Introduction
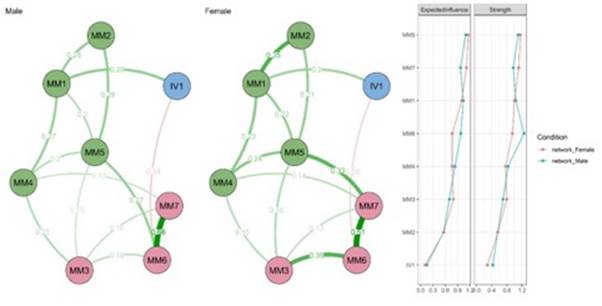
The COVID-19 pandemic has caused a strong pressure on the health systems of different countries, which has had an impact on the increase of emerging or re-emerging infectious diseases, as is the case of Monkeypox1. Monkeypox is a zoonotic disease caused by the Monkeypox virus, a type of orthopoxvirus that belongs to the same family as variola, which causes smallpox2. Symptoms include maculopapular rashes, mainly on the hands and feet, headache, swollen lymph nodes, fever, chills, and myalgia3. While clinically Monkeypox has less severity than smallpox4, its mortality rate varies around 3% to 6 %5. After 39 years without the disease being diagnosed in humans, an outbreak of 118 cases of Monkeypox was identified in Nigeria during 2017 and 20186. In early May 2022, a new outbreak of Monkeypox was identified in several countries in Europe, North America, and Australia, where the disease is not endemic7. Prior to this outbreak, cases of Monkeypox were uncommon outside endemic countries in central and west Africa8. In response, WHO declared Monkeypox a Public Health Emergency of International Concern (PHEIC) on July 23. As of September 28, 2022, more than 67,000 confirmed cases of Monkeypox have been reported worldwide and 27 deaths from the disease, with numbers continuing to rise9 (Figure 1). In South America, also as of September 28, 2022, 13,495 diagnosed cases of Monkeypox and 3 deaths from the disease were reported. In this region, Brazil (n= 7534 cases), Peru (n= 2436 cases) and Colombia (n= 2042 cases) were the countries with the highest number of reported cases (Figure 2).
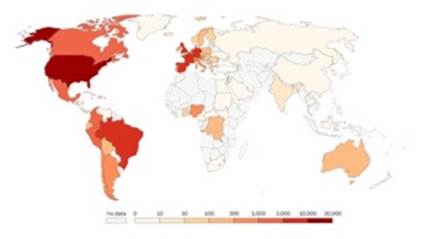
Figure 1 Monkeypox: accumulated confirmed cases worldwide, sep 28, 2022. Based on data from our world in data.
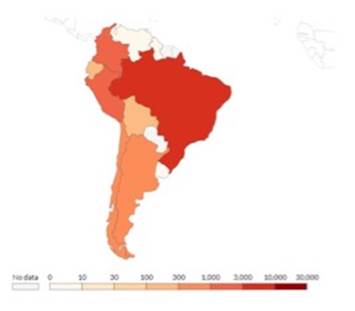
Figure 2 Monkeypox: accumulated confirmed cases in south america, sep 28, 2022. Based on data from our world in data.
One of the strategies to control the current Monkeypox outbreak is the vaccination of the population against the disease, which is being carried out in some countries in Europe, the USA and Canada10. In these countries, a "ring vaccination" is being carried out with vaccines against smallpox, which are effective against Monkeypox due to the relationship between the viruses of both diseases10. Indeed, it has been reported that smallpox vaccines can provide cross-protection (immunity to one disease provides immunity to the other) against Monkeypox in 85% of cases11. Currently, cidofovir, brincidofovir (CMX001), tecovirimat (ST-246) and immunoglobulin vaccinia (VIG) and JYNNEOS™ (Imvamune or Imvanex) are administered, while the live vaccine ACAM2000 is under trial testing12. Therefore, there would be a higher incidence rate of Monkeypox among unvaccinated people13. Information on the efficacy of the vaccines used against Monkeypox is obtained from in vitro, animal studies and clinical trials demonstrating their immunogenicity in humans. However, current vaccines are not specific for the virus causing Monkeypox; moreover, their efficacy on the recent outbreak has not been fully confirmed10.
The current COVID-19 pandemic has emphasized the importance of worldwide vaccination to protect people against emerging and/or re-emerging infectious diseases, such as Monkeypox. The success of any vaccination program will depend on the acceptance of the population to be vaccinated. However, convincing the population to accept vaccination remains a major challenge and one of the top ten threats to global public health. Intention to vaccinate involves willingness and acceptability to vaccinate, as well as positive attitudes toward the vaccine administered, as opposed to resistance or refusal to vaccinate14. A recent survey of health care workers indicated that 55.4% were likely to receive the Monkeypox vaccine and 79% would accept it if it were recommended to the general population15. Another study with a U.S. sample indicated that 46% would receive a Monkeypox vaccine if it were recommended to them, 29% would refuse to receive it, while 25% were hesitant16. Finally, another study conducted in the Netherlands indicated that 72% had a high intention to be vaccinated17. The above data would indicate the presence of a significant percentage of people who would refuse or hesitate to be vaccinated against Monkeypox. As in the COVID-19 pandemic, this would threaten collective immunity against the disease18. In Peru, it has been reported that Monkeypox vaccines are expected to arrive at the end of September. In this sense, together with the arrival of the Monkeypox vaccine, efforts should also focus on its acceptance to achieve immunity of the entire population.
There are different factors associated with the intention to vaccinate. Previous studies have shown that emotional factors, and in particular fear of disease, significantly influence the way people behave in the face of vaccination campaigns19. It has been indicated that fear, rather than cognitive risk assessments, drive health behaviors20. Specifically, it has been suggested that fear of an infectious disease is positively related to vaccination intentions19,21,22. It appears that people with higher levels of fear perceive disease as a threat to their health or those of their loved ones. Therefore, these people would be more willing to get vaccinated to protect themselves and their loved ones against disease. This is important considering that about 62% of the general population reported being more concerned about Monkeypox than COVID-1923. Although Monkeypox has a low overall mortality rate, there are aspects that have generated concern and fear, such as the similarity with the smallpox virus, the high number of reported cases, the lack of direct relationship between outbreaks and travel from endemic regions, the lack of clarity about the development of a greater capacity for human-to-human transmission of the virus, the rapid geographical spread, the lack of data on the effectiveness of available antivirals in treatment, among others24,25. It has been suggested that the presence of fear of an infectious disease triggers psychological factors associated with perceived behavioral control over vaccination acceptance, subjective norms of vaccination acceptance, attitudes toward vaccination acceptance, and perceived infectiousness from disease26.
Based on the above, the current study assessed how intention to be vaccinated against Monkeypox specifically relates to symptoms of Monkeypox fear in a sample of Peruvian citizens using network analysis. Specifically, we aim to (a) identify the interrelationship between the nodes of both variables; (b) identify the main nodes in each variable; and (c) compare the networks according to sex, which will allow us to identify whether the networks are invariant and the level of connection at which the networks can be considered almost identical. Network analysis is useful for visualizing the interaction between elements of a network, including symptoms of a syndrome or patterns of behaviors27. This type of analysis is based on the hypothesis that symptoms or nodes are interdependent and that a mental health problem is made up of a network of symptoms that interact with each other28,29. The relationships between the nodes or symptoms are the edges. Statistically significant edges would not indicate that the symptoms are influenced by underlying latent variables; rather, the symptoms directly influence each other30. If symptoms interact with each other, some variation in a central symptom will generate changes in other symptoms. However, it should be kept in mind that, in cross-sectional designs, network analyses suggest, but do not determine causality. Although, as mentioned, the presence of significant edges suggests causal influences, experimental designs are necessary to determine causality. Therefore, performing a network analysis provides information to support causal hypotheses between variables within a network.
Network analysis has been used to understand the relationship between different variables associated with mental health during the COVID-19 pandemic, both in Peru and other Latin American countries31,32,33. However, as far as is known from the literature, this technique has not been used to assess mental health symptoms and health behaviors during the Monkeypox public health emergency in any Latin American country. The importance of the study lies in the fact that the identification of symptoms or central nodes, which is characteristic of a network, would allow to identify which nodes to target during clinical intervention34.
Methodology
Participants
There were 506 participants with an average age of 27.11 years (SD = 9.77); 192 males (37.20 %) and 324 females (62.80 %), selected by snowball convenience sampling. Of the participants, 81.2% were married, 8.7% were single, 7% were divorced, 2.3% were widowed, and 0.8% were living with a partner. Likewise, the majority (49.1%) were unemployed at the time of answering the survey, 32.8% had a permanent job, 23.4% had a temporary job and 3.7% were retired. Regarding educational level, 38.2% had incomplete primary education, 28.9% had completed primary education, 20.5% had completed university studies, 8.3% had completed secondary education, 2.1% had incomplete university studies, 1.6% had incomplete secondary education, while 0.4% had incomplete technical studies. Only two people (0.4%) reported having been infected with Monkeypox and 12 reported knowing someone infected with the disease (2.3%). Regarding previous vaccination against COVID-19, 98.8% reported having been vaccinated against the disease. Of those vaccinated, 85.8% indicated that they had received full doses of vaccine, plus booster doses.
The sample was estimated a priori using the 'netSimulator' function35 by varying the sample size between 100, 250, 500, 1000; resulting those 250 data achieved a correlation between the true and estimated networks above 0.80 for the network weights; then, the study exceeded the minimum necessary to perform network analysis. The selection method was non-probabilistic and purposive.
Instruments
Fear of Monkeypox
The Monkeypox Fear Scale (MFS36 was used to measure symptoms of fear of the Monkeypox. The MFS is composed of seven items grouped into two factors: emotional and physiological reactions to Monkeypox fear. Each item presents five Likert-type response options ranging from 1 = strongly disagree to 5 = strongly agree (Appendix 1). A total score for each of the two factors can be obtained from the sum of the scores of the component items. Thus, a higher score would indicate a presence of emotional and physiological reactions to the fear of Monkeypox. In the present study, the reliability estimates for the factors emotional reactions (ω = 0.83) and physiological reactions (ω = 0.89) are high.
Intention to be vaccinated against Monkeypox.
The following single question was used: "How likely are you to receive a Monkeypox vaccine when it becomes available?" constructed ad hoc for this study. Participants answered the question on a five-point scale: 1= very unlikely; 2 = somewhat unlikely, 3 = unsure, 4 = somewhat likely, 5 = very likely. A higher score indicates a greater intention to vaccinate against Monkeypox. A continuous scale was used, and responses were not grouped as acceptance, hesitancy, or resistance, as this allows for a more accurate understanding of intention to vaccinate. Grouping participants who indicate any response between "somewhat unlikely" and "somewhat likely" could reduce the unique variation to be assessed.
Procedure
This cross-sectional study was conducted in Lima between August 21 and September 10, 2022. An online questionnaire containing sociodemographic questions, the MFS, and the single question of intention to be vaccinated against Monkeypox was constructed using the Google Form. The online questionnaire was shared through different online platforms (e.g., WhatsApp, Facebook, Instagram) and email. The study was part of an international project on mental health in a post-pandemic period that involved different Latin American countries, including Peru. This project was reviewed and approved by the Institutional Committee for the Protection of Human Subjects in Research (CIPSHI) of the University of Puerto Rico (No. 2223-006). All participants gave their informed consent electronically before answering the questions in the online questionnaire. The anonymity of the participants and the confidentiality of the data were assured, as well as respecting their right to withdraw from the research at any time.
Data Analysis
Data analysis was performed with the R programming language in its RStudio environment. The analysis was performed with the psychological network model30. The sequence of the analysis had as reference what was proposed by Fried et al.37 performing the estimation, stability, and accuracy of the network.
Estimation was performed with the ggmModSelect function, and a Spearman correlation matrix given the ordinal nature of the data38. Centrality was performed using Strength which has been shown to be the most stable39. Other typical measures of centrality such as betweenness and closeness were not used because they present difficulties of interpretation in the field of psychology40 and empirically they are very unstable39.
Accuracy and stability were examined through resampling techniques with the 'bootnet' library. Accuracy consisted of estimating a model several times with the data and calculating a value for the edges. That allowed generating 95 % confidence intervals whose width indicates accuracy (Epskamp et al., 2018). Stability was obtained by a procedure where cases are eliminated until 30% of the data is left and the relationship between true centrality and the resampled values is tested. The resulting value is captured in a coefficient called CS, which can be between 0.25 ≤ CS ≤ 0.5041.
The comparison was according to sex using the 'NetworkComparisonTest' library (NCT)42. The NCT uses a permutation procedure in which group differences are examined using 1000 randomly obtained replicates and its null hypothesis is that both groups are equal.
Results
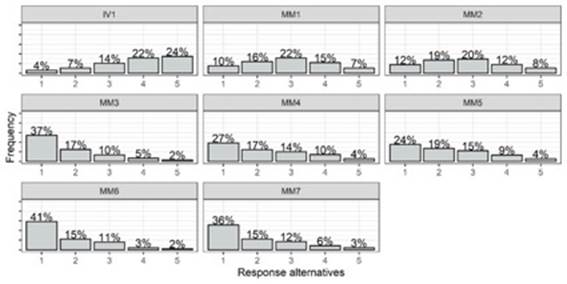
Figure 3 shows the response rates for each of the items. It is observed that the item of intention to vaccinate against monkeypox (IV) has a tendency towards high scores. In the case of the scale fear of monkeypox, items 1 and 2 have a predilection for alternative 3 ("Neither agree nor disagree"); while the rest of the items have a tendency towards low scores ("Strongly disagree").
Network estimation and centrality.
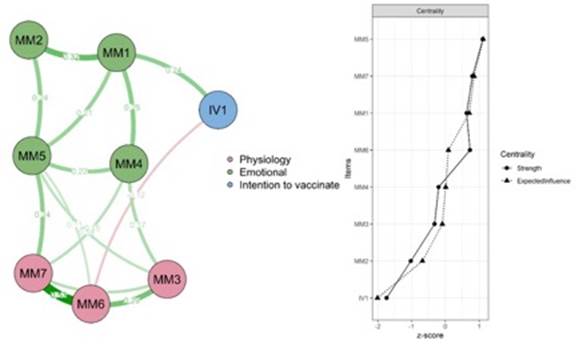
In the case of the IV item, it is observed that it is close to the items of the Emotional dimension of the fear of Monkeypox. It is evident that the edges are in the range of -.12 to .53 and that 15 of 28 edges are different from zero (53.57 % density). The edges within each community were positive. Regarding the connection between IV and the items of the monkeypox fear scale, a direct relationship is observed with MM1 ("Am I very afraid of monkeypox?") and an inverse relationship with MM6 ("How likely is it that I will receive a monkeypox vaccine when it becomes available?"). There is no relationship in the rest of the items. In relation to the centrality indexes, item MM5 is the most influential in both Strength and Expected Influence (Figure 4).
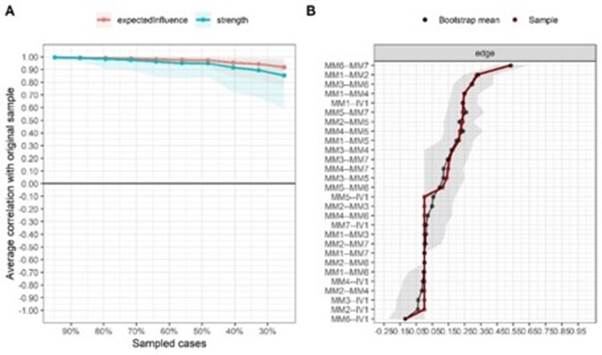
Network stability and accuracy
In relation to the stability, it is observed in Figure 5 that the fall of the lines are minimal. This reveals a stability in the centrality indices; likewise, the CS reveal 0.67 and 0.75 for Strength and Expected Influence respectively. Regarding accuracy, it is observed that the difference between the true network (red line) and the estimated network (black line) is small. In addition, the width of the 95% confidence intervals (gray band) are small.
Comparison
Broadly speaking, the networks are invariant (M = 0.33; p = .170) and connectivity does not differ (S = .12; p = .59). Likewise, the edges are related (rs = .79). However, a careful analysis shows that the relationship between IV-MM6 and IV-MM1 is higher in males than in females. Finally, the most influential node in both groups is MM5 for both Strength and Expected Influence (Figure 6).
Discussion
To the best of our knowledge from the scientific literature, this is the first study that evaluated the relationship between symptoms of fear of Monkeypox and intention to be vaccinated against Monkeypox based on a network analysis in a sample of the general population of Peru.
First, although this study did not seek to assess the prevalence of intention to vaccinate, it was observed that there is a trend toward high scores on the item of intention to vaccinate against Monkeypox. That is, most people indicated a high probability of being vaccinated against Monkeypox. This agrees with what has been reported in other studies conducted in different cultural contexts where between 46% and 72% of participants were likely to agree to be vaccinated against Monkeypox15-17. One of the factors that may have contributed to this result is that most of the participants had previously been vaccinated against COVID-19. It has been suggested that having received previous vaccinations is a predictive factor for vaccination against new diseases43. However, while intention is an important predictor of acceptance of health behaviors44, it has been suggested that intention to vaccinate is greater than actual acceptance of the vaccine45. Therefore, it is important to evaluate the factors associated with the intention to be vaccinated against Monkeypox. On the other hand, items referring to physiological and emotional reactions to fear of Monkeypox presented a tendency to low scores and expressed uncertainty regarding the presence of symptoms. Studies during previous infectious diseases suggested that the threat of infection posed by viruses can generate fear46,47. However, it is possible that the experience of the previous COVID-19 pandemic and the vaccination strategy implemented in is a possible reason for the low levels of fear experience of this new infectious outbreak in the Peruvian sample.
Fear is a normal response in infectious disease situations that minimizes people's engagement in risky behaviors and can promote responses that mitigate viruses48,49. In this sense, the results suggested that the emotional symptoms of fear were found to be closer to the intention to be vaccinated against Monkeypox. This may be expected since, during previous infectious diseases, a greater presence of emotional fear reactions has been observed in the Latin American population rather than physiological reactions50. It has been suggested that physiological symptoms are more characteristic of severe degrees of fear51. The findings would allow researchers and health professionals to distinguish between fear and its symptoms more closely associated with the intention to be vaccinated against Monkeypox. Specifically, it was observed that the strongest and most direct relationship occurred between intention to vaccinate and the item directly referring to fear of Monkeypox (I am very afraid of monkeypox). From the protection motivation theory, it has been indicated that fear triggers a perception of vulnerability, defined as the perception that a person has of possibly becoming infected, which results in an intention to protect oneself, such as the acceptance of being vaccinated against a disease, in this case Monkeypox52,53. Another study showed a mechanism that attempts to explain the association between fear of an infectious disease and intention to vaccinate, where psychological factors of perceived behavioral control contribute to people's intentions to vaccinate against the disease26. On the other hand, the intention to be vaccinated against Monkeypox was inversely associated with the item "I can't sleep because I worry about getting monkeypox". That is, the presence of sleep problems would decrease the intention to vaccinate. In periods of previous infectious diseases, sleep problems caused by worry about being infected are clinically relevant indicators for the development of fear of the disease in Latin American countries50. This finding can be explained by the Terror Management Health Model54, where people who experience fearful states, which generate sleep problems, can cope with proximal, direct, and rational defenses that eliminate the dangerous stimulus, in this case the Monkeypox vaccination.
The relationships between the intention to be vaccinated against Monkeypox and the two fear symptoms mentioned are higher in the male group compared to the female group. This is in line with what has been reported in Peru, where men are one of the groups most at risk of infection. According to the Monkeypox Situation Room of the Ministry of Health, 98.1% of the confirmed cases of Monkeypox occurred in men55. In this sense, the fact that men are more likely to be infected and experience adverse health consequences from Monkeypox could generate a greater perception of risk and fear, which would predict compliance with preventive measures, such as vaccination against an infectious disease56,57. Like other studies, this finding would suggest that it is fear of infectious disease, not gender per se, that would generate differences in preventive behavior58. In addition, these gender differences may reflect state-dependent changes rather than stable personality traits59,60. These results suggest that communication strategies about Monkeypox and the vaccination process against the disease may have a differential impact according to gender and should consider these differences.
On the other hand, the symptom "When I see news and stories about monkeypox on social networks, I get nervous or anxious" is the most central and influential symptom within the Monkeypox fear symptom network. That this symptom is the most central and influential has also been observed in a previous study on fear of COVID-19 where four South American countries participated, including Peru,50) participated and in other studies conducted in the Netherlands, Iran, Bangladesh, and Norway during the same pandemic61,62. Thus, this symptom would be characteristic of periods of infectious disease and could trigger or maintain the other symptoms of Monkeypox fear. It has been suggested that concerns about infectious diseases are related to the compulsive search for verification of information63. In this sense, the large amount of real-time information about the disease, in many cases erroneous, would generate more fear about its consequences64,65. The unlimited exchange of information through different media is a constant public health concern66. A recent study indicated that 52% of tweets about Monkeypox were misinformation or unverifiable information, another 20% were humorous information, and only 28% were serious information about the disease; furthermore, the most frequent misinformation was that the current Monkeypox outbreak is not real and is part of a series of conspiracies67. The exchange of misinformation can result in stigmatization of the most at-risk groups68. Although respondents seem to be more complacent about the imminent outbreak of Monkeypox in Peru, policy makers and public health professionals should support greater awareness and sensitization of Monkeypox69.
It is important to recognize several limitations of this study. First, the cross-sectional design of the study would not allow us to infer causal relationships and variations between fear of Monkeypox and intention to be vaccinated against Monkeypox over time. The symptom networks of Monkeypox fear and intentions to be vaccinated against Monkeypox may change over time and disease progression within a group of people. Second, the generalizability of the findings may be limited to Peruvian participants during a particular phase of the Monkeypox public health emergency of international concern. Data collected during a different period may generate other network structures among the variables. Third, the use of non-probability snowball sampling would limit the representativeness of the sample and the generalizability of the results to the general Peruvian population. Fourth, the assessments of symptoms of fear of Monkeypox and intention to vaccinate were made with self-report measures, so the presence of social desirability biases that may influence the results cannot be ruled out. Fifth, no data were obtained before Monkeypox was declared a public health emergency of international concern. This prevented comparisons of the networks between different stages of the disease. Finally, there can be no assurance that the results of the study can be generalized to adults in other Latin American countries or future infectious disease periods.
Despite the limitations, the findings may encourage researchers and health professionals to consider the importance of individual symptoms of fear of Monkeypox and their relationships to intentions to vaccinate against the disease. Also, the study has important implications for treatment. In this regard, the presence of highly consistent and reliable core symptoms, as well as stable connections between Monkeypox fear networks and intention to be vaccinated against Monkeypox in groups of men and women, highlighted the importance of long-term monitoring of Monkeypox-associated mental health. There is also potential utility in addressing specific symptoms of Monkeypox fear in interventions designed for the general population of Peru. In this sense, it would be possible to prevent the presence of these symptoms among people who do not intend to be vaccinated against Monkeypox and to treat those who currently suffer concurrent Monkeypox fear symptoms. This would challenge the idea that all Monkeypox fear symptoms have the same impact on the intention to be vaccinated against it. Identifying that the symptom "When I see news and stories about monkeypox on social media, I get nervous or anxious" is the most central, would justify the development of interventions that provide accurate and reliable information about the disease and vaccination through social media, with the aim of combating infodemia and misinformation about the current Monkeypox outbreak. This effort would involve collaboration between public health institutions, health leaders, and social media influencers to promote Monkeypox awareness. Also, there is a need to continuously review social networks, through an alert system, to identify evolving information, the emergence of new rumors and sources of erroneous70.
In conclusion, this study is the first to identify core symptoms and mediating symptoms within the Monkeypox fear network - the intention to be vaccinated against Monkeypox in a sample of Peruvians. The findings may be useful to future studies evaluating these symptom networks in other countries to better understand the key symptoms that occur among people from different cultures and those symptoms that only occur in specific groups.