INTRODUCTION
Children and adolescents with chronic kidney disease (CKD) often face unique challenges that significantly affect their mental well-being. The stress of ongoing medical treatment, fear of disease progression, and the impact of the disease on daily life and future aspirations can all contribute to these mental health issues. Research has shown that children with CKD experience a lower health-related quality of life (HRQOL) than healthy children, with the severity of CKD linked to further impairment1. Additionally, the psychological impact of CKD on children and adolescents is common and can have significant consequences2.
For example, children and adolescents with CKD often have elevated levels of depressive and anxiety symptoms that extend beyond the patients themselves and affect their parents3,4. Pediatric patients receiving renal replacement therapy have been found to have high rates of depression5. Furthermore, the COVID-19 pandemic has heightened anxiety levels in children with CKD, highlighting their increased vulnerability to external stressors6.
The prevalence of psychiatric diagnoses among children with chronic kidney disease (CKD) is estimated to be between 60 % and 70 % 7,8, with up to 50 % of the children having multiple diagnoses8,9. Stahl et al. have suggested that the main issue with these epidemiological data is that studies on children with CKD have small sample sizes, narrow representations of ethnic groups and geographic areas, and inconsistent definitions of psychiatric disorders, as reflected in the use of various symptom-based screening tools10.
To add to the current body of knowledge on mental health issues in children and adolescents with CKD and given that no prior research has been conducted in the ethnic or geographical context of Paraguay, we conducted an initial exploratory study to assess the mental health status of children and adolescents with CKD receiving care at the Departamento de Nefrología Pediátrica of the Facultad de Ciencias Médicas of the Universidad Nacional de Asunción.
METHODOLOGY
Design and sampling
This descriptive, prospective, cross-sectional, observational study11 was conducted at the Hospital de Clínicas of the Universidad Nacional de Asunción between August and December 2023 to explore the prevalence of mental disorders in children and adolescents diagnosed with CKD. The study sample consisted of all pediatric patients with CKD undergoing treatment at the Departamento de Nefrología Pediátrica of the hospital during the time the study was conducted (n = 28). Therefore, sampling was non-probabilistic for consecutive cases.
Measures
The study was structured around two groups of variables: sociodemographic variables, which included age, sex of the patient, area of residence, marital status, and educational level of the parents; and parental occupation and clinical variables, which focused on age at diagnosis of CKD, underlying pathology, and type of patient (CKD, transplanted, or on renal replacement therapy). The Brief Questionnaire for Screening and Diagnosis (CBTD), adapted from the Rutter's Child Scale, was used to assess mental health issues 12.
CBTD allows for the identification of various mental health problems in children and adolescents, facilitating early and appropriate interventions. The diagnoses assessed were externalizing disorders (impulsivity, attention/hyperactivity deficit disorder, oppositional defiant disorder, and general behavioral problems), internalizing disorders (depression and anxiety), and other syndromes (language problems, epileptic manifestations, and explosive behavior). The results were categorized as “non-cases” (with a score of 4 or fewer symptoms), “probable uncomplicated cases” (with a score of 5 to 8 symptoms), and “definite complicated cases” (with a score of 9 or more symptoms)12.
CBTD exhibits a high level of diagnostic accuracy. In a validation study that examined 530 children, with a cutoff point of 4/5, the measure’s sensitivity was 98.7 % and the positive predictive value was 99.8 %. Although the specificity was relatively low (50 %) due to the limited number of children falling below this threshold, the diagnostic algorithms for conditions such as attention deficit, depression, and conduct disorders showed moderate concurrent validity. The sensitivity ranged from 71 % to 84 %, and the negative predictive value was between 85 % and 97 % for the most general algorithms. These results indicate that CBTD is a valuable tool for identifying psychiatric disorders in highly symptomatic childhood populations12.
Data analysis
The Jamovi program was used for data management and analysis. Descriptive statistics were used in the form of frequency tables to summarize categorical variables and measures of central tendency and the dispersion of numerical variables. Using the CBTD diagnosis interview guidelines, the researchers were able to identify various mental health issues in children and adolescents. They assessed externalizing disorders, which include impulsivity, attention/hyperactivity deficit disorder, oppositional defiant disorder, and general behavioral problems, as well as internalizing disorders such as depression and anxiety. Other syndromes such as language problems, epileptic manifestations, and explosive behavior were also categorized. The results were classified based on the CBTD criteria into "non-cases" (with a score of 4 or fewer symptoms), "probable uncomplicated cases" (with a score of 5 to 8 symptoms), and "definite complicated cases" (with a score of 9 or more symptoms)12.
Ethical considerations
This study was conducted within the framework of the Program of Initiation to Scientific Research of the Network of Student Researchers in Neurosciences, and was approved by the Departmento de Psicología Medica of the Facultad de Ciencias Médicas at the Universidd Nacional de Asunción, Paraguay (Ref. 005-008-2023). The data were treated with confidentiality, equality, and justice, in accordance with the principles of the Helsinki Declaration. Both participants and their parents or guardians provided full written and informed consent to participate in the study.
RESULTS
The study included 28 young individuals (57.1 % males). The age of the participants varied between 2 and 17 years, with a mean of 12.3 ± 4.8 years (median=13 years, IQR=7,25). In total, 42.9 % of the participants were from the countryside and 50 % had parents who were divorced or separated. Additional sociodemographic information is shown in Table 1.
Table 1: Participants’ sociodemographic characteristics (n = 28).
| Characteristics | n | % |
|---|---|---|
| Sex | ||
| Male | 16 | 57.1 |
| Famale | 12 | 42.9 |
| Residence | ||
| Asunción | 3 | 10.7 |
| Greater Asunción | 13 | 46.4 |
| Countryside | 12 | 42.9 |
| Marital Status | ||
| Married | 13 | 46.4 |
| Divorced/separated | 14 | 50 |
| Common-law | 1 | 3.6 |
| Father's Education Level | ||
| Primary | 2 | 7.1 |
| Secondary | 25 | 89.3 |
| Tertiary | 1 | 3.6 |
| Mother's Education Level | ||
| Primary | 1 | 3.6 |
| Secondary | 23 | 82.1 |
| Tertiary | 4 | 14.3 |
| Father's Employment Status | ||
| Employed | 27 | 96.4 |
| Unemployed | 1 | 3.6 |
| Mother's Employment Status | ||
| Employed | 10 | 35.7 |
| Unemployed | 18 | 64.3 |
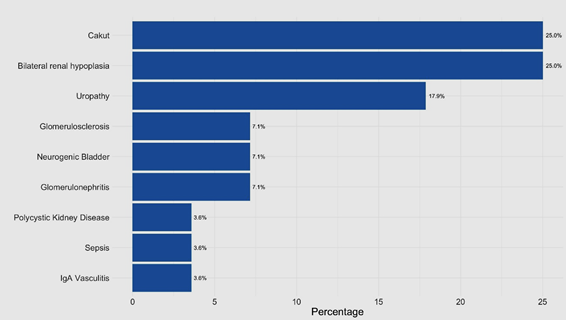
Among the participants, 42.9 % had chronic kidney disease ranging from stage I to III, 17.9 % had reached stage IV, and 39.3 % had undergone kidney transplantation. In terms of diagnosis, congenital anomalies of the kidney and urinary tract (CAKUT) and bilateral renal hypoplasia were the most common, accounting for 25 % of cases (Figure 1).
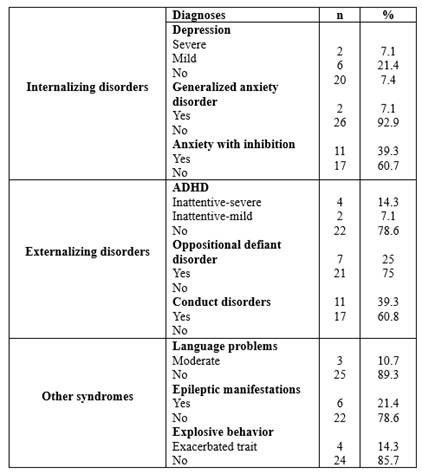
According to CBTD, 39.3 % of the participants were not probable cases of mental disorders. Furthermore, 32.1 % were probable cases without complications, whereas 28.6 % were probable cases with complications. In terms of internalizing disorders, anxiety with inhibition was the most prevalent, accounting for 39.3 % of the cases. Regarding externalizing disorders, conduct disorders were the most frequent, affecting 39.3 % of subjects. Additionally, other syndromes identified included language problems (10.7 %), epileptic manifestations (21.4 %), and explosive behavior as an exacerbated trait (14.3%). The diagnoses are presented in detail in Table 2.
DISCUSSION
This study is the first attempt to explore the prevalence of mental disorders among children and adolescents with CKD in the Paraguayan context. Our findings demonstrate a significant prevalence of both internalizing and externalizing mental health disorders in this vulnerable population, highlighting the complex interplay between chronic physical health conditions and mental health.
The high incidence of internalizing disorders, such as anxiety, found in 39.3 % of participants, parallels findings in other chronic pediatric conditions, suggesting that chronic illness-related stress, uncertainty about the future, and frequent medical interventions are significant contributors to psychological distress13. These findings are concerning, as internalizing disorders can significantly impair a child's ability to fully engage with life, affecting academic performance, social interactions, and the overall quality of life13. The presence of anxiety disorders, particularly inhibition-related anxiety, indicates a potential focus for targeted interventions aimed at improving coping strategies in these patients. Evidence suggests that the higher the CKD stage, the greater the psychological distress in patients, which is attributed to differences in comorbidities, chronic inflammation, oxidative stress, and individual perceptions of health caused by CKD14. However, this was not analyzed because of the limited sample size of our study.
Externalizing disorders such as conduct disorders were observed in 39.3% of the study cohort. This is significant as it suggests behavioral issues that could be responses to the stress associated with chronic illness management and the limitations imposed by the disease. These behaviors may be a child's way of expressing frustration, fear, or the need for control over their life circumstances15. The prevalence of behavioral disorders in children with CKD is a significant concern, as evidenced by a study that found a higher proportion of behavioral and emotional disorders in pediatric patients with CKD than in healthy controls15. This finding is crucial because it suggests that children with CKD may experience a higher burden of behavioral and emotional issues, which could be indicative of the stress associated with chronic illness management and the limitations imposed by the disease. Furthermore, behavioral sleep problems such as bedtime resistance, sleep onset delay, shorter sleep duration, and night awakenings were observed among children with CKD, suggesting that behavioral and psychological factors may contribute to sleep problems in this population16. Addressing these issues through behavioral therapies could help to reduce these symptoms, leading to better social functioning and reduced family stress.
Language problems were found in > 10 % of participants. Research on neurocognitive outcomes in children with CKD has shown the impact of language problems, which can result from factors such as sensorineural hearing loss, medication toxicity, and poor renal function, further emphasizing the multifaceted nature of behavioral issues in children with CKD17.
Notably, the COVID-19 pandemic has added a layer of complexity to the mental health landscape of children with CKD. Our findings suggest that pandemic-related stressors exacerbate existing mental health issues, a phenomenon also observed in broader pediatric populations with chronic diseases6. Furthermore, the influence of chronic illness-related stress, uncertainty about the future, and recurrent medical interventions on the psychological distress of children with CKD was intensified by events such as the COVID-19 pandemic, which not only affected the patients, as indicated by significantly higher levels of anxiety and depression in the guardians of children with CKD than in the control group18. This underscores the importance of integrating pandemic-related psychological support in chronic disease management programs.
Moreover, our study highlights the role of sociodemographic factors in the mental health of children with CKD. The significant number of children from broken homes (50 % having divorced or separated parents) suggests that familial instability may compound the psychological impact of chronic illness. Family dynamics play a crucial role in a child's adaptation to chronic diseases; as such, family centered therapeutic interventions might be beneficial in this context2.
Based on our findings, intervention strategies can be proposed to address the significant mental health challenges identified. First, it is crucial to establish comprehensive psychosocial support programs. These should include regular psychological evaluations and targeted interventions such as cognitive-behavioral therapy to help manage anxiety and conduct disorders19,20. Second, family centered therapeutic interventions could be beneficial, considering the role of family dynamics in a child’s adaptation to chronic diseases. Programs that include family therapy sessions can help improve communication and support within the family, potentially stabilizing a child's emotional and psychological state21. These strategies, grounded in our study’s findings, aim to reduce psychological distress, and improve the mental health and quality of life of children with CKD in Paraguay.
One of the strengths of this study is its pioneering role in addressing an under-researched area within a specific ethnic and geographical population. This study sheds light on the mental health challenges faced by children with CKD in Paraguay and provides a baseline for future investigations and interventions. Additionally, the use of a well-adapted tool for the assessment of mental disorders in children, the Brief Questionnaire for Screening and Diagnosis, enhances the reliability of our findings.
However, our study has some limitations. The small sample size and the cross-sectional design limit the generalizability of the results and prevent the establishment of causality between CKD and mental health outcomes. Furthermore, the study's reliance on a single center for data collection may not accurately reflect the situation in different regions or healthcare settings within the country. Future studies should include larger and more diverse populations and consider longitudinal designs to better understand the trajectories of mental health in this population.
CONCLUSION
In conclusion, our study highlights the substantial burden of mental health disorders in a sample of Paraguayan children and adolescents with CKD and highlights the urgent need for comprehensive, integrated mental health services tailored to the needs of this vulnerable population. The integration of such services could potentially transform the approach to managing CKD in pediatric patients, emphasizing a holistic approach that addresses both physical and psychological health.