyrocket > 2000 pg/mL with symptoms associated with this hormonal hypersecretion causing severe hypercalcemia, pathological fractures, renal impairment, etc). If the possibility of parathyroid carcinoma is suspected beforehand given the elevated parathyroid hormone levels, it may have not been necessary to resect the entire thyroid gland, thus limiting resection to the side sustaining the damage5.
Pathology. The biggest problem surrounding the management of this tumoral lesion is diagnosis itself since the early stages of the disease. Therefore, the tomographic findings and elevated parathyroid hormone levels in a patient scheduled for total thyroidectomy and mediastinal dissection would require the resection of this “possible adenoma”. Microscopic findings force pathologists to conduct conventional studies and immunohistochemistry (IHC) staining: chromogranin, Ki-67-which are very specific of this particular condition-and added to calcitonin, protein S100, CD10, CK 19, TTFI, all associated with thyroid cancer. The treating group may be called upon as it happened with our patient to have more in-depth information on intraoperative findings (tumor infiltration in tissues, difficulty dissecting views, location, etc.) to corroborate this description with microscopic findings. In our case, the lesion initially seen in the intraoperative and macroscopic studies that was en bloc resected as a parathyroid adenoma was of left thyroid lower lobe location, which did not facilitate the easy dissection of the lower pole during the macroscopic study as it would have been the case with a typical parathyroid adenoma. On the contrary, diffuse microscopic invasion of the thyroid parenchyma was seen. Overall, these tumors are often > 30 mm in size with capsular and vascular invasion, and even nerve connections, trabecular pattern, cellular atypia, tumor necrosis, and high rate of mitotic activity (often > 5 mitoses per high-power field) (1-6) (see Figure 2).
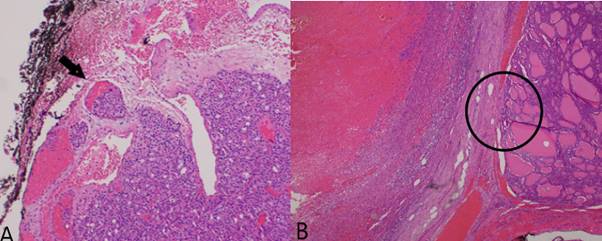
Figure 2. Histologic slices of the surgical piece. A: H&E stained image. Tumor tissue spreading towards the fibrous connective tissue with angioinvasive foci (arrow). Image augmentation (x 10). B: H&E stained image. Tumor tissue (left side) spreading towards the thyroid parenchyma (right side)-circle. Image augmentation (x 40). Pictures taken by the authors.
Supplementary therapy. Surgery is the treatment of choice for this kind of neoplasm. Radiotherapy is spared for cases like the one described with tumor volume, and infiltration of neighboring tissues. Since this tumor is rare, no TNM classification has ever been described to categorized this disease, and have proper management guidelines. Also, there is no scheme available or indication either for the use of chemotherapy to treat this particular entity. (7)
The follow-up tumor marker studies conducted almost 10 and 8 months after surgery confirmed that the patient’s parathyroid hormone levels remained low. PET/CT scan with 18 FDG (positron emission tomography with 18-fluorodeoxyglucose) helps us diagnose relapse that often happen 3 years after the index surgery depending on the early tumor volume. Pulmonary metastases are a common clinical sign too also to locoregional nodes. (6, 7)
CONCLUSIONS
Parathyroid cancer is a rare entity, which is why, on many occasions, it is difficult to distinguish the lesion from a parathyroid adenoma that starts with elevated levels of parathyroid hormones. Nonetheless, elevated parathyroid hormones levels associated with severe hypercalcemia and pathological fractures should raise a few eyebrows in the treating team. En bloc surgical resection of ipsilateral thyroid lobe or the entire thyroid is the treatment of choice unless thyroid carcinoma is discarded. Tumor marker studies may be necessary to confirm the diagnosis of malignancy. Radiotherapy is indicated for patients with large tumors. However, no chemotherapy pattern has ever been designed for this kind of tumors.
REFERENCES
1. Kaszczewska M, Popow M, Chudziński WI, et al. A Woman with a 27-Year History of Hyperparathyroidism and Hypercalcemia Who Was Diagnosed with Low-Grade Parathyroid Carcinoma. Am J Case Rep. 2021 Mar 11; 22: e930301. doi: 10.12659/AJCR.930301 [ Links ]
2. Gibi B, Shah JP. Parathyroid carcinoma. Clin Oncol (R Coll Radiol). 2010 Aug;22(6):498-507. doi: 10.1016/j.clon.2010.04.007 [ Links ]
3. Al-Kurd A, Mekel M, Mazeh H. Parathyroid carcinoma. Surg Oncol. 2014 Jun;23(2):107-14. doi: 10.1016/j.suronc.2014.03.005. [ Links ]
4. Suganuma N, Iwasaki H, Shimizu S, et al. Non-functioning parathyroid carcinoma: a case report. Surg Case Rep. 2017 Dec; 3(1):81. doi: 10.1186/s40792-017-0357-4 [ Links ]
5. Guo H, Mai R, Liu M, Peng H, Yang X, Wu M, Zhang G. Nonfunctional parathyroid carcinoma after breast carcinoma. J Clin Oncol. 2013 Mar 20;31(9): e122-4. doi: 10.1200/JCO.2012.44.7227 [ Links ]
6. Huertas-Quintero JA, Romero MC. Cáncer paratiroideo como causa de fractura y osteoporosis secundaria en el adulto mayor: reporte de caso y revisión de la literatura. Rev. Colomb. Endocrinol. Diabet. Metab. 021; 8(1): e693. https://doi.org/10.53853/encr.8.1.693 [ Links ]
7. Wang P, Xue S, Wang S, Zhi Lv, Xianying M, Guimin W, et al. Clinical characteristics and treatment outcomes of parathyroid carcinoma: A retrospective review of 234 cases. Oncol Lett. 2017 Dec;14(6): 7276-82. doi: 10.3892/ol.2017.7076 [ Links ]
Conflicts of interest: CSD teaches courses on nerve monitorization in head and neck surgery for Latin American surgeons with support from Medtronic (Jacksonville, FL. United States). The remaining authors declared no conflicts of interest whatsoever.
Authors’ contributions: CSD and MFP performed the surgery, drafted and reviewed the manuscript. AM held a discussion with the entire medical team, and studied the immunohistochemistry staining results that eventually led to achieving a diagnosis of parathyroid cancer. NS was involved in the bibliographic search and drafting of the manuscript.
Received: November 18, 2022; Accepted: February 03, 2023











 text in
text in 



