Chikungunya, a mosquito-borne viral disease, has rapidly emerged as a pressing public health concern in Latin America since late 2013, posing significant challenges to control efforts across the region1,2. The rapid spread of the disease during 2024-2025, coupled with limited resources, infrastructure, and other factors, has exacerbated the situation. However, the Latin American public health community has demonstrated remarkable resilience, requiring a coordinated and multifaceted approach to combat this persistent threat3.
One of the primary challenges in controlling Chikungunya in Latin America lies in the complex interaction between the virus, its vectors, and the environment. Environmental factors such as temperature and humidity influence the distribution and abundance of Aedes mosquitoes, the primary vectors of the Chikungunya virus (CHIKV). In regions with favorable environmental conditions, vector populations thrive, increasing the risk of disease transmission. Urbanization and population growth have also created breeding grounds for mosquitoes, further facilitating the spread of Chikungunya. Addressing these environmental determinants requires not just efforts but sustained and persistent efforts in vector surveillance and control and community engagement to promote environmental management practices. The urgency of this task cannot be overstated4,5.
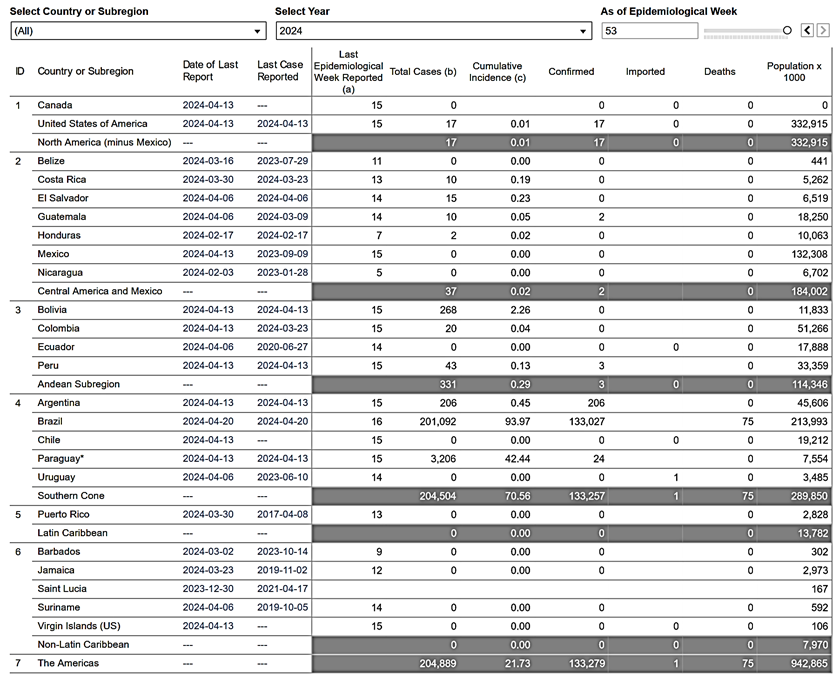
The current situation in the region is concerning. In 2023, 410,754 cases were reported in the Americas region (Table 1). The highest number is in Brazil (265,503), followed by Paraguay (140,095). In 2023, 419 deaths were associated with CHIKV (Table 1). During the ongoing 2024, in just a few months, 204,889 cases have been reported (Table 2), 201,092 in Brazil and 3,206 in Paraguay (Table 2). Additionally, 75 deaths due to CHIKV have already been reported in 2024 (Table 2).
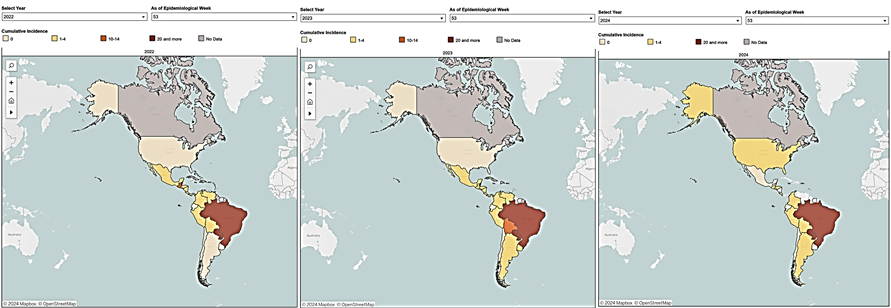
Despite that, multiple countries have reported CHIKV in 2022-2024 (Figure 1), showing the relevant geographical spread in the region. CHIKV has become a significant arboviral disease in the region, and after dengue, it is a significant concern in the context of arboviruses circulating6.
Furthermore, the mobility of populations within and across borders presents a significant challenge to Chikungunya control efforts in Latin America. Migration, trade, and tourism contribute to the rapid dissemination of the virus, which has been analyzed in some countries of the region7. High levels of human movement facilitate the introduction of the virus into new areas where susceptible populations may lack immunity, leading to outbreaks and epidemics8
Effective surveillance systems and cross-border collaboration are essential for early detection and response to imported cases, preventing the establishment of sustained transmission chains. As public health professionals, policymakers, researchers, and stakeholders, your role in this is crucial. Moreover, addressing migration's social and economic drivers, such as poverty and conflict, can help mitigate the underlying risk factors for Chikungunya transmission9,10.
The burden of Chikungunya falls disproportionately on vulnerable populations in Latin America, including the poor, marginalized communities, and indigenous groups11,12,13,14. Multiple studies highlight the social determinants of health contributing to the unequal distribution of Chikungunya burden, including inadequate housing, limited access to healthcare, and poor sanitation conditions11-14. These disparities exacerbate the disease's impact, leading to higher morbidity and mortality rates among disadvantaged populations. Addressing health inequities requires a comprehensive approach that integrates health promotion, access to healthcare services, and social welfare programs to improve the resilience of vulnerable communities and reduce their vulnerability to Chikungunya and other vector-borne diseases11-14. In addition, CHIKV may lead to chronic infection, which has been previously observed and confirmed in some countries in the region 15,16,17,18,19,20,21,22.
Inadequate healthcare infrastructure and diagnostic capacity pose significant challenges to the timely detection and management of Chikungunya cases in Latin America. Some studies highlight the limitations of current diagnostic methods for Chikungunya, particularly in resource-limited settings where access to laboratory facilities is limited23. Misdiagnosis and underreporting of cases hamper surveillance efforts and hinder the implementation of targeted control measures. Strengthening laboratory capacity, training healthcare workers, and enhancing public awareness are essential components of an effective response to Chikungunya, enabling early detection, diagnosis, and treatment of cases23.
In conclusion, the control of Chikungunya in Latin America presents multifaceted challenges that require a comprehensive and coordinated response from governments, healthcare systems, and communities7. Addressing environmental, social, and healthcare factors is essential for mitigating the disease's impact and preventing future outbreaks. By investing in vector surveillance and control, strengthening healthcare infrastructure, and addressing health inequities, Latin American countries can enhance their resilience to Chikungunya and improve the health and well-being of their populations24.
Table 1 Chikungunya cases by country or territory in 2023, according to the Pan American Health Organization (https://opendata.paho.org/en)
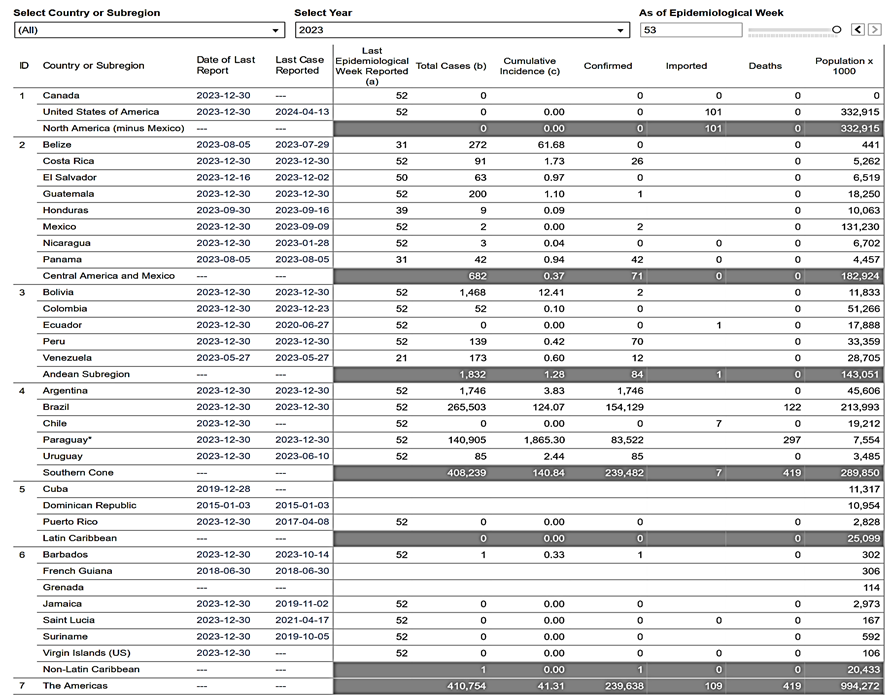
Table 2 Chikungunya cases by country or territory in 2024 (first trimester), according to the Pan American Health Organization (https://opendata.paho.org/en)