Introduction
Uveitis comprises a diverse set of clinical conditions linked by the presence of intraocular inflammation and is estimated to be responsible for 2.8% to 10% of all cases of blindness, making it a significant factor in visual morbidity1,2. The pathogenesis of these conditions involves environmental, genetic, and immunological factors and can be categorized into infectious and non-infectious causes3,4. In approximately 40% of uveitis cases, it is possible to identify an underlying disease of autoimmune origin. Conversely, various systemic diseases of rheumatological or infectious origin can manifest with uveitis symptoms3.
Infectious causes constitute a significant proportion of cases (30-50%) in developing countries. Noninfectious causes are more common in developed countries. Thorne et al reported a 91% proportion of non-infectious etiology in the United States5-7, although it should be mentioned that there is a lot of variation in the frequency reported by epidemiological studies. The most common are HLA-B27-associated disease, Fuchs’ uveitic syndrome, sarcoidosis, Vogt-Koyanagi-Harada syndrome, sympathetic ophthalmia, birdshot chorioretinopathy, multifocal choroiditis, serpiginous choroiditis, and Behçet 's disease8-10. In children in developed countries, the most common is juvenile idiopathic arthritis (JIA)11, while in non-developed countries, it is traumatic uveitis and pars planitis2.
Uveitis is a public health problem caused by ocular morbidity and blindness. Epidemiological studies of uveitis are important because factors such as age, sex, skin color, and geographical origin can influence uveitis. The comparison of studies carried out in different regions of the world and at different times allows us to establish trends and speculate relevant facts for the etiopathogenesis of uveitis and ultimately improve patient care and the health of the population in general. Several studies have shown that there are differences in uveitis patterns depending on geographic region12. In Paraguay, there are few studies of this type13. The present study aimed to contribute to the clinical-epidemiological knowledge of uveitis in this country, which is essential for doctors to establish appropriate differential diagnoses14.
Methodology
This was an observational, descriptive, cross-sectional, and retrospective study of consecutive cases. Patients aged 18 years or older with a diagnosis of non-infectious uveitis who attended the Ophthalmology Service of the Hospital de Clínicas de San Lorenzo) between January 2020 and October 2021 were included.
The data were recorded in an Excel 2019 electronic spreadsheet with the variables included in the study and subsequently analyzed using SPSS Version 22. The results were expressed as frequencies, percentages, means, and standard deviations.
The anonymity of the patients' personal data was guaranteed, and they were not included in the research results. The study was approved by the Ophthalmology Department of the Hospital de Clínicas.
Results
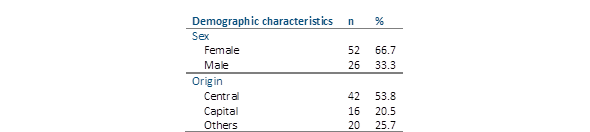
The records of patients diagnosed with non-infectious uveitis were analyzed. Of the total cases, 52 (66.7%) were female and the rest were male. The average age was 41.07 (SD±14.46) years (range, 18-67 years). A total of 42 patients (53.8%) came from the Central Department, 16 (20.5%) from the Capital Department, and the rest from other departments (Table 1).
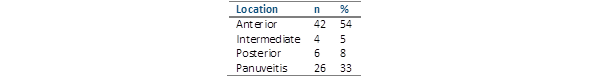
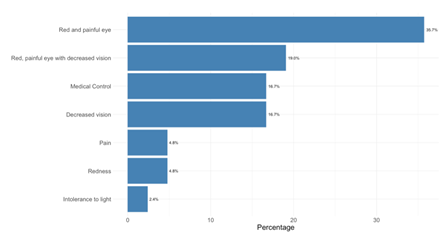
The most common anatomical location of uveitis was anterior in 42 patients (53.9%), followed in descending order by panuveitis, posterior, and intermediate (Table 2). Among the anterior uveitis cases, 24 (57.1%) were unilateral and 40 (95.2%) were non-granulomatous. Regarding the clinical course, 19 patients (45.2%) presented with an acute clinical course, 18 (42.9%) had recurrence, and the rest were chronic. The most frequent reason for consultation was “red and painful eye” with 15 patients (35.7%), followed at lower frequencies by “red and painful eye with decreased vision,” “decreased vision,” “medical control,” “redness,” “pain” and “light intolerance” (Figure 1). Regarding the systemic or ocular associations found in patients with anterior uveitis, the most frequent association was HLA-B27+ in 16 patients (38.1%), whereas idiopathic, lupus, rheumatoid arthritis, psoriasis, and sarcoidosis were found at lower frequencies. Two patients (4.8%) were diagnosed with Fuchs heterochromic iridocyclitis (Figure 2).
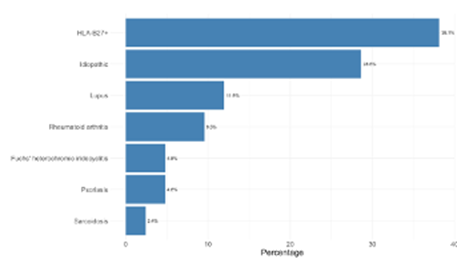
Figure 2 Patients with diagnosis of no infectious anterior uveitis by association with systemic or ocular conditions (n=42).
Regarding intermediate uveitis, two patients (50%) had unilateral uveitis, and two patients (50%) had bilateral uveitis. Regarding the clinical course, three patients (75%) had chronic disease and one patient (25%) had recurrent disease. The reasons for consultation were “decreased vision” with 2 patients (50%) and “floaters” with 2 patients (50%). Four patients (100%) had idiopathic etiology.
Regarding posterior uveitis, three patients (50%) had unilateral uveitis and three patients (50%) had bilateral uveitis. Regarding the clinical course, three patients (50%) were acute, and three patients (50%) were chronic. The most frequent reason for consultation was “decreased vision” with five patients (83.3%), followed by “floaters” with one patient (16.7%). The most frequently found systemic or ocular association was rheumatoid arthritis in two patients (33.3%), followed by lupus, vasculitis associated with ANCA-p, and idiopathic; one patient (16.6%) had a diagnosis of serpiginous choroiditis (Figure 3).
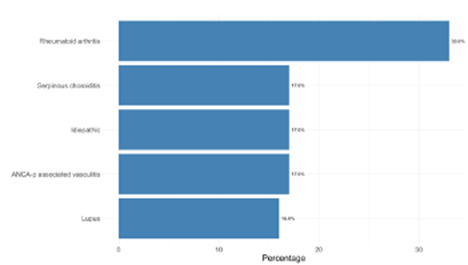
Figure 3 Patients with diagnosis of no infectious posterior uveitis by systemic or ocular associations (n=6)
Among the panuveitis cases, 19 (73.1%) were bilateral, and 14 (53.9%) were granulomatous. Regarding the clinical course, 17 patients (65.4%) had chronic disease, eight patients (30.8%) had acute disease, and one patient (3.85%) had recurrence. The most frequent reason for consultation was “decreased vision” with 9 patients (34.6%), followed by “medical control” with 7 patients (26.9%), “redness” in 3 patients (11.5%), “red and painful eye” with 2 patients (7.7%), “red and painful eye with decreased vision” with 2 patients (7.7%), “red and painful eye with decreased vision and floaters” with 2 patients (7.7%) and, finally, “eye pain” with 1 patient (3.8%). Of the total panuveitis cases, 13 (50%) were associated with Vogt-Koyanagi-Harada syndrome, while 13 (50%) had idiopathic etiology.
Discussion
This study aimed to determine the clinical and epidemiological characteristics of patients with noninfectious uveitis at a university hospital in Paraguay. The most frequent anatomical location was the anterior, a much lower percentage than that found in other studies, such as that of Thorne et al., in which 81% was anterior5, and that of Suhler et al., which reported 83.3% of anterior uveitis15, but higher than that found in the study by Nguyen et al., in which 29% of anterior uveitis was reported16, and similar to the study by Lopalco et al., which reported 54.32% anterior uveitis17. An explanation for the lower proportion of anterior uveitis in this study compared to most studies carried out worldwide could be that they are generally managed by ophthalmologists at the first level of care, and only the most complex cases reach the reference hospitals.2. Regarding laterality, most unilateral cases were observed in this study, as well as in the study by Nguyen et a16. Regarding the clinical course, most acute cases were observed, also like the study by McCannel et al18. The most frequent reason for consultation was a painful red eye, which was also observed in the study by Nguyen et al.16.
A greater proportion of non-granulomatous histological types was observed in a study by Hosseini et al.19. The association with HLA-B27 was the most frequent etiology, unlike that reported by Wakefield et al.20, who reported a higher proportion of idiopathic cases. Similar to the findings of Tsiruki et al., intermediate uveitis was the least frequent and was mainly chronic.2. The proportion between unilateral and bilateral was 1:1, similar to that reported by Nguyen et al.16, in which the proportion was almost equal. One hundred% had an idiopathic etiology, which is close to the 84% reported by Nguyen et al.16. The two equally frequent reasons for consultations were decreased vision and floaters. However, Nguyen et al.16 found that floaters were the most frequent reasons for consultation.
Regarding posterior uveitis, unilateral and bilateral uveitis were equally frequent in this study, and the main reason for consultation was decreased vision, like that found by Nguyen et al.16. Notably, the most common associated systemic condition was rheumatoid arthritis (33.3 %), while this represented only 9% in the series by Nguyen et al.16
Regarding panuveitis, a clear predominance of bilaterality was observed in this study (73.1 %), whereas in the series by Nguyen et al.16, bilaterality was observed in only 53 %. The most frequent reason for consultation, decreased vision, was also the main reason for Nguyen's series. It is striking that idiopathic etiology and Vogt-Koyanagi-Harada syndrome were equally frequent in this study, and Nguyen et al.16 reported that idiopathic etiology constituted 42% of the cases and Vogt-Koyanagi-Harada syndrome Harada only 9% of the cases, and in the Salinas study, carried out in Paraguay, constituted a very minority proportion of the cases13. One explanation could be bias due to the referral of patients to our service (ophthalmological reference center).
In relation to the epidemiological characteristics in this study, the majority of patients with noninfectious uveitis were female, and in the majority of the series carried out in the world, a predominance of the female sex has been found, such as that of Nguyen et al.16, carried out in the United States, which found a predominance of 58% of the female sex; that of Thorne et al.5, also carried out in the United States, which found a majority of 56.8% female patients. This greater predominance of noninfectious uveitis in women could be because autoimmune diseases are also more common in women21.
Most patients came from the Central Department, corresponding to the health coverage of the Hospital de Clínicas, followed by the Capital, and to a lesser extent, from other departments. This can be explained by the proximity of these places to the Hospital de Clínicas and the current availability of ophthalmological care in each department of Regional Hospitals. The average age found in this study, 41.07 (SD±14.46 years) was slightly lower than that found in the study by Nguyen et al.16, 45.16 (SD±2) years, and higher than that reported by Lopalco et al., 36.92 (SD±18.30) years17.
This study has limitations, as it is observational and descriptive, and it also has the risk of patient referral bias, making it impossible to calculate the exact prevalence of the pathologies described. However, it could be relevant for doctors to have an idea of the pathologies they expect to find in the Paraguayan population. It is suggested that studies be conducted, for example, with a prospective design, to collect more epidemiological data on these pathologies.
The clinical and epidemiological pattern observed in this study is for the most part similar to that observed in most series found in the literature. However, it is noteworthy in this study that the most frequent associations are different from those reported in the case of anterior uveitis, HLA-B27+, rheumatoid arthritis, and panuveitis; a large percentage of Vogt-Koyanagi-Harada syndrome is observed. Further studies are required to better specify these apparent differences with respect to the series from other populations.