Artículo original
Diagnostic Stability of Major Depressive Disorder in hospitalized patients in a University Hospital: a Brief Report
Estabilidad diagnóstica del trastorno de depresión mayor en pacientes hospitalizados en el Departamento de Psiquiatría de un Hospital Universitario: un breve informe
1Universidad Nacional de Asunción, Departamento de Psiquiatría, San Lorenzo, Paraguay.
2Fundação do ABC, Medical School, Department of Neuroscience, Santo André, SP, Brazil.
3University of São Paulo, Medical School, Department of Psychiatry, São Paulo, SP, Brazil.
4University of Foggia, Department of Clinical and Experimental Medicine, Foggia, Italy.
5Universidad Nacional de Asunción, Departamento de Psicología médica, San Lorenzo, Paraguay.
ABSTRACT
Introduction:
There may be a discordance between diagnoses at admission and discharge of mentally ill patients with major issues regarding their diagnostic stability. The objective of this brief report was to determine the diagnostic stability of major depressive disorder at patients’ discharge and if the diagnosis of their hospital admission had been retained.
Methodology:
This was a pilot, descriptive, cross-sectional, and retrospective observational study. A non-probabilistic sampling of consecutive cases was used. We reviewed the medical records, at admission and discharge, of patients with an initial diagnosis of major depressive disorder, hospitalized in the Department of Psychiatry of the ‘Hospital de Clínicas’ of the National University of Asunción, Paraguay, during the months of October to December 2020.
Results:
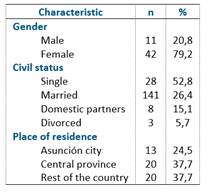
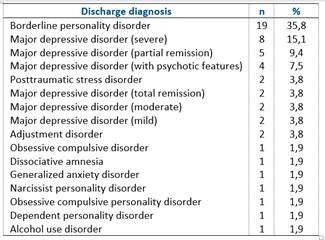
Fifty-three patients with a diagnosis of major depression on their hospital admission were included in the study (mean age = 35.7 ± 16.5 years). 79.2 % were women, 52.8 % were single, and 37.7 % were from the Central province of Paraguay. The most frequent diagnosis at discharge was borderline personality disorder, in 35.8% of cases. Major depressive disorder was confirmed in 15.1% of cases. No significant relationship was found between any discharge diagnosis and sociodemographic data.
Conclusion:
The results of this study, although preliminary, described the trajectories of diagnoses in the Psychiatry Department of a University hospital, but confirmatory studies are needed.
Keywords: diagnosis; diagnostic stability; major depressive disorder; borderline personality disorder
RESUMEN
Introducción:
puede existir una discordancia entre los diagnósticos al ingreso y al alta de los pacientes con enfermedades mentales, con problemas importantes en cuanto a su estabilidad diagnóstica. El objetivo de este breve informe fue determinar la estabilidad diagnóstica del trastorno depresivo mayor al alta de los pacientes y si se había mantenido el diagnóstico de su ingreso hospitalario.
Metodología:
se trata de un estudio observacional piloto, descriptivo, transversal y retrospectivo. Se utilizó un muestreo no probabilístico de casos consecutivos. Se revisaron las historias clínicas, al ingreso y al alta, de los pacientes con diagnóstico inicial de trastorno depresivo mayor, hospitalizados en el Departamento de Psiquiatría del Hospital de Clínicas de la Universidad Nacional de Asunción, Paraguay, durante los meses de octubre a diciembre de 2020.
Resultados:
se incluyeron en el estudio 53 pacientes con diagnóstico de depresión mayor a su ingreso hospitalario (edad media = 35,7 ± 16,5 años). El 79,2 % eran mujeres, el 52,8 % eran solteros y el 37,7 % eran del Departamento Central del Paraguay. El diagnóstico más frecuente al alta fue el trastorno límite de la personalidad, en el 35,8% de los casos. El trastorno depresivo mayor se confirmó en el 15,1% de los casos. No se encontró relación significativa entre ningún diagnóstico al alta y los datos sociodemográficos.
Conclusiones:
los resultados de este estudio, aunque preliminares, describen las trayectorias de los diagnósticos en el Departamento de Psiquiatría de un hospital universitario, pero son necesarios estudios confirmatorios.
Palabras clave: diagnóstico; estabilidad diagnóstica; trastorno depresivo mayor; trastorno límite de la personalidad
INTRODUCTION
Depression is a chronic illness that can affect thoughts, mood, and physical health. It is characterized by low mood, lack of energy, sadness, insomnia and inability to enjoy life1. In Paraguay, the frequency of Depression in the Emergency Department of the ‘Hospital de Clínicas’ of the National University of Asunción is 16.75%, so it may be considered a common illness2. However, it is common that the diagnosis at admission may be not very accurate and during the hospitalization a more accurate psychiatric diagnosis is made3-5.
There may be a discordance between diagnoses at admission and discharge of mentally ill patients with major issues regarding their diagnostic stability. Many factors may contribute to the diagnostic instability, such as the clinical criteria and clinical assessment of physician involved in the admission, as well as symptoms that may occur without the presence of disorder3. The objective of this brief report was to determine the diagnostic stability of major depressive disorder at patients’ discharge and if the diagnosis of their hospital admission had been retained.
METHODOLOGY
This was a pilot, descriptive, cross-sectional, and retrospective observational study. A non-probabilistic sampling of consecutive cases was used. We reviewed the medical records, at admission and discharge, of patients with an initial diagnosis of major depressive disorder, hospitalized in the Department of Psychiatry of the ‘Hospital de Clínicas’ of the Universidad Nacional de Asunción, during the months of October to December 2020. We reviewed information on the patient’ sex (male, female), age, marital status (single, married, widower, divorced), and diagnosis at discharge (according to the 5th edition of the Diagnostic and Statistical Manual of Mental Disorders, DSM-5)6.
The sample size was calculated using the Epidat 4.2 epidemiological package (Pan American Health Organization, Galician Board of Health and the CES University of Colombia). Assuming a frequency of depression in the emergency department of 16.75% (2), a confidence interval of 95% and a precision of 10.5%, the minimum sample was set at 49 patients. Finally, the sample included 53 patients7.
Data were loaded into a spreadsheet and then processed with the PSPP statistical package. Categorical variables were summarized in the form of frequency tables, while quantitative variables were summarized with measures of central tendency and dispersion. The study was approved by the Department of Psychiatry of the National University of Asunción, School of Medical Sciences (Paraguay). Data were treated with confidentiality, equality, and justice, respecting the Helsinki principles.
RESULTS
Fifty-three patients with a diagnosis of major depression at their hospital admission were included in the study, with ages ranging from 13 to 73 years old (mean = 35.7 ± 16.5 years). 79.2 % were women, 52.8 % were single, and 37.7 % were from the Central province of Paraguay. Sociodemographic data can be seen in detail in Table 1. The most frequent discharge diagnosis was borderline personality disorder, in 35.8% of the cases. Major depressive disorder was confirmed in 15.1% of cases. Regarding the number of days of hospitalization, it ranged between 2 and 43 days (mean = 19 ± 10 days). Table 2 shows diagnoses at discharge. No significant relationship was found between any discharge diagnosis and sociodemographic data. Also, no significant difference was found between days of hospitalization and sociodemographic data.
DISCUSSION
Depression is a disorder frequently reported in the emergency departments of psychiatric units, almost always accompanied by life-threatening behaviors that require immediate intervention and hospitalization2. This research reported on the definitive diagnoses of patients who were classified at admission as affected by major depression. It is not uncommon in psychiatry that, as more is known about patient's clinical history and patient's biopsychosocial context, a different diagnosis from the initial one at admission may be made at discharge; this usually may happen for patients affected by bipolar disorder8.
In this brief report, the most frequent definitive diagnosis was borderline personality disorder, in fact 35.8% of cases admitted as major depressions were re-diagnosed as such at discharge. The overlap and convergence between these diagnoses has been discussed in the medical literature9. The reactive depressive features and depressive symptoms, as integral parts of borderline personality disorder, may easily be misinterpreted and misdiagnosed as major depression10.
Borderline personality disorder is a severe mental illness. People affected by this disorder present with intense dysregulation of emotions and impulses, an unstable sense of self and multiple difficulties in interpersonal relationships. In addition, the disorder is often accompanied by suicidal and self-injurious behaviors11. Some authors have suggested that more than 60% of patients with borderline personality disorder received other different diagnoses as their first diagnosis. Stress-related disorders and depressive disorders were the most frequent first diagnoses. These low diagnostic stabilities demonstrate that patients with borderline personality disorder are a heterogeneous group of patients diagnosed with many other psychiatric diagnoses over time12. This supports the need for prompt and accurate diagnosis.
Diagnostic stability is essential for the validation of mental disorders and serves as a basis for the prediction of their course and outcome13. However, there are several factors that lead to the re-diagnosis of patients initially diagnosed with major depressive disorder. This highlights the need for a longitudinally based diagnostic process in the diagnostic systems.
For example, patients with bipolar disorder often receive the initial diagnosis of major depressive disorder, since patients often have one or more depressive episodes before their first manic or hypomanic syndrome14. The likelihood of changing diagnosis is higher in patients with younger age of onset of their first lifetime major depressive episode, with family history of bipolar disorder, with psychotic symptoms or subthreshold hypomanic symptoms during the depressive episode, treatment resistance, and comorbid symptoms of attention deficit hyperactivity disorder or substance use disorders15,16. In the case of psychotic disorders, some studies have suggested that up to 30 percent of patients initially diagnosed with major depressive disorder eventually develop symptoms that warrant a change in diagnosis to a schizophrenia spectrum disorder17,18.
It is essential to make an accurate diagnosis in psychiatry, since this will allow establishing adequate and efficient treatments for each patient. Therefore, a good longitudinal follow-up of patients should always be carried out since many disorders may be defined on the base of their long-term outcome (e.g., bipolar disorder).
The results of this study, although preliminarily, let us to better understand the trajectories of diagnoses in the Psychiatry Department of a University hospital, even if confirmatory studies are needed.
Among limitations, it can be mentioned that the sample size is not optimal, since the error assumed in the calculation is greater than recommended. Another limitation is the type of sampling used (non-probabilistic), which prevents the results from being generalized to the general population; however, internal validity is assured, so that the interpretations are valid, as long as they are applied to the present sample.
REFERENCES
1. Cui R. Editorial: A Systematic Review of Depression. Curr Neuropharmacol. 2015;13(4):480. 10.2174/1570159x1304150831123535
[ Links ]
2. Torales J, Ventriglio A, Barrios I, Arce A. Demographic and clinical characteristics of patients referred to the psychiatry unit of the emergency department at the National University of Asunción’s General Hospital, Paraguay. Int J Cult Ment Health. 2016;9(3):233-238. 10.1080/17542863.2016.1197290
[ Links ]
3. Melgarejo OJ, Torales JC, Cantero JB. Código Z: necesidad de integrar un trabajador social psiquiátrico a la sala de internación del Servicio de Psiquiatría del Hospital de Clínicas. Un estudio piloto. An. Fac. Cien. Méd. (Asunción) 2017;50(3):29-40. 10.18004/anales/2017.050(03)29-040
[ Links ]
4. Sánchez R, Jaramillo LE, Quintero C. Estabilidad del Diagnóstico Psiquiátrico en Pacientes de Consulta Externa. Rev Colomb Psiquiatr. 2002;31(2):101-122.
[ Links ]
5. Kendell RE. The stability of psychiatric diagnosis. Br J Psychiatry. 1974;124(0):352-356. 10.1192/bjp.124.4.352
[ Links ]
6. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington VA: APA Press, 2013.
[ Links ]
7. Muñoz Navarro SR. How many subjects do I need to power my study?. Medwave. 2014;14(6):e5995. 10.5867/medwave.2014.06.5995
[ Links ]
8. Cegla-Schvartzman FB, Ovejero S, López-Castroman J, Baca-García E. Diagnostic Stability in Bipolar Disorder: A Narrative Review. Harv Rev Psychiatry. 2019;27(1):3-14. 10.1097/HRP.0000000000000187
[ Links ]
9. Paris J. Differential Diagnosis of Borderline Personality Disorder. Psychiatr Clin North Am. 2018;41(4):575-582. 10.1016/j.psc.2018.07.001
[ Links ]
10. Rao S, Broadbear J. Borderline personality disorder and depressive disorder. Australas Psychiatry. 2019;27(6):573-577. 10.1177/1039856219878643
[ Links ]
11. Beatson JA, Rao S. Depression and borderline personality disorder. Med J Aust 2013; 199(6):S24-S27. 10.5694/mja12.10474
[ Links ]
12. Kjær JN, Biskin R, Vestergaard C, Gustafsson LN, Munk-Jørgensen P. The clinical trajectory of patients with borderline personality disorder. Personality and Mental Health 2016;10:181-190. 10.1002/pmh.1337
[ Links ]
13. Blázquez A, Ortiz AE, Castro-Fornieles J, Morer A, Baeza I, Martínez E, et al. Five-year diagnostic stability among adolescents in an inpatient psychiatric unit. Comprehensive Psychiatry 2019;89:33-39. 10.1016/j.comppsych.2018.11.011
[ Links ]
14. Ratheesh A, Davey C, Hetrick S, Alvarez-Jimenez M, Voutier C, Bechdolf A, et al. A systematic review and meta-analysis of prospective transition from major depression to bipolar disorder. Acta Psychiatr Scand. 2017;135(4):273-284. 10.1111/acps.12686
[ Links ]
15. Chen MH, Chen YS, Hsu JW, Huang KL, Li CT, Lin WC, et al. Comorbidity of ADHD and subsequent bipolar disorder among adolescents and young adults with major depression: a nationwide longitudinal study. Bipolar Disord. 2015;17(3):315-322. 10.1111/bdi.12266
[ Links ]
16. Bukh JD, Andersen PK, Kessing LV. Rates and predictors of remission, recurrence and conversion to bipolar disorder after the first lifetime episode of depression--a prospective 5-year follow-up study. Psychol Med. 2016;46(6):1151-1161. 10.1017/S0033291715002676
[ Links ]
17. Kessing LV. Diagnostic stability in depressive disorder as according to ICD-10 in clinical practice. Psychopathology. 2005;38(1):32-37. 10.1159/000083968
[ Links ]
18. Schwartz JE, Fennig S, Tanenberg-Karant M, Carlson G, Craig T, Galambos N, et al. Congruence of diagnoses 2 years after a first-admission diagnosis of psychosis. Arch Gen Psychiatry. 2000;57(6):593-600. 10.1001/archpsyc.57.6.593
[ Links ]