INTRODUCCIÓN
Spirometry, while considered the gold standard for diagnosing and monitoring obstructive pulmonary diseases in children, is not widely utilized in daily medical practice1. Studies indicate that only 30% of children with asthma and 50% of those hospitalized for asthma receive functional testing during follow-ups2,3. This overreliance on primary clinical skills in primary care may contribute to the overdiagnosis of bronchial asthma. Objective measures, like spirometry, could play a crucial role in addressing this issue4.
In addition to the social, economic, and cultural factors influencing prescribing habits, there are two crucial variables to consider in ensuring the reliability of this diagnostic tool. Firstly, there is a need to develop a method for obtaining more accurate forced expiratory maneuvers. Secondly, it's essential to ensure that the measurements and values align with the parameters outlined in the most commonly used reference equations.
Obtaining high-quality forced expiratory maneuvers requires attention, cooperation, and coordination, particularly in certain age groups such as children. It's worth noting that variable rates of acceptable testing are reported in this demographic, emphasizing the critical nature of achieving accurate results in these cases5,6.
Representativeness is a crucial aspect to consider when establishing reference values for spirometric tests. The concept of having a unified source for these values aims to resolve debates regarding the most suitable parameters for categorizing respiratory diseases across different regions of the world. The Global Lung Function Initiative (GLI), led by the European Task Force, has extracted predictive values from a diverse range of ethnicities, including Caucasians, African-Americans, Asians, and others. This multi-ethnic approach, coupled with a wide age range and the innovative z-score interpretation method in GLI7, has been the subject of recent research. These studies have shown varying levels of agreement within adult and child populations, potentially due to inadequate representation of certain regions, such as South America, in the universal equation8,9.
Our study sought to evaluate the feasibility of conducting high-quality spirometry, the effectiveness of incentivizing techniques to enhance its performance, and the compatibility with reference equations in a school-aged population in Asuncion, Paraguay.
METHODOLOGY
A convenience sample of 140 children, from first to sixth grade, was selected from a public school in Asunción, Paraguay, whose parents received an information sheet, a health questionnaire, and a post-informed consent form. The cross-sectional study was conducted between March and April 2011 and was previously approved by the Teaching Committee of the Instituto Nacional de Enfermedades Respiratorias y del Ambiente (INERAM), a health care center of the Public Health Ministry (Paraguay).
Inclusion criteria were children aged 6-11 years who appeared healthy, without symptoms of respiratory diseases or neurological diseases that could prevent testing, and whose parents consented to the test and their inclusion in the study.
Exclusion criteria were a history of preterm birth or low birth weight, chronic respiratory disease, acute respiratory disease in the last four weeks, and home exposure to tobacco. Morbidly obese children were excluded according to WHO references10. For the purpose of equation-fit analysis, those children who failed to perform the forced expiratory maneuver were excluded.
Age was expressed in absolute numbers. If the kid was 6 months older from birth data, the greater age was recorded. Weight (kg) and height (cm) were measured using weighing scales, respectively. In accordance with the aforementioned tables and in accordance with WHO guidelines for assessing nutritional status, the body mass index (BMI = weight/height2) was also recorded.
To rule out acute viral illnesses on the study day and to confirm the data gathered from the questionnaire, a survey was conducted. The physical examination conducted prior to the test was to find no signs of cardiorespiratory, neuromuscular, or thoracic deformity that might interfere with the subject's ability to exert themselves to their fullest potential.
The functional test was performed by an experienced physician (O.A.) with a portable spirometer (Easy-One, NDD Medical Technologies, Zurich, Switzerland), calibrated before the study with a 3L syringe and attachable to a laptop computer.
The following parameters were evaluated: forced vital capacity (FVC) and forced expiratory volume in the first second (FEV1). The volume-flow and volume-time curves were also recorded as part of the test acceptability evaluation, together with an extrapolated volume of 5% of FVC and a minimum 3-second breath-hold as end-of-test criteria in < 10-year-old children and 6 seconds in those ≥ 10-year-olds, in accordance with ATS/ERS requirements11.
The effectiveness of incentive software (child blowing balloon cartoon, NDD Medical Technologies, Zurich, Switzerland) in achieving quality tests was evaluated. All those who did not get acceptable maneuver quality were asked to perform soft exhalation maneuvers in a brief play period with a blow whistle roll. After a rest period, the relative frequencies of grade A or grade B maneuvers (a 150 ml or 200 ml difference between FVC and FEV1, respectively) obtained before and after the incentive period were recorded. The test was performed standing and with the use of nasal forceps.
For the evaluation of the accuracy or fit of the observed FVC or FEV1 measurements, only post-incentive maneuvers graded A or B were taken. Expected parameters were extracted from the equations of GLI12 and from references proposed by Zapletal13, Polgar14, Quanjer15, Hankinson16, Knudson17, Perez-Padilla18, and Rosenthal19 and included in a previous version of Spirxpert software (GLI, European Respiratory Society, 2006). The expected values were subtracted from the values observed in the spirometry performed on each child to obtain the difference, or "error". The closer the difference is to zero, the greater the accuracy of the equations, and it was considered a good fit when the expected values were 100 ml or less from the observed values.
Comparison of observed and predicted values, as well as the more reliable statistical technique known as the z score, were used to evaluate the fit of equations. The z score measures how close or how far the values obtained are, in terms of standard deviation, from the reference values (the z score is calculated by the ratio of the difference between the measured value and the predicted value with the residual standard deviation). The data was broken down into sex and age categories.
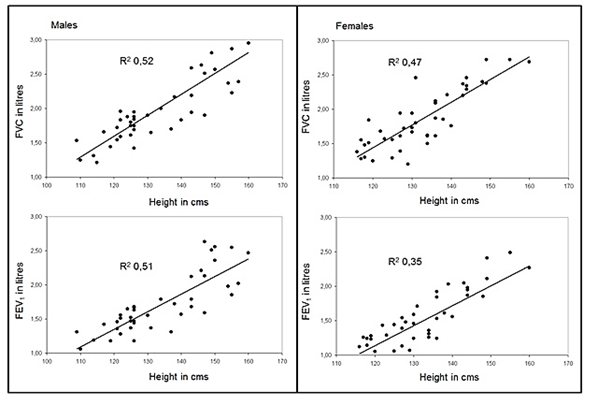
For the descriptive analysis, anthropometric data (gender, age, weight, and height) and functional variables (FVC and FEV1) are described. The scatter plot graph has been used, to evaluate the linear relationship between height and the values of FVC and FEV1 through the coefficient of determination (R2) that provides the model's goodness of fit.
To analyze the statistical difference between the measured value and the expected value of FEV1 and FVC, a t-test for related samples was performed. The same test was employed to analyze the difference between measured FVC and FEV1 and predict values expressed as GLI-2012 z-scores. The SPSS statistical package (v 11.5) was used for inferential analysis. The significance level was set at p<0.05.
The teaching committee of the Instituto Nacional de Enfermedades Respiratorias y Ambientales accepted the protocol's cross-sectional structure and ethical considerations (INERAM).
RESULTS
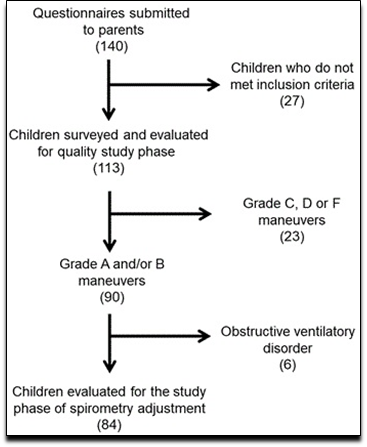
Out of the 140 schoolchildren chosen, 113 (48 men) participated in the study of acceptability. Due to denial of permission, asthma, or a recent history of an upper respiratory infection, 27 kids were not included (Figure 1).
When applying incentive software, the frequency of acceptable and reproducible grade A and grade B maneuvers was observed in 58.4% of cases (n = 66). Between 6 and 7 years old, the proportion of grade C, D, or F maneuvers was significantly higher. After the blow, whistle, and roll phases of play motivation, the overall percentage of high-quality spirometric tests was 79.6% (n = 90).
To assess the fit of the equations, 84 children (42 boys and 42 girls) who performed high-quality maneuvers were studied. In Table 1 the anthropometric features and functional test results are presented.
Table 1. Distribution, anthropometric and spirometric data of 84 school children in Paraguay according to three age groups.
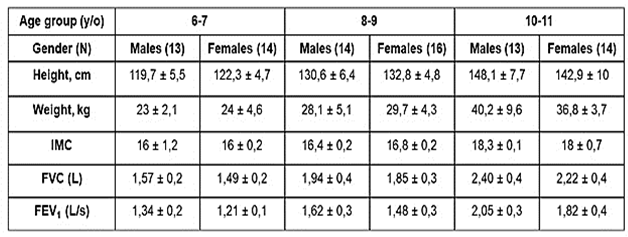
In both sexes, spirometric parameters rise with age and height, with varying degrees of dispersion. A non-uniform distribution may be seen when the relationship between these values and height is plotted, with FEV1 having the most pronounced non-uniformity in females (Figure 2).
The coefficient of variation, which represents the inter-individual variance of the expiratory maneuvers, was on average 16,4% (range 13,2 to 19,6%) for FVC and 16,7% (range 12,2 to 19,4) for FEV1 for boys. The FVC and FEV1 of the girls in the sample were 14,6% (range 10,3 to 18,3%) and 14,2% (range 11,9 to 18,5%), respectively.
When comparing the values predicted by the Zapletal, Polgar, Quanjer, Hankinson, Knudson, Perez-Padilla, and Rosenthal equations with the values measured in our population, we note that there are significant (p 0.05) scattered differences for the FVC, the FEV1, or both. The values predicted by the GLI did not present differences when compared with the measured parameters (Figure 3).
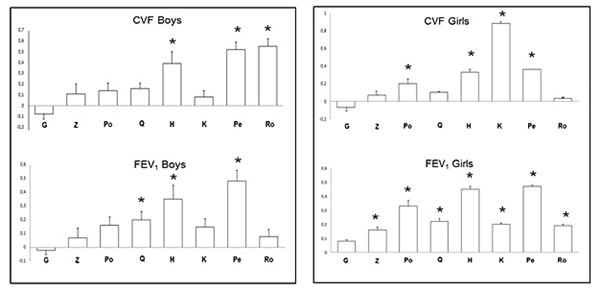
Mean and standard error of the difference between the observed and expected value for forced vital capacity, expressed (FVC) and forced expiratory volume in one second expressed (FEV1) using the equations of Global Lung Initiative (G), Zapletal (Z), Polgar (Po), Quanjer (Q), Hankinson(H), Knudson (K), Perez-Padilla (Pe) and Rosenthal (R). *p< 0,05.
Figure 3. Differences between Expected and Measured Values According to Most Used Equations in Spirometry in School Children from Paraguay.
Except for the GLI, there are absolute differences of more than 100 ml between the measured values and the values predicted by all of the equations tested (Table 2).
Table 2. Agreement between the Observed Values of FVC and FEV1, and Those Expected by the Prediction Equations in schoolchildren
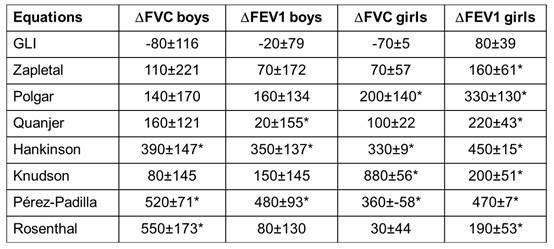
The mean of the differences was obtained by subtracting the predicted value from the measured value and expressed in milliliters for forced vital capacity, expressed (FVC) and forced expiratory volume in one second (FEV1) using the equations of Global Lung Initiative (GLI), Zapletal, Polgar, Quanjer, Hankinson, Knudson, Perez-Padilla and Rosenthal. * p< 0,05.
When all of the spirometric variables are reported as GLI 2012 z-scores, the measured variables for both sexes exhibit significant but inconsistent changes when compared to the projected values. The Hankinson and Knudson estimates are the exception.
Table 3. Differences between measured FVC and FEV1 and predicted values expressed as GLI-2012 z-scores in school children of Paraguay
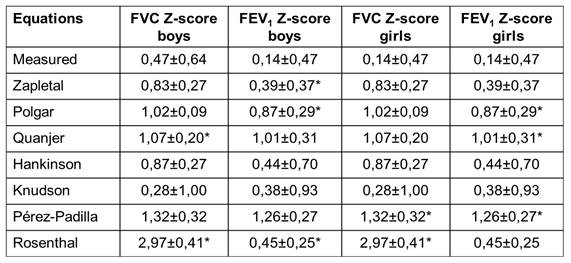
Z-scores of measured and predicted values were obtained using GLI (Global Lung Function Initiative) software and are expressed as mean ± standard deviation. Forced vital capacity, expressed (FVC) and forced expiratory volume in one second (FEV1). Zapletal, Polgar, Quanjer, Hankinson, Knudson, Pérez-Padilla and Rosenthal. *p<0,05.
DISCUSSION
The prevalence of asthma, the most common chronic respiratory condition in children, has a substantial adverse impact on the quality of life of children and is a significant driver of healthcare resource utilization20. Current therapeutic practices for this patient population often fall short of recommended standards, particularly due to the underutilization of spirometry, which is considered the gold standard for diagnosis1,21. Surprisingly, spirometry is only utilized by a limited percentage of primary care doctors (12%-75%) and pediatricians (25%-50%) across different countries, with a significant lack of confidence in interpreting these test results22,23. This reliance on clinical history alone may lead to a failure to detect a substantial proportion of obstructive airway disorders, resulting in potential overdiagnosis and unnecessary treatment24. As a result, it is crucial to recognize the limitations of relying solely on clinical history and to prioritize the adoption of spirometry to improve diagnostic accuracy and reduce the risk of overdiagnosis25.
There are several reasons why the use of this diagnostic test is limited, such as its cost, difficulty in interpretation, lack of time in the office, equipment availability, and patient difficulties in performing the test22. To achieve accurate respiratory maneuvers, cooperation and collaboration are necessary. However, this can result in varying percentages of technically acceptable outcomes, particularly in children, who benefit from the use of techniques to optimize forced expiration exercises. Improving spirometry standards in children can be achieved through additional training time and the utilization of incentive computer applications. By investing in these areas, healthcare providers can improve the accuracy and reliability of respiratory assessments in pediatric patients, ultimately leading to better overall care.
There is debate over the data generated by stimulation software. Gracchi and cols. have found that the prior use of these resources can negatively impact the reproducibility and performance of forced expiratory maneuvers26, while Vilozni and cols. were able to achieve better results when comparing two different animation software27. In this study, we adhered to the most recent recommendations for spirometry standardization and utilized this resource consistently in our bilingual population28. Only 58.4% of the people had tests that were acceptable and reproducible across the board and without training prior to the experiment. According to Tomalak et al., only 50.21 percent of the 233 children under the age of 10 who participated in the study fully cooperated. The most common reasons for test failure included improper breathing techniques, a lack of a peak in expiratory flow, respiratory effort variables, and even a lack of interest. Only 23,9%, even the ones who were cooperative, were able to exhale for more than three seconds. The maneuvers were performed without any training or computational incentives6. In 109 spirometric tests conducted on kids between the ages of 6 and 15, Zanconato et al. obtained unacceptable results in 22% of the cases and incorrect interpretations in 21% of the cases. However, prior instruction or rewards before or during the execution are not entirely clear29. The same spirometer model was used in a sample of 3,133 healthy children between the ages of 4 and 18, and it was discovered that 82.6% of those children met the extrapolated volume and reproducibility criteria. However, when the end-of-test criterion was added, the quality of the spirometry dropped to 39.7%30. Compared to 92% of tests completed in pulmonary function laboratories, 63% of spirometry tests conducted by patients at home met valid technical criteria31. This suggests the significance of a technician's or professional's assistance and/or the necessity of a set training period supported by amusing stimuli and/or assistance software, for proprioceptive training and audiovisual feedback, seeking to maximize performance. Van Delden et al. recommend a set of requirements for incentive metaphors-the authors' term for computer programs-along with a number of optional games in order to produce high-quality results32.
A prior training period is not usual before performing spirometry and this aspect leads our experiment to a real practice field with an interesting practical proposal. A game period was used with the blow whistle roll in the sample that was examined here, but only for those who did not pass the test the first time. With this action, the percentage of acceptable and repeatable results rose to 79.6%. The rate of achievement in specific populations may be further optimized by home training recommendations given prior to visiting the pulmonary function laboratory and/or after failing to pass a quality test on the test day. Arets et al. used computer applications to obtain > 90% extrapolated volume and 15.3% forced expiratory time as end-of-test criteria in 446 schoolchildren who, on average, had previously undergone at least two spirometric tests. In other words, the people were already trained33.
The national literature lacks analyses that effectively align reference parameters with spirometry test results in Paraguayan children, potentially leading to confusion in diagnosing and treating obstructive lung diseases. Among the eight equations tested, the values provided by GLI were deemed the most suitable for this study due to their minimal difference between expected and observed values, which was not statistically significant. Hall et al. considered a z score difference > 0.5 in FVC or FEV1 values between sexes significant when using the Zapletal, Polgar, Quanjer, Pérez-Padilla, and Rosenthal equations34.
GLI predicted values are obtained by more reliable statistical methods (Generalized Additive Models of Location, Scale, and Shape, or GAMLSS) rather than linear regression models like Rosenthal et al., which is one of the reasons for better adjustment35. GLI was developed using data from different ethnic groups and a continuous age distribution rather than an age group like Hankinson36,37.
The FVC and FEV1 values obtained from children in France38, Australia34, England39, and sub-Saharan Africa40 are consistent with the GLI reference values, according to two studies38,39. These prediction equations, however, do not accurately match the spirometric data from children from Taiwan41, Jordan42 and Brazil43.
In order to turn auxiliary techniques into trustworthy instruments for decision-making, numerous epidemiological studies on children's lung function have emerged in other nations. The use of the lower limit of normality (LLN) rather than predetermined cut-off points to establish diagnostic thresholds suggests a greater degree of individual adjustment, taking anthropometric and demographic information into account. On the other hand, using the Z score as a tool for expressing results and a measure of dispersion has the benefit of allowing value comparisons across gender, height, age, and ethnicity44.
Our study has some limitations. The sample comes from one educational institution in the capital, which makes it difficult to extrapolate the results. It is critical to conduct studies with larger samples that take into account the rural, urban, and ethnic diversity of our nation. The ATS/ERS technical recommendations for spirometric quality have recently been updated, but it should be noted that the technical standard for "forced exhalation" (variation of 0.025-L in 1 second or forced exhalation time of 11-15 seconds, or failure to continue from exhalation to a plateau) is mostly derived from 28 studies in adults 28.
We conclude that: a) most of the schoolchildren perform good forced expiratory behaviors; b) the playful nature of the experiment significantly increases the percentage of participants that perform acceptable and repeatable exercises; and c) GLI reference values are those that best match in this cohort.